Robotic assisted lung resection needs further evidence
Since robotic assisted thoracic surgery (RATS) for lung resection using the “Da Vinci robotic system” has been introduced into the clinical practice of thoracic surgery by Dr. Melfi from Pisa in 2001 and published in 2002 (1), several steps ahead have been done, and the procedure has become more commonly used worldwide. Nevertheless in their article Bao and colleagues conclude “that robotics for lung cancer seems to have higher costs and longer operative time without superior advantage in morbidity rates and oncologic efficiency” (2). In few words, the authors add questions to the already known controversy about the application of RATS for lung resection, and confirm that the use of robotics is not yet based on good evidence of any effect on survival when compared with open surgery or standard video assisted thoracic surgery (VATS). In particular, the observations of Bao et al. (2) are in contrast with those who reported that robotics surgery has several advantages. The proponents of RATS have in fact reasoned that more intuitive movements, greater flexibility and high-definition three-dimensional vision render surgery easier for the surgeon, with shorter learning curve than VATS. Furthermore the proponents affirm that robot-assisted approaches to lung cancer resection and lymph node dissection appear to offer comparable radicality and safety to VATS and open surgery (3-5). Nevertheless it is wise here to remember that many of the proponents of RATS declare relationships with the robotic industries (6).
Nevertheless, although RATS thoracic centers are increasing, a few questions should be posed: is the use of RATS for lung resection justified on the available evidence? Should hospitals invest in robots? Should residency program in thoracic surgery include robotic surgery?
I try briefly to answer.
Is the use of RATS for lung resection justified on the available evidence?
Veronesi et al. in 2010 (7) and Cerfolio et al. in 2011 (8) arrived at the same results. The former performed a comparative study between 38 patients with stage I–II lung cancer operated with RATS vs. 34 patients operated through an open muscle sparing thoracotomy. The latter performed a similar study comparing 106 RATS vs. 318 nerve sparing lobectomy. Both authors concluded that the procedure is practicable, safe, and associated with shorter postoperative hospitalization than open surgery. They also showed that the mean duration of RATS lobectomy was longer than open surgery (2.2 vs. 1.5 hours), and the median numbers of lymph nodes removed were indistinguishable between the robotic and open procedures, suggesting that the robotic approach achieves similar oncological radicality to that achieved by thoracotomy.
Louie et al. (9) have shown that although RATS operative times were longer (median 186 vs. 173 min), all postoperative outcomes were similar, including complications and 30-day mortality (robotic lobectomy, 0.6% vs. VATS, 0.8%; P=0.4). Median length of stay was 4 days for both, but a higher proportion of patients undergoing robotic lobectomy had hospital stays less than 4 days (48% vs. 39%; P<0.001). Nodal upstaging overall was similar (P=0.6) but with trends favoring VATS in the cT1b group and robotic lobectomy in the cT2a group.
A recent publication of Yang HX et al. (10) confirms the results of Park et al. (11) regarding the estimation of survival after robotic lobectomy. Both studies confirm that Robotic lung resections result in similar long-term survival as compared with VATS and thoracotomy. Robot-assisted and VATS procedures are associated with short lengths of stay in hospital, and the robotic procedure in particular results in superior lymph node assessment. These findings suggest that robotic lobectomy for non-small cell lung cancer (NSCLC) affords long-term stage-specific survival consistent with historical results for VATS and thoracotomy.
In short, it is evident that the operation performed via RATS is the same performed by open surgery or VATS, and therefore it would be a surprise to find different long-term survival. Whether more extended lymphadenectomy influences long-term outcome remain uncertain.
Nevertheless, it is interesting to note that few surgeons after initial experience with RATS decided to return to standard VATS resection, as the clinical advantages of the robotic approach were insufficient to justify the greater expense and longer operating times. They showed a Median hospital stay of 11 days (range, 7–53 days), median operating time of 228 min (range, 162–375 min), and one death occurred within 30 days (12).
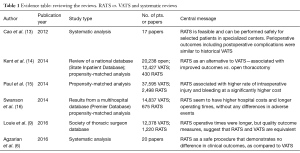
Reviewing the reviews
There aren’t many papers comparing RATS to VATS, and all of them could be found in one of the most recent comprehensive reviews (6). Nonetheless, I made a short review of the reviews with large data or meta-analysis (Table 1), and interestingly the central message is similar to all of them: RATS is feasible and clinical results including quality outcome measures such as hospital stay, 30-day mortality, and nodal upstaging are comparable to standard VATS or thoracotomy. Most authors agree that the robotic approach results in greater lymph node assessment, and this could influence long term survival, which unfortunately has not yet been demonstrated (Table 1).
Full table
Surgeons are always concerned with the risk of intraoperative bleeding for their patients, and bleeding control could be difficult during RATS. Paul et al. (15) demonstrated in their study that specific complications including cardiovascular complications (23.3% vs. 20.0%) and iatrogenic bleeding complications were higher during RATS than VATS (5.0% vs. 2.0%). The higher risk of iatrogenic bleeding complications during RATS persisted in multivariable analyses (adjusted OR, 2.64; 95% CI, 1.58–4.43) (15). However, Cerfolio et al. (17) have recently shown that during robotic anatomic pulmonary resection the incidence of major vascular injury was 2.4% (15 of 632). Of these, 13 patients required thoracotomy performed in a nonurgent manner while the injury was displayed on a monitor, two had the vessel repaired minimally invasively, two required blood transfusion (0.15%), and one patient had 30-day mortality (0.16%). He concluded that major vascular injuries can be safely managed during minimally invasive robotic surgery (17).
Should hospitals continue to invest in robotic thoracic surgery?
Looking the real world, the high capital and running costs, long operating times and operating room usage do not justify such enormous cost. The high cost of the robot is not reasonable for the majority of hospitals especially in rural areas, but recently it has been shown that regional competition could influence the hospital’s decision to acquire a surgical robot to attract more patients (18). Many surgeons and oncologists believe it would be unethical to buy a robot just to attract patients instead of buying it because longer survival is demonstrated. Another big problem is the reported long duration of the operating room usage, which will translate into higher cost. We know that with a good organization in some operating thoracic centers it is possible to perform three major VATS lung resections from 9.00 am to 5.00 pm. This is unlikely to happen with the robot because it is necessary to add the “preparation” time of the operating room. Certainly, in the future when companies will be able to drive down costs, and operating room usage will be similar to standard VATS it could be possible to use more robotic surgery for lung.
Should residency program train juniors thoracic surgeons in robotic surgery?
Residents can participate as the primary surgeons in a variety of thoracic operations during the implementation of a robotics program (19). Operative time, estimated blood loss, and length of stay were similar regardless of level of resident participation (20). As Toker (21) clearly wrote that standardization in surgical education could only be provided through computer-based systems, rather than the classical Halstedian learning systems (see one—do one—teach one), the new generation of surgeon may learn through simulation rather than on patients, and therefore RATS training program will be probably necessary in all surgical school.
The future
Already in the 1970s, NASA suggested to look into the option of remote-controlled robots to operate on astronauts, and we know that it is now possible that long-distance robotic surgery could be used more widely in the earth, allowing people to access world-leading surgeons without having to travel (22). Another more than realistic option is that robots could in the future use algorithms and databases to make decisions during surgery to perform, and finish the operation without human guiding the scalpel. Modern robots combine advanced mechanical, motion and task dexterity features with human-like cognition and intelligence capabilities, and uniportal RATS could become a reality. We could envisage an “octopus” with the head outside the chest and the moving tentacles inside the chest. Certainly the intelligent and autonomous robots offer new opportunities, doubts, law and ethical issues that have to be evaluated and resolved (22).
Nevertheless, because the lack of persuasive level data displaying patient benefit when compared to conventional VATS surgery, in these days, it may be some time before the robot is widely embraced in thoracic surgical practice. In the era of minimal invasiveness, robotic surgery for lung resection deserves a 360° evaluation (including cost, chest pain and long term survival) in a randomized trial vs. the different type of VATS approaches and open lung resection (23-25).
Pragmatically, the fact that RATS did not demonstrated to provide longer survival than VATS or thoracotomy makes it hard to justify buying a robot for lung resection, furthermore the longer duration of the operation and the longer operative room usage and higher cost make the adoption of the robot even more problematic.
Furthermore it is evident that only one operating surgeon is “in charge” in the console, and this might translate in the future to less need for surgeons with elevated surgical skills (26). The next generation of surgeons will decide to operate according to the approach that suits them best (RATS, VATS, single incision, bi-portal or 3-portal technique) and not according to what technology and patients demand.
When a new surgical innovation is introduced into clinical practice, the balance between advantages and disadvantages should be in favor of the advantages for patients and surgeons, and the therapeutic success must be evident. This is not yet the case of robotic assisted lung resection.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by Editor-in-chief Nanshan Zhong (Academician, Chinese Academy of Engineering. Guangzhou Institute of Respiratory Disease, Guangzhou, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Melfi FM, Menconi GF, Mariani AM, et al. Early experience with robotic technology for thoracoscopic surgery. Eur J Cardiothorac Surg 2002;21:864-8. [Crossref] [PubMed]
- Bao F, Zhang C, Yang Y, et al. Comparison of robotic and video-assisted thoracic surgery for lung cancer: a propensity-matched analysis. J Thorac Dis 2016;8:1798-803. [Crossref] [PubMed]
- Veronesi G. Robotic lobectomy and segmentectomy for lung cancer: results and operating technique. J Thorac Dis 2015;7:S122-30. [PubMed]
- Veronesi G. Robotic surgery for the treatment of early-stage lung cancer. Curr Opin Oncol 2013;25:107-14. [Crossref] [PubMed]
- Melfi FM, Mussi A. Robotically assisted lobectomy: learning curve and complications. Thorac Surg Clin 2008;18:289-95. vi-vii. [Crossref] [PubMed]
- Agzarian J, Fahim C, Shargall Y, et al. The Use of Robotic-Assisted Thoracic Surgery for Lung Resection: A Comprehensive Systematic Review. Semin Thorac Cardiovasc Surg 2016;28:182-92. [Crossref] [PubMed]
- Veronesi G, Galetta D, Maisonneuve P, et al. Four-arm robotic lobectomy for the treatment of early-stage lung cancer. J Thorac Cardiovasc Surg 2010;140:19-25. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Skylizard L, et al. Initial consecutive experience of completely portal robotic pulmonary resection with 4 arms. J Thorac Cardiovasc Surg 2011;142:740-6. [Crossref] [PubMed]
- Louie BE, Wilson JL, Kim S, et al. Comparison of Video-Assisted Thoracoscopic Surgery and Robotic Approaches for Clinical Stage I and Stage II Non-Small Cell Lung Cancer Using The Society of Thoracic Surgeons Database. Ann Thorac Surg 2016;102:917-24. [Crossref] [PubMed]
- Yang HX, Woo KM, Sima CS, et al. Long-term Survival Based on the Surgical Approach to Lobectomy For Clinical Stage I Nonsmall Cell Lung Cancer: Comparison of Robotic, Video-assisted Thoracic Surgery, and Thoracotomy Lobectomy. Ann Surg 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Park BJ, Melfi F, Mussi A, et al. Robotic lobectomy for non-small cell lung cancer (NSCLC): long-term oncologic results. J Thorac Cardiovasc Surg 2012;143:383-9. [Crossref] [PubMed]
- Augustin F, Bodner J, Maier H, et al. Robotic-assisted minimally invasive vs. thoracoscopic lung lobectomy: comparison of perioperative results in a learning curve setting. Langenbecks Arch Surg 2013;398:895-901. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. A systematic review and meta-analysis on pulmonary resections by robotic video-assisted thoracic surgery. Ann Cardiothorac Surg 2012;1:3-10. [PubMed]
- Kent M, Wang T, Whyte R, et al. Open, video-assisted thoracic surgery, and robotic lobectomy: review of a national database. Ann Thorac Surg 2014;97:236-42; discussion 242-4. [Crossref] [PubMed]
- Paul S, Jalbert J, Isaacs AJ, et al. Comparative effectiveness of robotic-assisted vs thoracoscopic lobectomy. Chest 2014;146:1505-12. [Crossref] [PubMed]
- Swanson SJ, Miller DL, McKenna RJ Jr, et al. Comparing robot-assisted thoracic surgical lobectomy with conventional video-assisted thoracic surgical lobectomy and wedge resection: results from a multihospital database (Premier). J Thorac Cardiovasc Surg 2014;147:929-37. [Crossref] [PubMed]
- Cerfolio RJ, Bess KM, Wei B, et al. Incidence, Results, and Our Current Intraoperative Technique to Control Major Vascular Injuries During Minimally Invasive Robotic Thoracic Surgery. Ann Thorac Surg 2016;102:394-9. [Crossref] [PubMed]
- Wright JD, Tergas AI, Hou JY, et al. Effect of Regional Hospital Competition and Hospital Financial Status on the Use of Robotic-Assisted Surgery. JAMA Surg 2016;151:612-20. [Crossref] [PubMed]
- White YN, Dedhia P, Bergeron EJ, et al. Resident training in a new robotic thoracic surgery program. J Surg Res 2016;201:219-25. [Crossref] [PubMed]
- Kumar R, Jog A, Vagvolgyi B, et al. Objective measures for longitudinal assessment of robotic surgery training. J Thorac Cardiovasc Surg 2012;143:528-34. [Crossref] [PubMed]
- Toker A. Robotic thoracic surgery: from the perspectives of European chest surgeons. J Thorac Dis 2014;6 Suppl 2:S211-6. [PubMed]
- Tzafestas SG. The World of Robots. In: Tzafestas SG. editor. Roboethics. Springer International Publishing, 2016:35-64.
- Wilson CB. Adoption of new surgical technology. BMJ 2006;332:112-4. [Crossref] [PubMed]
- Paul S, McCulloch P, Sedrakyan A. Robotic surgery: revisiting "no innovation without evaluation". BMJ 2013;346:f1573. [Crossref] [PubMed]
- Migliore M. How surgical care is changing in the technological era. Future Sci OA 2016;2:FSO104.
- Migliore M. Will the widespread use of uniportal surgery influence the need of surgeons? Postgrad Med J 2016;92:240. [Crossref] [PubMed]


