Does 11.5 mm guided single port surgery has clinical advantage than multi-port thoracoscopic surgery in spontaneous pneumothorax?
Introduction
The definition of spontaneous pneumothorax (SP) is air accumulation in the pleural space and is a common disorder in young patients (1). Among multi-factorial causes of SP, the major one is the pleural bleb or bulla, usually located at the lung apex (2). Bullectomy is the most effective treatment which decreases the recurrence rate. Especially, video-assisted thoracoscopic surgery (VATS) has been considered as the first surgical option in SP because of less postoperative pain and early recovery (3). VATS with three-ports is a common practice of surgery for SP, using one port for thoracoscopy, another for lung grasping, and the other, the largest 11.5 or 12 mm port, for stapling devices (4). With increased experience, surgical skills, and advancement of instruments in VATS, single port VATS has been attempted in the field of thoracic surgery (5,6). Although the single port VATS has been expected to have benefits such as lesser postoperative pain and earlier recovery compared to the multi-port VATS, the clinical advantage is still unclear. Using one 2.5 cm incision with a wound protector or the SILS Port™ (Covidien, Norwalk, CT, USA) has been a common fashion for the single port VATS (7,8), and the incision was larger than the biggest incision of multi-port VATS, which made it possible to place several instruments. However, authors believed that the definition of single port VATS is to make the single incision not larger than the maximal port incision in conventional multi-port VATS.
In 2012, we performed the single port VATS using the SILS PortTM or a wound protector, then from 2013, modified the technique using a 11.5 mm single port. We evaluated the clinical benefits in the 11.5 mm single port VATS compared with multi-port VATS for SP.
Methods
This is a retrospective study with Bucheon St. Mary’s Hospital Institutional Review Board approval (HC15RISI0109). Between July 2013 and May 2015, 107 patients underwent wedge resection for SP. The patients with secondary pneumothorax (n=15), open procedure (n=1) and lacking of medical records (n=5) were excluded. A standard three-port VATS was conducted in 46 patients and the single port was performed in 40 patients. The medical records were reviewed including pain, paresthesia, complications and recurrence.
The pain scores were estimated using a visual analog scale (VAS) from 0 to 10. The VAS was checked on the first visit in our hospital, after chest tube insertion, immediately after operation and every 8 hours (hr) until discharge. It was usually recorded during 7–8 AM, 1–2 PM, and 10 PM, by the non-thoracic doctors to avoid any bias derived from attending physicians.
The paresthesia score was evaluated on the first follow-up (F/U) day after discharge. The definition of paresthesia is numbness, tingling or disordered sensation (9). Severity of the paresthesia was categorized according to score (1–3 point: mild; 4–7 point: moderate; 8–10: severe).
All statistical analyses were carried out using SPSS version 18 (SPSS Inc., Chicago, USA). Continuous variables were compared using the Mann-Whitney U test and categorical variables were compared using the Chi-square test and the Fisher exact test.
Surgical technique
Single port VATS
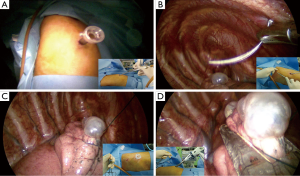
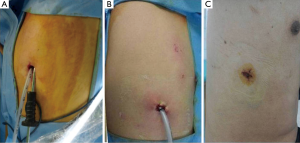
Under general anesthesia with double-lumen endotracheal tube, the patient was changed to the lateral decubitus position. An incision for 11.5 mm port was made on the 5th or 6th intercostal space at the mid-axillary line. If the patient had a chest tube, chest tube incision was used without extending the incision. The 11.5 mm port was placed and a 5 mm thoracoscopy was advanced through the port. The port is then taken out, along the thoracoscopy. Lung is manipulated by using long curved endoscopic instruments and ruptured bulla was identified (Figure 1A). After identification of the bulla, a 1-0 nylon suture was passed through the outside chest wall into the thoracic cavity on the 3rd or 4th intercostal space. The needle was grasped using an endoscopic needle holder under thoracoscopy (Figure 1B). Stay suture was placed at the distal portion of the bulla, then the needle was taken out through the incision (Figure 1C). With gentle retraction of the nylon for lung lifting, wedge resection was performed using endo-staplers (Figure 1D). Absorbable polyglycolic acid sheet (Neoveil, Gunze Ltd, Kyoto, Japan) and fibrin glue were applied on the resection margin after apical pleural abrasion (Figure S1). The operative wound is as same as the wound of chest tube insertion (Figure 2).
Multi-port VATS
Three-port were used for the procedure. An 11.5 mm port was placed on the 7th intercostal space at the mid-axillary line for endo-stapler; 5 mm port was placed on the 7th intercostal space at the anterior axillary line for the right side or at the posterior axillary line for the left side for 5 mm thoracoscopy. Another 5 mm port was made at the subscapular area for the right side or the 4th intercostal space at the anterior axillary line for the left side. Other procedures were same as the previous single port surgery.
All patients were received intravenous patient controlled analgesia (PCA) using fentanyl and oral non-steroidal anti-inflammatory drugs (NSAIDs) for pain control. A chest tube was removed in the absence of air leakage.
Results
The mean age of 86 patients was 22.9±8.5 years old and the mean height and body weight were 174.4±7.1 cm and 60.1±8.5 kg. High resolution computed tomography (HRCT) was performed before operation. Operative indications were: (I) recurrent pneumothorax; (II) previous history of contralateral pneumothorax; (III) hemopneumothorax; (IV) bilateral pneumothorax; (V) prolonged air leakage (>4 days); (VI) visible bullae (>5 mm in diameter) on HRCT despite of the first episode of PSP (10).
Chest tube insertion was performed in 51 patients before operation (59.3%). Preoperatively, the VAS of the patients with chest tube insertion was significant higher compared with the patients without chest tube insertion (mean VAS 4.5±1.7 vs. 2.5±1.3; P<0.001).
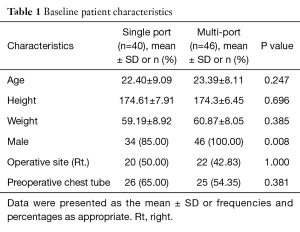
Single port VATS was performed in 40 patients (46.5%). The patients’ characteristics were demonstrated in Table 1 according to the surgical technique (single port vs. three-port VATS). The patient ages were 22.4 years old in the single port group and 23.4 years old in the three-port VATS without difference. The height and weight were not significantly different. Operative site and presence of chest tube before operation were not significantly different between two groups. However, there was significantly more male patient in the group of three-port VATS (P=0.008).
Full table
The mean operation time was 37.25±11.2 minutes (min) in the single port group and 39.02±23.2 min in the three-port VATS group without difference (P=0.204). There was no difference in complications (P=0.595). In the single port group, complications occurred in two patients (5%). In one patient, there was no definite bulla at the time of the operation, and apical stapling and pleural abrasion was performed. Prolonged air leakage was noted after the operation and reoperation was performed. Tiny ruptured bleb was identified on the superior segment of lower lobe. In another patient, wound disruption was developed. In the three-port VATS group, bleeding was developed on postoperative day (POD) 2. About 1 liter of blood has drained without symptoms.
Hospital stay was 3.13±1.8 days in the single port group and 4±1.5 days in the three-port group (P<0.001). Chest tube duration time was 43.85±42.7 hr in the single port group and 57.61±24.4 hr in the three-port VATS group (P<0.001). The paresthesia in the single port group was lower than three-port VATS group (P=0.003) on 1 week after discharge. The grade was mild in all of the patients with paresthesia (Table 2).
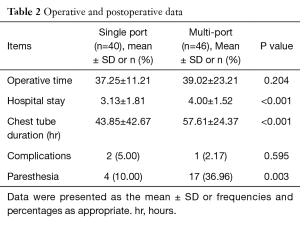
Full table
In VAS score (Figure 3), pre-operative pain score was 4±2.1 in the single port group and 3.4±1.7 in the three-port VATS without difference (P=0.228). The presence of pre-operative chest tube was 26 patients (65%) in the single port group and 25 patients (54.3%) in the three-port VATS group (P=0.381). There was no significant difference in VAS score on the immediate postoperative state, postoperative 8 and 16 hr between two groups. However, VAS score was significantly lower in the single port group after POD 1. The mean VAS score difference was 1.08 between POD 1 and 2. However, chest tube removal was performed before POD 1 in the 13 patients (12 patients in the single port, 1 patient in the three-port VATS) and VAS score was not significantly different at POD 1 after exclusion of these patients (P=0.176). Mean VAS score was 3.46±1.6 in the single port group and 4.16±2.1 in the three-port VATS (Table 3). In VAS score on 1 week after discharge, there was no significant difference between two groups (P=0.200).
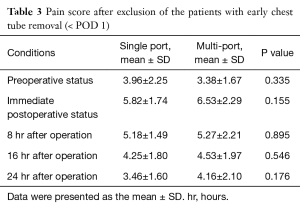
Full table
The mean F/U period was 27±6 months. There were two recurrences in the single port VATS (5%) and four recurrences in the three-port VATS (8.7%) without difference (0.681).
Discussion
VATS is a common procedure in the field of thoracic surgery because of its benefit, less postoperative pain and early recovery, compared with thoracotomy (11). However, chronic postoperative pain still remains high even after thoracoscopic surgery (12). The intercostal nerve injury is known as the main reason for postoperative pain, and the creation of multi-ports in conventional VATS may develop several injuries. In recent years, single port VATS have been attempted in the field of thoracic surgery and since the first report by Yamamoto et al. (13), the safety and feasibility of the single port VATS have been achieved through the numerous literatures (14). Nowadays, adaptation of the single port VATS is extended to the advanced technique of thoracic surgery including bronchoplasty (15). The Single port VATS is expected to reduce postoperative pain compared with the conventional VATS because it involves only one intercostal nerve damage; however, clinical benefit remains unclear. When there is no large randomized and prospective study, there are meta-analyzes about postoperative pain after single port and multiport VATS in the primary SP (16-18). Among those, two meta-analyzes concluded that the single port VATS have shown reduction of pain compared with three-port VATS (16,17), while the other showed that single port VATS had minimal effect of postoperative pain due to heterogeneity, including various surgical techniques and skin incisions (18). Most literatures had 1.5–3 cm skin incisions of single port VATS for minor thoracic surgery (16), and we believe that, the ambiguity of terminology defining the single port (uniportal) VATS caused ununiformed conclusions. In our opinion, single port or uniportal VATS should not have the incision exceeding the maximal length of port incision in conventional VATS. An 11.5 or a 12 mm port is the biggest and essential port for the use of endo-stapler in conventional VATS and that is why we used an 11.5 mm port for the single port VATS. In the 11.5 mm port guided single port VATS, the space is too narrow for several instruments, thus the procedure is less comfortable than multi-port VATS (4). Son et al. described anchoring suture technique for single port VATS wedge resection (8). This technique is similar to our technique but our technique is easier and simpler. Stay suture was performed at the distal portion of bulla using 1-0 nylon and the needle was extracted through the single incision for the lung lifting and retraction.
We investigated the VAS score at the time of pre-operative status because the thoracostomy is a painful procedure. The patients with closed thoracostomy complained for more pain than the patients without closed thoracostomy. However, there was no significant difference in VAS score according to the surgical technique at the time of pre-operative status. The postoperative VAS score found to have significant difference after POD 1; however, the gap of the score between the two groups was only 1 point. Furthermore, this result may contain bias. This result does not consider the chest tube duration time because the placement of chest tube is the factor for pain as described above. In our study, chest tube removal was performed in the 13 patients before POD 1. Twelve patients were in the single port group. After exclusion of these patients, The VAS score was not significantly different between the two groups. Moreover, the VAS score was not different at the 1 week after discharge. Although paresthesia is more common in the multi-port VATS but the grades are mild in all of the patients.
The limitation of our study is small sized retrospective study and heterogeneity of the patients between two groups. The male was more prominent in three-port VATS. It may contain selection bias due to cosmetic effect.
Conclusions
Considering young age without underlying disease in primary SP, the benefit of single port VATS in SP is small. We cautiously suggested that early chest tube removal is the most important for pain reduction, not single port VATS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of Bucheon St. Mary’s Hospital (HC15RISI0109).
References
- Melton LJ 3rd, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis 1979;120:1379-82. [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Waller DA, Forty J, Morritt GN. Video-assisted thoracoscopic surgery versus thoracotomy for spontaneous pneumothorax. Ann Thorac Surg 1994;58:372-6; discussion 376-7. [Crossref] [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [Crossref] [PubMed]
- Lin TS, Kuo SJ, Chou MC. Uniportal endoscopic thoracic sympathectomy for treatment of palmar and axillary hyperhidrosis: analysis of 2000 cases. Neurosurgery 2002;51:S84-7. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Son BS, Kim DH, Lee SK, et al. Small Single-Incision Thoracoscopic Surgery Using an Anchoring Suture in Patients With Primary Spontaneous Pneumothorax: A Safe and Feasible Procedure. Ann Thorac Surg 2015;100:1224-9. [Crossref] [PubMed]
- Sihoe AD, Cheung CS, Lai HK, et al. Incidence of chest wall paresthesia after needlescopic video-assisted thoracic surgery for palmar hyperhidrosis. Eur J Cardiothorac Surg 2005;27:313-9. [Crossref] [PubMed]
- Jeon HW, Kim YD, Kye YK, et al. Air leakage on the postoperative day: powerful factor of postoperative recurrence after thoracoscopic bullectomy. J Thorac Dis 2016;8:93-7. [PubMed]
- Landreneau RJ, Hazelrigg SR, Mack MJ, et al. Postoperative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 1993;56:1285-9. [Crossref] [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [Crossref] [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Xie D, Wang H, Fei K, et al. Single-port video-assisted thoracic surgery in 1063 cases: a single-institution experience†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i31-6. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Qin SL, Huang JB, Yang YL, et al. Uniportal versus three-port video-assisted thoracoscopic surgery for spontaneous pneumothorax: a meta-analysis. J Thorac Dis 2015;7:2274-87. [PubMed]
- Xu W, Wang Y, Song J, et al. One-port video-assisted thoracic surgery versus three-port video-assisted thoracic surgery for primary spontaneous pneumothorax: a meta-analysis. Surg Endosc 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [Crossref] [PubMed]
- Jeon HW, Kim YD. 11.5 mm single port guided VATS bullectomy. Asvide 2016;3:413. Available online: http://www.asvide.com/articles/1185


