A case report of hydatid cysts containing aspergillus
Introduction
Infection by the Aspergillus is usually observed in immunocompromised patients (1) while hydatid disease infected by the tapeworm Echinococcus is endemic in many parts of the world, most ommonly in the Middle East, Australia, Iceland, and South America. The liver and/or lungs are often affected (2). But Aspergillus within a hydatid cyst is extremely rare, and to our knowledge, no more than ten cases have been reported in the English literature. The patients reported mostly were in middle-aged or suffering from other diseases (3-6), the patient in this case is the youngest one ever reported and is immunocompetent. Here, we described the clinical manifestations and possible mechanisms for the co-infection.
Case report
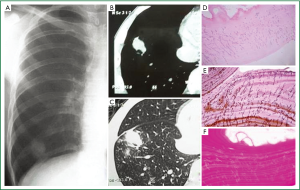
A 15-year-old male presented with cough, hemoptysis and low fever (less 38 °C) of one-month duration. The patient was from Xinjiang, an area of China where hydatid disease is fairly common because people keep domestic animals like sheep and dogs (7). There was no history of pulmonary disease or immunosuppression. A chest radiograph showed an opaque shadow in the low lobe of the right lung. Computerized tomography (CT) scan revealed a solitary pulmonary mass about 2.4 cm × 2.8 cm × 3.2 cm with cavitation in the right lower lobe and an opaque air crescent, suggesting a possible hydatid cyst (Figure 1 A,B,C). Sputum tests for acid fast bacilli, bacteria and fungi, and hydatid hooklets were all negative. Hydatid serology by enzyme linked immunosorbent assay (ELISA) was weakly positive for serum Echinococcal antibodies (IgGs). Results of other laboratory tests such as hemogram, routine urinalysis, stool examination, and tests of liver function did not reveal any abnormalities. The patients was also negative for the human immunodeficiency virus. Abdominal ultrasonography shown no liver lesions. Dyskaryotic cells were found by bronchoscopic brush biopsy.
The patient underwent resection of a lower lobe of the right lung, and a wedge resection specimen was sent for histopathological evaluation. A 4 cm × 4 cm × 4 cm mass, medium hard with a smooth surface, was found in the basal segment containing two intact hydatid cysts. The exocyst was not adhesion the surrounding lung tissue and there was nothing in the innermost layer (ectocyst). Subsequent microscopic examination demonstrated that the ectocyst was acellular and surrounded by lamellated hyaline. On the ectocyst wall, there was a cluster of acute angle branching septate hyphae resembling Aspergillus, confirmed later by Grocott’s methenamine-silver (GMS) and periodic acid-Schiff stain (PAt) (Figure 1D,E,F). Lung tissue around the cyst showed nonspecific chronic inflammation. The patient received oral albendazole (10 mg·kg-1·day-1) as a follow-up treatment.
Discussion
A fully developed hydatid cyst consists of three layers, an inner germinal layer (endocyst), an outer laminated layer (ectocyst) and a host-derived fibrous layer (pericyst). From the germinal layer, scolices, brood capsules, and daughter cysts develop. The clinical manifestation of pulmonary hydatid disease depends on whether the cyst remains intact. Intact cysts remain asymptomatic or cause mild symptoms such as cough, dyspnoea, and chest pain. In addition, patients with a complicated cyst may discharge contents of the cyst, and present with hemoptysis or fever (8). On a chest plain film or CT, intact cysts may display as round or oval masses that possess well-defined borders (9).
In this report, cough, hemoptysis, and fever were the patient’s chief complaints, and a solitary pulmonary mass in the right lung was discovered. The diagnosis of hydatid cyst was made by chest CT, and consistent with serology (serum Echinococcal antibodies). To avoid the risk of anaphylaxis and dissemination, the patient underwent surgery. Two intact cysts were found, but there was nothing in the endocyst, indicating a sterile cyst, which is not the same with previous reports (3-6). Two pathologists confirmed the diagnosis, and the presence of Aspergillus on the wall of the ectocyst was confirmed by microscopic observation, GMS and PAS.
More than 100 species of Aspergillus are known, but only about 20% are pathogenic. The immune state of the patient and structural alterations in lung may predispose to Aspergillus infection. Generally, invasive pulmonary aspergillosis is observed in severely immunocompromised patient, chronic necrotizing aspergillosis in mildly immunocompromised, and aspergilloma in patients with existing lung cavities (10). The most common symptoms are low fever, chronic productive cough, and hemoptysis (11).
Aspergillosis and echinococcosis share the same symptoms and crescent signs on chest CT (2,12), making difficult to distinguish. In this case, the symptoms were not result of hydatid cyst rupture because gross pathology showed the hydatid cysts intact. Even if the cyst were burst, and there was nothing to discharge. So we assume that symptoms of the patient were mainly caused by the Aspergillus infection, but this hypothesis requires further confirmation.
Hydatid cysts containing fungi resembling Aspergillus are extremely rare. At present, such cases have been uncommonly reported, there are no enough data to further study. From 100 archival cases of hydatid disease, Koçer NE et al. found two cases of simultaneous Aspergillus infection, and only in the lung (13). The reason for association remains unclear. Fungal spores can invade through the channels between the airways and cyst and survive in the cyst cavities. Immune deficiencies and structural deformities of lung are predisposing conditions for aspergillosis (1). The patient in this case study was immunocompetent and there was no rupture to form hollow spaces resembling those left after excision of a hydatid cyst. Gupta N et al. (14) proposed that fungi could invade the wall of the ectocyst and breed in the pericyst cavity. It was also suggested that a pressure difference would allow fungal to live in the pericyst cavity (15). The possible reasons we suppose is the resistance of the lung to Asperillus would decline and/or the anatomical structure change when with hydatid infection in lung.
As this co-infection is an incidental finding, a high degree of suspicion is needed to predict the superimposed mycosis. Early diagnosis and trement is important to prevent potential complications stemming from infection by these two pathogens, such as massive hemoptysis. The true mechanisms for this co-infection will be revealed as the number of known cases accumulates, and continued studies will aid in choosing the best treatment options, like surgery to remove the cysts or anti-Aspergillus treatment.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest 2002;121:1988-99.
- Morar R, Feldman C. Pulmonary echinococcosis. Eur Respir J 2003;21:1069-77.
- Rosenheim SH, Schwarz J. Cavitary pulmonary cryptococcosis complicated by aspergilloma. Am Rev Respir Dis 1975;111:549-53.
- Bal A, Bagai M, Mohan H, et al. Aspergilloma in a pulmonary hydatid cyst: a case report. Mycoses 2008;51:357-9.
- Vaideeswar P, Vyas M, Katewa A, et al. Piggyback mycosis: pulmonary hydatid cyst with a mycotic co-infection. Mycoses 2010;53:265-8.
- Koçer NE, Kibar Y, Güldür ME, et al. A retrospective study on the coexistence of hydatid cyst and aspergillosis. Int J Infect Dis 2008;12:248-51.
- Chu XD, Wang GZ, Feng XH, et al. Risk factors on human cystic echinococcosis in HobukesarMongolian Autonomous County in Xinjiang. Zhonghua Liu Xing Bing Xue Za Zhi 2010;31:297-9.
- Kuzucu A, Soysal O, Ozgel M, et al. Complicated hydatid cysts of the lung: clinical and therapeutic issues. Ann Thorac Surg 2004;77:1200-4.
- Brunetti E, Junghanss T. Update on cystic hydatid disease. Curr Opin Infect Dis 2009;22:497-502.
- Zmeili OS, Soubani AO. Pulmonary aspergillosis: a clinical update. QJM 2007;100:317-34.
- Caras WE, Pluss JL. Chronic necrotizing pulmonary aspergillosis: pathologic outcome after itraconazole therapy. Mayo Clin Proc 1996;71:25-30.
- Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest 2002;121:1988-99.
- Koçer NE, Kibar Y, Güldür ME, et al. A retrospective study on the coexistence of hydatid cyst and aspergillosis. Int J Infect Dis 2008;12:248-51.
- Gupta N, Arora J, Nijhawan R, et al. Aspergillosis with pulmonary echinococcosis. Cytojournal 2006;3:7.
- Date A, Zachariah N. Saprophytic mycosis with pulmonary echinococcosis. J Trop Med Hyg 1995;98:416-8.


