The future of off-pump coronary artery bypass grafting: a North American perspective
Introduction
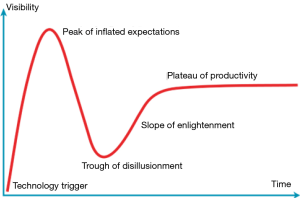
The hype cycle is a conceptual framework used to describe the adoption of emerging technologies. It can be used to illustrate the stages of adoption of off-pump coronary artery bypass graft (OPCAB) (Figure 1) (1). An initial introduction or Technology Trigger was followed by enthusiasm among early adopters and reports of single center experiences that compared favorably with on-pump surgical revascularization. Then a Peak of Inflated Expectations occurred in which OPCAB became widely adopted with continued positive results reported in retrospective and registry series. Subsequently, a Trough of Disillusionment describes the waning of interest as large-scale prospective trials failed to demonstrate mortality benefit and even reports of some inferior long term outcomes. Finally, there was a Slope of Enlightenment with maturing of this technology including the development of adjunctive tools to facilitate off-pump coronary anastomoses. Finally, we are approaching a Plateau of Productivity where we have a more refined understanding of how OPCAB procedures fit into our surgical, interventional and hybrid revascularization armamentarium.
Overview of the OPCAB randomized controlled trial (RCT) literature
In large registry series from the New York State database, Society of Thoracic Surgery (STS) Adult Cardiac Surgical Database (ACSD) and a California-based database, OPCAB has outperformed conventional on-pump CABG (ONCAB) for major outcomes including risk-adjusted operative mortality (2-4). However, such retrospective studies of surgical revascularization are challenged by selection bias, even when propensity matched, and as such, we focus primarily here on prospective data.
Several large-scale RCTs did not demonstrate differences in major adverse cardiovascular and cerebrovascular outcomes (5-7). However, they did consistently show lower ventilation times, ICU stay and transfusion rates with OPCAB and some showed more frequent, incomplete revascularization and reduced long term graft patency. Importantly, there was significant variability in experience with off-pump techniques.
The Randomized On/Off Bypass (ROOBY) trial was the first large-scale multicenter RCT comparing OPCAB vs. on-pump CABG (ONCAB) in Veteran Affairs centers (5). Here, OPCAB was associated with higher composite mortality, myocardial infarction (MI) and repeat revascularization. The major criticisms of this study were the issues of insufficient surgeon experience with OPCAB and the relatively young and healthy male patient population, a subset that one may not expect to benefit greatly from avoidance of cardiopulmonary bypass (CPB). The CABG Off or On Pump Revascularization Study (CORONARY) trial included surgeons with greater experience in OPCAB technique but similarly, did not find differences in primary endpoints of mortality, MI and stroke at 1 year. However, there was a trend towards benefit with OPCAB for higher EuroSCORE patient cohorts (6). Regarding repeat revascularization, there was a trend towards higher incidence with OPCAB in the CORONARY trial. Similarly, in the German Off-Pump CABG in Elderly (GOPCABE) trial, an RCT of patients >75 years (median age 78.5 years) there was no difference in early mortality, stroke or MI between OPCAB and ONCAB (7).
The Surgical Management of Arterial Revascularization Therapies (SMART) trial randomized 200 patients to OPCAB vs. ONCAB by a single, experienced off-pump coronary surgeon (JDP). In this trial, there were no differences in late survival, 1-year graft patency (93.6% for OPCAB vs. 95.8% for ONCAB, P=0.33), recurrent angina or repeat revascularization (8).
Thus, the RCTs suggest that for many patients at low risk for complications from CPB and aortic cross-clamping, ONCAB with fastidious cardioplegia, single aortic clamping and multiple arterial conduits can provide excellent early outcomes and long-term survival. Indeed forgoing completeness or precision of revascularization to perform OPCAB may lead to compromise of longer-term outcomes.
Are there patient subsets that particularly benefit from an off-pump approach?
Retrospective data from specific high-risk subpopulations suggest significant benefit from an OPCAB approach (9-12). These subpopulations may include females (10) and patients in the highest two predicted risk quartiles (3,9). In such patients, improved end-organ perfusion, myocardial protection, limited aortic manipulation and avoidance of systemic inflammation may explain the observed difference in major morbidity and mortality.
What are the theoretical advantages of OPCAB as a state-of-the-art multiple arterial and minimal aortic manipulation procedure?
Off-pump revascularization should be performed as a state-of-the-art technique incorporating multiple arterial grafting and minimal aortic manipulation. Regarding graft choice, it is certainly true that saphenous vein graft (SVG) conduits, with their inevitable attrition, make CABG more vulnerable to need for reintervention. There is strong evidence demonstrating the survival benefit of bilateral ITA (BITA) (13,14) and radial artery grafting (15-17). The Arterial Revascularization Trial of single versus BITA grafting whose primary outcome is 10-year survival will report in 2018, providing high-quality prospective data. The interim 1-year safety end point showed that the use of BITA did not increase mortality or MI in comparison to a single ITA but did lead to a small increase in the risk of sternal wound reconstruction, mostly in obese patients with diabetes (18). In 2009, the Society of Thoracic Surgeons Adult Cardiac Surgery Database reported that only 4.1% of isolated primary CABG cases in North America used BITA grafts and 5.5% used a radial artery graft (19). Notably, the overall proportion of OPCAB increased from 14.5% in 2000 to 21.1% in 2009. This is significantly lower than that reported in European countries who perform multiple arterial grafting in approximately 10–15% of patients, and even more so when compared to rates in Japan (20). We advocate for the use of a greater proportion of arterial grafting for all surgical revascularization, including OPCAB. The increased risk of deep sternal wound infection and the added time necessary for BITA harvest are factors that discourage broader adoption of this technique despite its mortality benefit in CABG patients. It may be necessary and appropriate to provide surgeons with incentive rewards to refine and routinely perform this more technically demanding procedure. Moreover, professional societies, including the STS, should consider BITA grafting/multiple arterial grafting a legitimate quality indicator that should factor into the quality ratings of individual surgeons and surgical centers.
Stroke remains the Achilles’ heel of surgery in trials comparing percutaneous coronary intervention with surgical revascularization, including the SYNTAX and FREEDOM trials (21-23). One advantage of OPCAB is the avoidance of aortic cannulation and CPB which is intuitively attractive for its potential stroke reduction (24,25). In addition, OPCAB uniquely offers the possibility of routinely minimizing or even completely avoiding aortic manipulation, by use of clampless facilitating devices [e.g., HEARTSTRING III (Maquet, Rastatt, Germany)] or utilizing only internal thoracic arterial inflows without aortocoronary anastomoses to further reduce the risk of stroke to levels similar to those reported with multivessel PCI (25-27).
State-of-the-art off-pump surgical revascularization adds several levels of complexity, including the use of complex arterial grafting techniques and proximal anastomosis devices. However, with the use of modern snares and shunts, cardiac positioning devices and coronary stabilizers, proximal anastomosis devices, as well as transit time flow probes, precise coronary anastomoses can be routinely constructed with a minimal-aortic touch technique.
How can we address the technical challenges of OPCAB?
As mentioned, variable surgeon experience may have played a role in the increase in incomplete revascularization, reduction of long term graft patency and need for repeat revascularization in the OPCAB cohorts of some large-scale RCTs. It is our belief that the choice to perform a procedure off-pump should not compromise the completeness of revascularization, except under very unusual circumstances in which CPB is contraindicated or impractical. There is clearly a need to address the technical difficulty of performing OPCAB. As valvular repair, aortic surgery and surgical management of heart failure have become the province of subspecialized teams, so should complex coronary revascularization be performed by dedicated teams that focus on achieving complete revascularization with multiple arterial grafts, minimizing aortic manipulation and advancing the evolving fields of hybrid revascularization and robotic minimally invasive direct coronary artery bypass (MIDCAB). We should move towards a model of reference centers of excellence in which state-of-the-art surgical coronary revascularization will be reliably performed and taught in advanced fellowships.
In this regard, the American Association for Thoracic Surgery sponsored the inaugural International Coronary Congress in 2015 directed by Dr. John Puskas (New York, USA) and Mr. David Taggart (Oxford, UK). This was the first major annual meeting devoted to establishing and disseminating best practices in all types of surgical coronary revascularization. In another example of knowledge dissemination, Dr. Paul Seargent has developed a small private on-line course training program, which is free for all (http://www.opcab-training.eu). It includes a state-of-the-art on-line course with hundreds of hours of high-quality lectures, videos, and theoretical materials. These initiatives and others are helping to increase the overall proficiency of off-pump techniques amongst surgeons world-wide.
The future of OPCAB: what is the role of minimally-invasive and hybrid revascularization?
Off-pump revascularization has facilitated the development of sternal-sparing minimally invasive cardiac surgery (MICS) revascularization procedures. There are several different variations. A small thoracotomy may be used to accomplish LITA harvest and off-pump bypass on the anterior wall under direct vision, known as single vessel small thoracotomy (SVST) or MIDCAB. Multiple grafts may also be performed via mini-thoracotomy; this is known as multivessel small thoracotomy (MVST) (28). Thoracoscopic or robotic-assisted left ITA dissection and harvest can be followed by a direct hand-sewn off-pump anastomosis to the LAD (robotic MIDCAB) or by an endoscopic LITA-LAD anastomosis, known as totally endoscopic CABG (TECAB). Hybrid coronary revascularization (HCR) combines a minimally invasive LITA-to-LAD graft with percutaneous intervention to non-left anterior descending targets (Figure 2) (29-31).
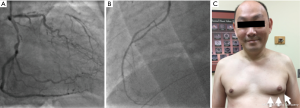
For the small cohort of patients with isolated anterior single vessel disease, a MIDCAB or robotic MIDCAB offers a sternal-sparing incision with the long term patency and survival benefit of the LITA graft. Blazek et al. (32) showed equivalent 7-year survival in 130 patients with single vessel LAD disease randomized to MIDCAB vs. DES-PCI. There was no difference in the composite primary endpoint of all-cause mortality, MI and repeat revascularization but as expected, there was a significantly higher incidence of repeat revascularization with PCI (HR, 13.50; 95% CI: 1.76–103.29; P<0.001). Moreover, a single center propensity score-matched MIDCAB vs. DES-PCI comparison found at 10 years that DES-PCI was associated with a 2.2-fold increased risk of mortality as well as a 2.0-fold increased risk of repeat revascularization (33). Several experienced groups have reported excellent outcomes using a robotic CABG approach (34-36). In their series of direct MVST CABG of which 75% were performed off-pump, Ruel and colleagues (37,38) report excellent graft patency (92% and 100% 6-month graft patency for all grafts and for LITA grafts, respectively).
The concept of HCR stems from the hypothesis that (I) the LIMA-LAD is superior to coronary stenting; and (II) contemporary DES-PCI is non-inferior to saphenous vein bypass grafts used for non-LAD disease. Thus, patients with multivessel disease with a complex LAD lesion and non-complex non-LAD lesions suitable for PCI, HCR may be considered. Currently hybrid revascularization is still limited to select centers where the major clinical outcomes of HCR are equivalent to traditional CABG (33). A meta-analysis of six retrospective studies found that HCR was associated with no difference in freedom from MACCE at 1 year when compared with CABG but a greater incidence of repeat revascularization.
The 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery suggests that HCR is reasonable in patients with (relative) contraindications to traditional CABG, such as heavily calcified proximal aorta or poor target vessels for CABG; lack of conduits; or unfavorable LAD artery for PCI (class IIa, level of evidence B) (39). Furthermore, HCR may be reasonable as an alternative to multivessel PCI or CABG in an attempt to improve the overall risk-benefit ratio (class IIb, level of evidence C). The 2014 European Society of Cardiology/European Association of Cardio-Thoracic Surgery Guidelines on myocardial revascularization suggests HCR for redo revascularization when lack of conduit poses a limitation to a conventional surgical approach (class IIb, level of evidence C).
There are currently no published prospective comparisons of hybrid vs. multivessel PCI. A key question is whether hybrid revascularization is superior to multivessel PCI for patients with low SYNTAX score and proximal LAD disease. The National Institutes of Health has recently agreed to fund a multicenter prospective RCT of HCR vs. multivessel PCI. This trial will enroll more than 2,000 patients in at least 50 centers and follow them for at least 5 years, leveraging the ACC and STS databases for short term and demographic data and centralized data acquisition for longer term endpoints to make this one of the most cost-efficient clinical trials ever conducted in cardiovascular disease.
Conclusions
OPCAB is a highly specialized technique with the potential for reduction of in-hospital morbidity and mortality, particularly in high-risk patient populations. When possible, it should be performed as a clampless technique with multiple- or all-arterial conduits. This is a time-consuming and technically challenging operation that requires dedicated acquisition of individual and team skills beyond those necessary for on-pump LITA-plus-SVG grafting. It is not for every surgical team, nor for every patient. The quality of anastomoses and completeness of revascularization should not be compromised when performing off-pump CABG. With the appropriate use of modern stabilizers and positioning devices as well as surgeon experience and patient selection, equivalent completeness of revascularization and graft patency can be achieved. The major drawback of OPCAB is its greater technical difficulty, requiring judicious navigation of a learning curve for the entire surgical team. By optimizing longevity of graft patency with arterial conduits and minimizing the risk of perioperative stroke by minimizing aortic manipulation, clampless and no-aortic touch OPCAB techniques may be considered the ideal form of surgical coronary revascularization.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wikipedia, the free encyclopedia. Hype cycle. Available online: https://en.wikipedia.org/wiki/Hype_cycle
- Li Z, Yeo KK, Parker JP, et al. Off-pump coronary artery bypass graft surgery in California, 2003 to 2005. Am Heart J 2008;156:1095-102. [Crossref] [PubMed]
- Polomsky M, He X, O'Brien SM, et al. Outcomes of off-pump versus on-pump coronary artery bypass grafting: Impact of preoperative risk. J Thorac Cardiovasc Surg 2013;145:1193-8. [Crossref] [PubMed]
- Hannan EL, Wu C, Smith CR, et al. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation 2007;116:1145-52. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013;368:1189-98. [Crossref] [PubMed]
- Puskas JD, Williams WH, O'Donnell R, et al. Off-pump and on-pump coronary artery bypass grafting are associated with similar graft patency, myocardial ischemia, and freedom from reintervention: long-term follow-up of a randomized trial. Ann Thorac Surg 2011;91:1836-42; discussion 1842-3.
- Puskas JD, Thourani VH, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg 2009;88:1142-7. [Crossref] [PubMed]
- Puskas JD, Edwards FH, Pappas PA, et al. Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg 2007;84:1447-54; discussion 1454-6. [Crossref] [PubMed]
- Keeling WB, Williams ML, Slaughter MS, et al. Off-pump and on-pump coronary revascularization in patients with low ejection fraction: a report from the society of thoracic surgeons national database. Ann Thorac Surg 2013;96:83-8: discussion 88-9.
- Sepehripour AH, Harling L, Ashrafian H, et al. Does off-pump coronary revascularization confer superior organ protection in re-operative coronary artery surgery? A meta-analysis of observational studies. J Cardiothorac Surg 2014;9:115. [Crossref] [PubMed]
- Grau JB, Ferrari G, Mak AW, et al. Propensity matched analysis of bilateral internal mammary artery versus single left internal mammary artery grafting at 17-year follow-up: validation of a contemporary surgical experience. Eur J Cardiothorac Surg 2012;41:770-5; discussion 776. [Crossref] [PubMed]
- Weiss AJ, Zhao S, Tian DH, et al. A meta-analysis comparing bilateral internal mammary artery with left internal mammary artery for coronary artery bypass grafting. Ann Cardiothorac Surg 2013;2:390-400. [PubMed]
- Tranbaugh RF, Dimitrova KR, Friedmann P, et al. Radial artery conduits improve long-term survival after coronary artery bypass grafting. Ann Thorac Surg 2010;90:1165-72. [Crossref] [PubMed]
- Schwann TA, Tranbaugh RF, Dimitrova KR, et al. Time-varying survival benefit of radial artery versus vein grafting: a multiinstitutional analysis. Ann Thorac Surg 2014;97:1328-34; discussion 1334. [Crossref] [PubMed]
- Shi WY, Hayward PA, Fuller JA, et al. Is the radial artery associated with improved survival in older patients undergoing coronary artery bypass grafting? An analysis of a multicentre experience†. Eur J Cardiothorac Surg 2016;49:196-202. [Crossref] [PubMed]
- Taggart DP, Altman DG, Gray AM, et al. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J 2010;31:2470-81. [Crossref] [PubMed]
- ElBardissi AW, Aranki SF, Sheng S, et al. Trends in isolated coronary artery bypass grafting: an analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg 2012;143:273-81. [Crossref] [PubMed]
- Kobayashi J. Current status of coronary artery bypass grafting. Gen Thorac Cardiovasc Surg 2008;56:260-7. [Crossref] [PubMed]
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375-84. [Crossref] [PubMed]
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Puskas JD, Winston AD, Wright CE, et al. Stroke after coronary artery operation: incidence, correlates, outcome, and cost. Ann Thorac Surg 2000.691053-6. [PubMed]
- Bowles BJ, Lee JD, Dang CR, et al. Coronary artery bypass performed without the use of cardiopulmonary bypass is associated with reduced cerebral microemboli and improved clinical results. Chest 2001;119:25-30. [Crossref] [PubMed]
- Cavallaro P, Itagaki S, Seigerman M, et al. Operative mortality and stroke after on-pump vs off-pump surgery in high-risk patients: an analysis of 83,914 coronary bypass operations. Eur J Cardiothorac Surg 2014;45:159-64. [Crossref] [PubMed]
- Kim KB, Kang CH, Chang WI, et al. Off-pump coronary artery bypass with complete avoidance of aortic manipulation. Ann Thorac Surg 2002;74:S1377-82. [Crossref] [PubMed]
- Calafiore AM, Di Mauro M, Teodori G, et al. Impact of aortic manipulation on incidence of cerebrovascular accidents after surgical myocardial revascularization. Ann Thorac Surg 2002;73:1387-93. [Crossref] [PubMed]
- Moss E, Puskas JD, Thourani VH, et al. Avoiding aortic clamping during coronary artery bypass grafting reduces postoperative stroke. J Thorac Cardiovasc Surg 2015;149:175-80. [Crossref] [PubMed]
- Lapierre H, Chan V, Sohmer B, et al. Minimally invasive coronary artery bypass grafting via a small thoracotomy versus off-pump: a case-matched study. Eur J Cardiothorac Surg 2011;40:804-10. [PubMed]
- Vassiliades TA Jr, Douglas JS, Morris DC, et al. Integrated coronary revascularization with drug-eluting stents: immediate and seven-month outcome. J Thorac Cardiovasc Surg 2006;131:956-62. [Crossref] [PubMed]
- Vassiliades TA, Kilgo PD, Douglas JS, et al. Clinical outcomes after hybrid coronary revascularization versus off-pump coronary artery bypass: a prospective evaluation. Innovations (Phila) 2009;4:299-306. [Crossref] [PubMed]
- Blazek S, Rossbach C, Borger MA, et al. Comparison of sirolimus-eluting stenting with minimally invasive bypass surgery for stenosis of the left anterior descending coronary artery: 7-year follow-up of a randomized trial. JACC Cardiovasc Interv 2015;8:30-8. [Crossref] [PubMed]
- Puskas JD, Halkos ME, DeRose JJ, et al. Hybrid Coronary Revascularization for the Treatment of Multivessel Coronary Artery Disease: A Multicenter Observational Study. J Am Coll Cardiol 2016;68:356-65. [Crossref] [PubMed]
- Benedetto U, Raja SG, Soliman RF, et al. Minimally invasive direct coronary artery bypass improves late survival compared with drug-eluting stents in isolated proximal left anterior descending artery disease: a 10-year follow-up, single-center, propensity score analysis. J Thorac Cardiovasc Surg 2014;148:1316-22. [Crossref] [PubMed]
- Halkos ME, Liberman HA, Devireddy C, et al. Early clinical and angiographic outcomes after robotic-assisted coronary artery bypass surgery. J Thorac Cardiovasc Surg 2014;147:179-85. [Crossref] [PubMed]
- Srivastava S, Gadasalli S, Agusala M, et al. Use of bilateral internal thoracic arteries in CABG through lateral thoracotomy with robotic assistance in 150 patients. Ann Thorac Surg 2006;81:800-6; discussion 806. [Crossref] [PubMed]
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013;95:803-12. [Crossref] [PubMed]
- Ruel M, Shariff MA, Lapierre H, et al. Results of the Minimally Invasive Coronary Artery Bypass Grafting Angiographic Patency Study. J Thorac Cardiovasc Surg 2014;147:203-8. [Crossref] [PubMed]
- Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2012;143:4-34. [Crossref] [PubMed]


