We should ban the OPCAB approach in CABG, just as we should ban jetliners and bicycles, or maybe not!
The worldwide implementation of off-pump coronary artery bypass (OPCAB) surgery has failed. But so has the universal implementation of total arterial revascularization, no-touch aorta and so many other possible strategies to improve patient outcomes in coronary artery bypass grafting (CABG). It is said that the cause of the failure in implementation is due to the failure in providing evidence.
Evidence
On 22 January 1952 the first jetliner, the de Havilland DH 106 Comet 1, made its maiden flight from London to Johannesburg. It had four turbojet engines, expedited intercontinental travel with a speed of 805 km/h and offered an incomparable comfort versus the previous flying proposals. It only had to make a single stop in Entebbe. The concept was exciting but the evidence was catastrophic. On 10 January 1954, BOAC flight 781 imploded in flight and a similar event happened on 8 April 1954 with SA 201. The evidence suggested that jetliners were unsafe. Since then jetliners have been abandoned because the evidence was against them!
Karl Friedrich Christian Drais von Sauerbronn presented the first draisienne in 1817 in Mannheim on 12 June 1817 and drove it from the centre of Mannheim to Schwetzingen. It was a wooden two-wheel running velocipede. Immediately women and men got fascinated by the ability to move around at rather “low” cost and rather “high” speed. But bad roads, their lack of riding skills and the absence of appropriate braking systems endangered pedestrians who were unprepared to confront the fast draisiennes. Based on this evidence, authorities in Germany, Great Britain, the USA and even India very correctly banned the velocipedes, ending forever this dangerous form of transportation, due to negative evidence!
Impeding and facilitating factors affecting adoption of technological innovation
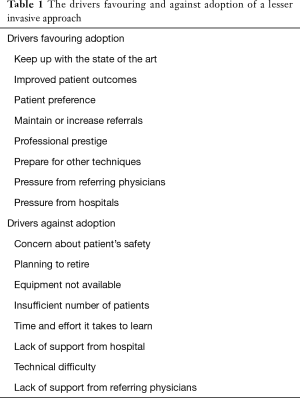
It is possible to give examples of such negative evidence for nearly every possible technological innovation, in or out of medicine. But evidence is only a very secondary component in the adoption of a technology. Pisano (1) studied the organisational differences in rates of learning in the adoption of minimally invasive cardiac surgery between adopters and non-adopters. Evidence was not even mentioned in the top eight drivers facilitating or impeding adoption (Table 1). Most of these drivers address the individual surgeon, few relate to the patient.
Full table
The science of learning has studied these processes in more detail and described several fundamental factors (Table 2) that can be considered impeding and facilitating factors in the adoption of a new technology.

Full table
Perhaps the most important factor in the diffusion of innovations such as lesser invasive surgery in European Health Care systems is the payment system. Without some sort of pressure, people continue to do what they were already doing (2). Technological pull drives often the patient’s expectations and raises them prior to the availability (3) of good efficacy in the long term. A typical example of real world events is the CABG procedure performed on the Japanese emperor using the OPCAB approach. This CABG procedure had the consequence, on itself, of close to excluding the on-pump approach for later patients. A technological pull is a technological imperative that drives physicians to offer the latest technology. This has been identified as a major influence (4) on medical practice in the United States, and is certainly also valid in Europe.
Technology adoption is a complex process of learning how and learning what: this demands a correct understanding (5) of how the distribution of tacit and codified knowledge interacts with performance improvement. But the primary barriers to diffusion of minimally invasive techniques lie within the profession itself. Physicians often cite structural and procedural factors (human and material) but have no insight into their own resistances. Finally, the surgical teams have no insight into the most effective enactment (6). Indeed, shifting back and forth between conventional and a new technology increases the challenge to fall prey to habitual routines and return to the conventional technology. The optimal chance for success is total implementation.
Let the reader not be misled by the introduction, jetliners fly every day and have turned out to be the safest method of travelling. The failures of the Comet 1 plane were first blamed on external factors as the weather but the truth was very different. It had large square windows and metal fatigue that induced the implosions. It was a conceptual problem. The Comet 4, introduced in 1958, had rounded windows and flew for 30 years.
At least a billion bicycles (7) are now on the road and their concept has considerably changed from the first draisiennes. It was also a conceptual problem associated with an operational problem, namely training of the users as well as the pedestrians.
Reasons for failure
Evidence on OPCAB surgery appears very confusing (8-11), however, on the contrary it is not. When the laws of science are applied to most of these manuscripts, the limitations and the consecutive confusion becomes well understood. The data originating from experienced centers appears more convincing compared to those coming from lesser experienced ones. The core issue has been that OPCAB has not been proposed from the beginning as a strict set of rules, procedures and training processes. OPCAB was perceived as a menu wherein components could be chosen and deleted at will, even within the same manuscript and most certainly within meta-analyses. Pressure, suction, friction stabilizers even forks were used to stabilize the anterior wall. This was combined with the unproven dramatic reduction of the level of anticoagulation. The grafted vessel, leading to viable working cardiac muscle, was occluded during the anastomosis without recognizing the consequences of ischemia on a working heart. Neither was there appropriate real-time beat-to-beat monitoring of the possible ischemia, pressure changes, wave form changes or enzymatic evaluation after surgery.
Enucleation of the heart was often more of a strangulation of the heart, in total opposition to physiology. Failure to monitor its consequences on contractility and relaxation supported the continued application of not only ineffective but also deleterious enucleation methods. What happened in the units was often not recorded, neither reported and consequently live procedures turned out to be often catastrophic events, devoid of any educational effort. Consequently, single- as well as multi-center randomized control trials, reviews and meta-analyses were combining different concepts with different levels or absence of safety monitoring, different anticoagulation and stabilization protocols, different levels of training, implementation and experience. It is obvious that evidence generated in such an environment would and always will be confusing.
Fortunately, evidence is not a strong driver in the implementation of a new technology. There are issues emanating from technology itself: the concepts of work are not refined enough, the concepts and conditions of work vary considerably and there is a considerable patient variability. There are similar issues from the side of the scholar impacting evidence in the form of failure to ignore his personal short- and long-term results with older technology, in the ignorance of the basics of outcome analysis with regards to appropriate observation interval, but also the appropriate correction for variability and the power issue.
Learning curves
The mandatory prevalence of learning curves is often cited as the cause of failure of innovation. But learning curves take different shapes.
A first possible shape of the learning curve is the abrupt increase of performance, from day 1, from the previous level up of performance to the new level of performance. This is the optimal implementation but demands massive preparation, organizational processes, simulation and scenario training; possible but a rare reality in the medical profession. The airline industry obtained this learning curve in the Airbus 380 (except for some engine issues) but failed in the Boeing Dreamliner.
A second possible shape shows, from day 1, first a decrease in performance from the previous level, followed sometime later by a gradual increase of performance to a greater than the initial level. This shape of the learning curve is the one most often referred to when learning curves receive a negative connotation. From a medical ethical perspective this shape of learning curve is totally inacceptable, even for the early patients in whom the new procedure is implemented.
An acceptable learning curve for the patient is a third shape with from day 1 a gradual asymptotic increase of performance. The science of learning (12,13) has defined that this curve can only be obtained in the presence of an optimal induced learning (conceptual and simulation) followed by an operational learning process and finalized by autonomous learning.
Induced learning
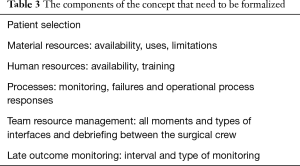
Induced learning has two essential and very active components: conceptual and simulation learning. Conceptual learning mandates the formal creational process, by all the team players, of a concept of work: a very detailed, complete and stepwise description of all components of the concept.
This can be based on existing concepts but needs to be re-created by the team. Table 3 gives an overview of some of the components. The team consists of the five major players in this procedure: anesthesia, surgery, perfusion, nursing and administration. An optimal approach to OPCAB implementation involves also participation of interventional cardiology from the very beginning. Their understanding of changes of surgical strategy will optimize the differential therapy approach for the patient.
Full table
The second part of induced learning is simulation learning. This involves technical skills training as well as scenario training. A surgeon familiar or possibly expert in a certain technique must now acquire expertise in a new technique without any negative impact on any patient. This can only be obtained in simulation. Most surgeons, including myself, use(d) parachuted anastomotic techniques. From a microscopic perspective the effect of parachuting on the vessel wall is similar to the effect of the Gigli saw on the pelvic bone and annihilates all possible benefit of reducing the trauma effect on the vessel wall such as in reducing suture size or reducing the sewing area. In addition, the parachuting technique demands airspace. Airspace is the space between the anastomotic surface and the roof. This is usually not an issue on the anterior wall, but becomes a major one rapidly on the lateral wall, certainly in the presence of hypertrophied ventricles and is even enhanced by incorrect or incomplete enucleating techniques. Coronary artery surgery and therefore obviously OPCAB will benefit considerably from the surgeon learning in simulation and applying anastomotic skills not using the parachuted approach. They have been deconstructed into teachable components and taught to several thousand experienced and lesser experienced surgeons using live and cloud-based simulation courses.
Operational learning
The sustainability of an innovation is embedded in operational learning (14). It starts in OPCAB with the availability of center-specific parameters of on-pump CABG. We repeatedly challenge during proctoring (15) the scholars about their own short- or long-term outcome data. In the absence of own data, it is impossible for them to understand operational learning processes.
We used typical industrial process methods to support operational learning:
- We started by selecting a large cohort of 1,500 of the most recent patients before initiating the OPCAB implementation and all operated by the traditional on-pump approach, standardized for all surgeons. This is essential to ensure quality processing. We excluded the patients undergoing resuscitative cardiac massage or severe cardiogenic shock to reduce the need for complex risk-adjustment;
- We selected a rich dataset of a few hundred preferably continuous preoperative (co-morbidity variables) and some operative variables including the name of the surgeon;
- We selected a rich dataset of well-defined outcome variables including where appropriate the censoring variables. These variables include completeness of revascularization, enzymatic release, stroke, the biased intensive care unit and hospital stay and finally 3-month and late outcome survival and quality-of-life data;
- This step is the data registration of the same morbidity and outcome variables on the OPCAB patients;
- We combined both datasets into one, created a saturated propensity model excluding time variables, created repeatedly separate outcome models for each event after forced inclusion of the propensity model and further search for risk-adjustment. Once no further correction was possible we brought in the OPCAB yes/no variable and identified the effect of this new approach. In this type of approach only the effect of this OPCAB variable is important in the beginning, since there is no power due to the insufficient number of OPCAB records. Varying for each outcome event it became rapidly clear that OPCAB always carried a risk-decreasing sign but it took several hundred or several thousand patients to obtain the strictest evidence for a statistical benefit.
Autonomous learning
Autonomous learning is how the learner then is empowered and interfaces with his data and the ability to take charge of one’s own learning. It is basically the relation of the learner’s psychology to the learning process and evidence (16). A typical example for us was the understanding that our practice of still partially clamping the aorta as in the first 3,000 OPCAB patients could not completely abolish stroke although there was an impact on major reduction of stroke. We also resorted to a higher level of anti-aggregation in the days after surgery, from a preventive level to a therapeutic level.
Conclusions
Implementing a new technology is a science, well studied and described. Translation in science is precisely implementing the progress from one science into the application of another.
More information can be found in a mobile course by going with smartphone to Android or Apple stores and downloading CABG OPCAB by Meplis. Create your own username and password. The use is free for all.
Acknowledgements
None.
Footnote
Conflicts of Interest: P Sergeant has been or is an educational consultant for Medtronic, Maquet and Ethicon.
References
- Pisano GP, Bohmer RM, Edmondson AC. Organisational differences in rates of learning: evidence from the adoption of minimally invasive cardiac surgery. Manage Sci 2001;47:752-68. [Crossref]
- Banta HD, Vondeling H. Diffusion of minimally invasive therapy in Europe. Health Policy 1993;23:125-33. [Crossref] [PubMed]
- Johnson AG. New interventional procedures: efficacy, safety and training. Aust N Z J Surg 1998;68:3-5. [Crossref] [PubMed]
- Barger-Lux MJ, Heaney RP. For better and worse: the technological imperative in health care. Soc Sci Med 1986;22:1313-20. [Crossref] [PubMed]
- Edmondson AC, Winslow AB, Bohmer RM, et al. Learning how and learning what: Effects of tacit and codified knowledge on performance improvement following technology adoption. Decision Sciences 2003;34:197-224. [Crossref]
- Gersick CJ, Hackman JR. Habitual routines in task-performing groups. Organ Behav Hum Decis Process 1990;47:65-97. [Crossref] [PubMed]
- Komanoff C. Bicycling. In: Cleveland CJ. editor. Encyclopedia of Energy. New York: Elsevier, 2004:141-50.
- Sergeant P, Puskas J. Imperitia culpae adnumeratur. Ann Thorac Surg 2013;96:751-4. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Houlind K, Kjeldsen BJ, Madsen SN, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation 2012;125:2431-9. [Crossref] [PubMed]
- Møller CH, Penninga L, Wetterslev J, et al. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev 2012.CD007224. [PubMed]
- Lapré M, Mukherjee AS, Van Wassenhove LN. Behind the learning curve: linking learning activities to waste reduction. Manage Sci 2000;46:597-611. [Crossref]
- Dutton JM, Thomas A. Treating progress functions as a managerial opportunity. Acad Manage Rev 1984;9:235-47.
- Gobran SR, Goldman S, Ferdinand F, et al. Outcomes after usage of a quality initiative program for off-pump coronary artery bypass surgery: a comparison with on-pump surgery. Ann Thorac Surg 2004;78:2015-21; discussion 2021.
- Albert A, Peck EA, Wouters P, et al. Performance analysis of interactive multimodal CME retraining on attitude toward and application of OPCAB. J Thorac Cardiovasc Surg 2006;131:154-62. [Crossref] [PubMed]
- Holec H. Autonomy and Foreign Language learning. Strasbourg: Council of Europe, 1979:1-65.


