Off-pump coronary artery bypass grafting in left main stem stenosis: outcomes, concerns and controversies
Introduction
Left main stem (LMS) coronary artery disease (CAD) was first described as clinical entity in 1912 by Herrick (1). It is known to be an important poor prognostic factor conferring to the morbidity and mortality at the various stages of CAD (2,3). Its incidence nowadays is calculated at around 16–24% (2).
In the past, LMS disease was considered a relative contraindication for off-pump (OFP) coronary artery bypass grafting (CABG) mainly because of the haemodynamic changes occurring with changing the position of the heart during the process of grafting (4). However, emerging number of reports in literature have proven this method as a safe alternative to cardiopulmonary bypass (CPB) (5-7). This review will focus on outcomes, concerns and controversies related to the use of OFP surgery in LMS disease.
Material and methods
A literature review was performed in MEDLINE from period of 1978 to May 2016. We searched for studies including patients with LMS disease undergoing CABG with emphasis on comparison of outcomes between OFP and on-pump (ONP). We reviewed the reference lists of these publications in order to identify all the relevant papers. We included papers published in the English language and listed on MEDLINE and selected the ones which provided the best evidence on the topic. All figures are original and based on data from included in this review studies.
Comments
Outcomes
Numerous studies have shown favourable outcomes with OFP surgery in patients with LMS disease (7-9). Certainly, the uses of stabilizers to steady the heart and intracoronary shunts to permit continued myocardial perfusion during performance of the distal anastomoses have contributed to this. Table 1 summarizes some of the key studies.

Full table
Mortality
Early mortality
Different studies have compared early mortality between OFP and ONP CABG for LMS disease. The rates for OFP range between 0% to 1.8% and for ONP between 2.6% to 5% (Figure 1). The majority of these studies were not able to demonstrate a statistically significant difference (9-12). Freedom from death at 30 days and 1 year has been shown 96.5% and 94.5% for the OFP group and 97.4% and 95.2% for the conventional ONP group, respectively (12).
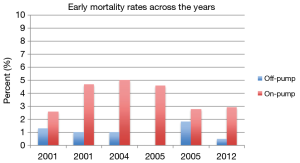
Dewey et al. (5) compared 100 patients who underwent an OFP operation and 723 who had an ONP surgery. Early mortality was not statistically different between the groups; 1% vs. 4.7%, respectively. However, in a logistic regression model adjusting for patient age, obesity, sex, and preoperative hemodynamic instability the use of bypass machine was identified as an independent risk factor for early death with an odds ratio (OR) of 7.3 [95% confidence interval (CI), 1.3–138.4].
Murzi et al. (13) did a propensity matching analysis and ended up with 548 patients in each group with comparable preoperative characteristics. OFP surgery showed an actual benefit as it was associated with lower in-hospital mortality (0.5% vs. 2.9%; P=0.001). However, survival at 1 year was 96.8% in both groups. A multivariable regression analysis revealed the use of CPB was again identified as an independent risk factor for in-hospital morality (OR, 5.74; 95% CI, 1.33–37.24; P=0.001). Other independent predictors included in the model were diabetes and urgency of the operation.
Panesar et al. (8) in their meta-analysis which included nine papers and compared OFP with ONP CABG demonstrated lower incidence of 30-day mortality, while no significant heterogeneity was apparent between the studies. The collective mortality in the OFP was 1% and in the ONP was 3.05%. When studies of high quality were analyzed separately the incidence of early mortality continued to be lower in the OFP (OR, 0.51; 95% CI, 0.23–1.10).
Suzuki et al. (14) compared patients with or without LMS disease and undergoing an OFP surgery. This group demonstrated no difference in the 30-day mortality (P=0.45).
Mid-term mortality
Lu et al. (12) included in their study 2-year mortality data. The crude hazards ratio of 2-year mortality for the OFP was 1.11 (95% CI, 0.64–1.93; P=0.71). After adjusting for the propensity score, the hazards ratio went down to 0.83 (95% CI, 0.45–2.77, P=0.54). Freedom from death at 2 years for the OFP was 93.1% compared to 93.7% for the ONP one. Following adjustment, freedom from death at 2 years for the OFP patients was 94.6% and 93.6% for the ONP patients. Murzi et al. (13) have also demonstrated a comparable 5-year survival of 87.3% for OFP and 88.6% for ONP CABG.
Late mortality
A comparable 10-year survival of 71.7% for OFP and 69.8% for ONP surgery has been demonstrated by Murzi et al. (13). The same groups have identified age, vascular disease and chronic obstructive pulmonary disease as independent predictors of long-term mortality. Strangely, incomplete revascularization was not found a statistically significant predictor (P=0.086).
Suzuki et al. (14) compared patients with or without LMS disease and undergoing an OFP surgery. This group showed that the rates of 6-year freedom from all cause death were 87.3% in the LMS group and 60.7% in the non-LMS group (P=0.17). Multivariate Cox proportional hazards regression analysis showed chronic renal failure as an independent predictor of long-term cardiac events (cardiac death, myocardial infarction, angina pectoris, repeat coronary intervention, and heart failure) with a hazard ratio of 0.3 (95% CI, 0.2–0.6; P=0.001). Hypertension, hyperlipidemia and complete revascularization were not found to be significantly predicting independently the outcome.
Jeong et al. (15) by propensity matching compared OFP CABG with percutaneous coronary intervention (PCI). Overall survival at 8 years was similar between groups; 88.6±3.5% vs. 85.8±5.3%, respectively; P=0.394).
Morbidity
When comparing OFP and ONP surgery for morbidity, the majority of the studies favour the OFP option (9,10,12). Yeatman et al. (9) showed that OFP surgery required less postoperative inotropic support, less temporary pacing, had lower postoperative transfusion requirements and had reduced incidence of postoperative chest infections when compared to the ONP method. The reduced requirement for transfusion of red blood cells in the OFP, despite similar total blood loss was attributed to the greater haemodilution and increased intraoperative blood loss with CPB.
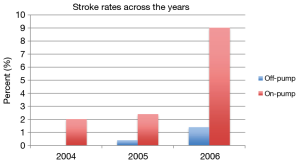
Saba et al. (10) demonstrated that patients operated on with the conventional method had higher levels of peak creatine kinase-myocardial band, blood transfusions, and inotropic requirements, while mechanical ventilation times and hospital stay were longer. The incidence of postoperative atrial fibrillation, mediastinitis, and intra-aortic balloon pump (IABP) use were comparable between the groups. However, the incidence of neurological events was statistically higher with the conventional method.
Lu et al. (12) demonstrated that the requirements for inotropic support were again lower for the OFP patients. Fewer patients in the OFP required prolonged length of stay and a trend was identified to suggest a lower incidence of stroke and chest infection with OFP surgery. Murzi et al. (13) showed again a benefit with OFP surgery as this was associated with lower incidence of stroke, postoperative renal dysfunction, pulmonary complications, and infection.
Virani et al. (11) found no difference in major complications i.e., stroke, myocardial infarction, renal failure, sternal wound infection between OFP and ONP. However, mean hospital length of stay favored the OFP.
In a recent meta-analysis performed by Panesar et al. (8) a difference in the incidence of stroke favoring the OFP (OR, 0.17; 95% CI, 0.05–0.60) was demonstrated. When studies of higher quality were analyzed, the OFP method still emerged as superior to the ONP approach (OR, 0.16; 95% CI, 0.04–0.65). However, for transient ischemic attacks the difference wasn’t statistically significant. Total length of hospital stay, blood loss and inotropic requirements are all significantly more favorable with OFP. All the remaining morbidity outcomes such as atrial fibrillation (AF), acute renal failure, reoperation and myocardial infarction showed just a trend towards favoring OFP surgery. Figure 2 presents a comparison of the stroke rates along the years between OFP and ONP CABG for LMS disease.
Finally, Jeong et al. (15) compared patients having either an OFP surgery or a PCI and demonstrated that freedom from major adverse cardiac and cerebrovascular events (MACCE) was significantly higher in the OFP. This difference was mainly due to a higher risk of acute myocardial infarction and higher rates of target-vessel revascularization in the PCI group.
Graft patency
Previous studies (16,17) have found no difference between the graft patency rates of patients undergoing OFP or ONP surgery. However, the ROOBY trial (18) demonstrated lower 1-year patency rates with the OFP method, although no difference was demonstrated in the patency of internal thoracic anastomoses to left anterior descending artery (LAD) between ONP and OFP method. Various types of grafts have been used in the different series. Left internal thoracic artery (ITA) has been in use frequently for LAD, diagonal and circumflex artery and right ITA for the LAD region but with less frequency (7,19). For revascularization of the right coronary artery territory apart from saphenous veins a right ITA has been used by Jeong et al. when the proximal stenosis was >80% (15). The same group has used an in situ right gastroepiploic artery when the right ITA could not reach the right coronary artery territory. Suzuki et al. (14) have used bilateral ITAs in 69% of patients with LMS disease undergoing OFP surgery. A common combination was in situ grafting of the left ITA to the circumflex area and the right ITA to the LAD. The same group used also skeletonized right gastroepiploic artery for distal right coronary artery.
Unfortunately, detailed data on graft patency for patients with LMS disease is quite limited. Hirose et al. (7) studied 147 patients with LMS undergoing OFP operation. The mean number of bypass grafts was 3.2±1.0, and complete revascularization was performed in 86.4% of the studied population. Postoperative angiography was performed in 66.7% of the patients before discharge from hospital. A total of 249 distal anastomoses were evaluated and the overall patency rate was satisfactory at 97.6% level.
Fukui et al. (19) have shown good results with the use of bilateral skeletonized ITA in OFP surgery. Skeletonization ensured that the right ITA could reach the posterolateral vessels through the transverse sinus. The left and right ITAs were used as grafts for the LAD in 70.5% and in 29.1% of the patients, respectively. The patency rates of the grafts were high both at early angiography and at 1-year angiography. In patients with LMS disease, the patency rates of the ITA grafts were: 98.6% for left ITA and 98.6% for right ITA at early angiography and 97% and 93.2% at 1-year, respectively. Fukushima et al. (20) by performing postoperative angiography in 96.9% of their study population showed comparable patency rates for the arterial grafts (ONP: 100% vs. OFP: 98.3%). However for saphenous vein grafts the difference in patency rates increased (ONP: 93.4% vs. OFP: 76.5%).
Conversion rates
Conversion rate data to ONP are quite limited in LMS disease. Saba et al. (10) had only 1 case out of 100 patients requiring conversion to ONP due to haemodynamic instability (which is the most common reason) without any further adverse outcomes. In two other series the conversion rates were low ranging between 0% and 0.6% (20,21). However, in the series by Lu et al. (12) the conversion rates were higher (3%), but with no justification for this found in their text. Finally, Gan et al. (22) have demonstrated how the incidence of conversion rates increases with the presence of ostial LMS disease. In patients with non-ostial disease it was 1.92% increasing up to 10.26% in the presence of stenosis in the ostium.
Concerns
The optimal treatment for CAD still remains unclear. It is known that advanced CAD which includes as well LMS pathology is associated with uneven cold blood cardioplegia distribution and as a result of this slow and unequal diastolic arrest and delayed recovery of myocardial function when CABG is performed with the conventional way (23). This is mainly because the flow of the cardioplegia is slow through the left coronary in LMS disease having subsequently negative impact on the rate of success of the diastolic arrest and the recovery of the myocardium off-bypass. Apart from that it is known that patients with LMS disease quite often have atheromatous plaques on the aorta and carotid arteries (24) which increase the chances for neurologic deficits postoperatively when a conventional approach with aortic cannulation and cross-clamping is used (25).
In the past OFP CABG although avoiding the aforementioned issues was not widely applied in LMS disease for different reasons. First of all due to the concern for profound haemodynamic disturbances with manipulating the heart and positioning it appropriately for distal coronary anastomoses. This issue is especially prominent in revascularization of the posterior wall (4). Patients with LMS disease and poor collaterals to the right system may not tolerate displacement of the heart for posterior wall grafting with sudden haemodynamic collapse ensuing. Hirose et al. (7) propose in these cases to perform first the left ITA to LAD anastomosis and optimize myocardial flow; displacement of the heart is usually well tolerated after blood supply to the LAD is restored. For ostial LMS the risk is much greater. Gan et al. (22) demonstrated that it does pose an additional risk in OFP surgery in terms of early mortality and MACCEs. The spasm of the ostial LMS lesion during the displacement maneuver often causes severe ischemia in the left coronary artery territory leading to cardiac arrest and emergency conversion to ONP CABG. Truly, the majority of the incidents of mortality and MACCEs in the first 30 postoperative days were attributable to unstable hemodynamics during intraoperative manipulation of the heart for positioning. The incidence of MACCEs was a lot higher in the ostial LMS group when compared to the non-LMS or the non-ostial LMS groups. This group further demonstrated that within the ostial LMS group, the patients who required conversion to ONP had a higher rate of severe LMS stenosis (90%). Therefore, they suggest that 90% or greater stenosis might be a cut-point that could inform the decision of whether to use an IABP during OFP or just start the operation from the beginning on pump.
Suzuki et al. (14) demonstrated that the use of an IABP during OFP surgery was effective in high-risk patients. They commented on the positive effects of this type of support in the reduction of ventricular afterload, improvement of diastolic coronary perfusion, and enhancement of subendocardial perfusion especially when the heart is displaced for grafting. Thus, hemodynamic stability is maintained in these cases with application of an IABP before the operation.
Another concern is on the degree of revascularization with OFP surgery. Most of the studies have shown lower number of grafts off-bypass. Yeatman et al. (9) demonstrated a statistically significant difference in the numbers of grafts performed between OFP and ONP surgery. The ONP received on average 0.5 more grafts per patient when compared to the OFP. This difference was attributed to less extensive CAD and less grafting to the circumflex area in the OFP when compared to the other group. Possibly, the decision was made beforehand in cases of technically difficult circumflex branches requiring grafts to have it done on-bypass. Murzi et al. (13) again showed this difference in practice; the OFP received fewer grafts and had a lower rate of complete revascularization. The same was evident in Virani et al. (11) paper; the average number of grafts was 3.1 in OFP and 4.1 in ONP surgery (P=0.004).
Finally it’s important to mention that fractional flow reserve measurement preoperatively along with real-time graft flow assessment using epigraftic ultrasonography perioperatively is pivotal for assuring long-term patency of the grafts (26,27). Unfortunately, none of these tests are routinely used in everyday practice.
Controversies
The studies included in this review have shown better or at least the same outcomes for OFP surgery of patients with LMS disease (8-10). However, the ROOBY trial involving 2,203 male patients has demonstrated in the whole population (LMS and non-LMS disease) that at 1-year follow-up patients undergoing a beating heart operation experienced worse composite outcomes i.e., mortality, repeat revascularization, or myocardial infarction than did patients in the ONP (28). The rate of graft patency was also significantly lower in the OFP when compared to the ONP (82.6% vs. 87.8%; P<0.01) at 1 year and this accounted for most of the difference in the outcomes between the two groups. However, Dewey et al. (5) has reported that the use of CPB is an independent risk factor for mortality in patients with LMS, with an OR of 7.3.
The SYNTAX trial has shown that in LMS disease an operation is riskier in terms of mortality when compared to coronary stenting especially in patients with lower and intermediate severity scores (29). In contrast, patients with more advanced disease (SYNTAX scores >32) benefit more from an operation with three-fold decrease in the need for repeat revascularization.
Patients in the OFP routinely receive lower number of grafts compared to the ONP approach and even in some studies it is mentioned that the revascularization is incomplete, however the postoperative mortality is equal (10,11) or even favorable (13) when compared to conventional approach. This might indicate that the majority of the patients which had OFP surgery actually had less advanced disease or the incomplete revascularization might have involved less important coronary artery branches to achieve these results. However, Suzuki et al. (14) had similar number of distal anastomoses per patient between OFP and ONP and the complete revascularization achieved was not statistically different between the groups; they didn’t see any difference in the outcomes between the groups as aforementioned previously. In the same context Thomas et al. (30) by comparing patients with or without LMS disease with both groups undergoing an OFP surgery demonstrated no difference in postoperative outcomes i.e., cardiac-related events, neurological deficits, cardiac enzyme course, arrhythmias, blood loss, infections and renal failure although the LMS group had higher EuroScore and more co-morbidities when compared to the other group. They speculated that these favorable outcomes may be attributed to the improved myocardial preservation, reduced reperfusion injury, and absence of the hypothermic insult with avoidance of bypass machine.
OFP surgery in LMS disease is associated in many studies with decrease of the incidence of postoperative neurologic events such as a stroke (8,10,13). However, Calafiore et al. (31) have concluded that the use of side-clamping provides the same risk of stroke as in patients in whom aortic cannulation, bypass machine and cross-clamping were used. A different study has shown that OFP CABG significantly lowers stroke rates compared with conventional ONP surgery irrespective of aortic manipulation (32). This group attributed the neurologic events more on the embolic load caused by the bypass circuit generating micro-gaseous or micro-particulate emboli.
For risk stratification, five different systems have been checked for calibration and discrimination for predicting mortality in OFP surgery (33,34). From them the EuroScore appeared reasonably well calibrated for the highest risk group but not so much for the other groups and its discrimination was moderate (AUC, 0.75; 95% CI, 0.64–0.85) (33). The newer EuroScore II had a satisfactory model fit with a worse discrimination (AUC, 0.706; P=0.0002) (34). Both of them should be checked for this subgroup of patients with LMS disease.
Conclusions
Despite the understandable concerns and controversies OFP surgery has found its place in LMS disease, providing equal or even improved mortality and morbidity outcomes when compared to a conventional approach. Conversion rates are low and graft patency rates comparable to ONP surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Herrick J. Clinical features of sudden obstruction of the coronary arteries. JAMA 1912;59:2015-20. [Crossref] [PubMed]
- Bridgewater B, Neve H, Moat N, et al. Predicting operative risk for coronary artery surgery in the United Kingdom: a comparison of various risk prediction algorithms. Heart 1998;79:350-5. [Crossref] [PubMed]
- Conley MJ, Ely RL, Kisslo J, et al. The prognostic spectrum of left main stenosis. Circulation 1978;57:947-52. [Crossref] [PubMed]
- Watters MP, Ascione R, Ryder IG, et al. Haemodynamic changes during beating heart coronary surgery with the 'Bristol Technique'. Eur J Cardiothorac Surg 2001;19:34-40. [Crossref] [PubMed]
- Dewey TM, Magee MJ, Edgerton JR, et al. Off-pump bypass grafting is safe in patients with left main coronary disease. Ann Thorac Surg 2001;72:788-91; discussion 792. [Crossref] [PubMed]
- Brann S, Martineau R, Cartier R. Left main coronary artery stenosis: early experience with surgical revascularization without cardiopulmonary bypass. J Cardiovasc Surg (Torino) 2000;41:175-9. [PubMed]
- Hirose H. Off-pump coronary artery bypass grafting for patients with left main disease. Cardiology 2004;101:194-8. [Crossref] [PubMed]
- Panesar SS, Chikwe J, Mirza SB, et al. Off-pump coronary artery bypass surgery may reduce the incidence of stroke in patients with significant left main stem disease. Thorac Cardiovasc Surg 2008;56:247-55. [Crossref] [PubMed]
- Yeatman M, Caputo M, Ascione R, et al. Off-pump coronary artery bypass surgery for critical left main stem disease: safety, efficacy and outcome. Eur J Cardiothorac Surg 2001;19:239-44. [Crossref] [PubMed]
- Saba D, Ener S, Bicer M, et al. Off-pump bypass grafting in patients with significant left main coronary artery stenosis. Heart Vessels 2004;19:8-12. [Crossref] [PubMed]
- Virani SS, Lombardi P, Tehrani H, et al. Off-pump coronary artery grafting in patients with left main coronary artery disease. J Card Surg 2005;20:537-41. [Crossref] [PubMed]
- Lu JC, Grayson AD, Pullan DM. On-pump versus off-pump surgical revascularization for left main stem stenosis: risk adjusted outcomes. Ann Thorac Surg 2005;80:136-42. [Crossref] [PubMed]
- Murzi M, Caputo M, Aresu G, et al. On-pump and off-pump coronary artery bypass grafting in patients with left main stem disease: a propensity score analysis. J Thorac Cardiovasc Surg 2012;143:1382-8. [Crossref] [PubMed]
- Suzuki T, Asai T, Matsubayashi K, et al. Left main coronary artery disease does not affect the outcome of off-pump coronary artery bypass grafting. Ann Thorac Surg 2010;90:1501-6. [Crossref] [PubMed]
- Jeong DS, Lee YT, Chung SR, et al. Revascularization in left main coronary artery disease: comparison of off-pump coronary artery bypass grafting vs percutaneous coronary intervention. Eur J Cardiothorac Surg 2013;44:718-24. [Crossref] [PubMed]
- Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004;291:1841-9. [Crossref] [PubMed]
- Nathoe HM, van Dijk D, Jansen EW, et al. A comparison of on-pump and off-pump coronary bypass surgery in low-risk patients. N Engl J Med 2003;348:394-402. [Crossref] [PubMed]
- Hattler B, Messenger JC, Shroyer AL, et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012;125:2827-35. [Crossref] [PubMed]
- Fukui T, Tabata M, Manabe S, et al. Off-pump bilateral internal thoracic artery grafting in patients with left main disease. J Thorac Cardiovasc Surg 2010;140:1040-5. [Crossref] [PubMed]
- Fukushima S, Kobayashi J, Tagusari O, et al. Rationale of off-pump coronary artery bypass grafting for left main trunk disease. Jpn J Thorac Cardiovasc Surg 2004;52:560-6. [Crossref] [PubMed]
- Meharwal ZS, Trehan N. Is off-pump coronary artery bypass surgery safe for left main coronary artery stenosis? Indian Heart J 2001;53:314-8. [PubMed]
- Gan HL, Zhang JQ, Xiao W, et al. Ostial left main coronary artery stenosis as an additional risk factor in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg 2012;143:103-10. [Crossref] [PubMed]
- Noyez L, van Son JA, van der Werf T, et al. Retrograde versus antegrade delivery of cardioplegic solution in myocardial revascularization. A clinical trial in patients with three-vessel coronary artery disease who underwent myocardial revascularization with extensive use of the internal mammary artery. J Thorac Cardiovasc Surg. 1993;105:854-63. [PubMed]
- Doonan AL, Karha J, Carrigan TP, et al. Presence of carotid and peripheral arterial disease in patients with left main disease. Am J Cardiol 2007;100:1087-9. [Crossref] [PubMed]
- Kallikazaros I, Tsioufis C, Sideris S, et al. Carotid artery disease as a marker for the presence of severe coronary artery disease in patients evaluated for chest pain. Stroke 1999;30:1002-7. [Crossref] [PubMed]
- Honda K, Okamura Y, Nishimura Y, et al. Graft flow assessment using a transit time flow meter in fractional flow reserve-guided coronary artery bypass surgery. J Thorac Cardiovasc Surg 2015;149:1622-8. [Crossref] [PubMed]
- Takahashi S, Kuroda M, Orihashi K, et al. Real-time graft flow assessment using epigraftic ultrasonography during coronary artery bypass grafting. Eur J Cardiothorac Surg 2014;46:706-12. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Taggart DP. Lessons learned from the SYNTAX trial for multivessel and left main stem coronary artery disease. Curr Opin Cardiol 2011;26:502-7. [Crossref] [PubMed]
- Thomas GN, Martinez EC, Woitek F, et al. Off-pump coronary bypass grafting is safe and efficient in patients with left main disease and higher EuroScore. Eur J Cardiothorac Surg 2009;36:616-20. [Crossref] [PubMed]
- Calafiore AM, Di Mauro M, Teodori G, et al. Impact of aortic manipulation on incidence of cerebrovascular accidents after surgical myocardial revascularization. Ann Thorac Surg 2002;73:1387-93. [Crossref] [PubMed]
- Patel NC, Deodhar AP, Grayson AD, et al. Neurological outcomes in coronary surgery: independent effect of avoiding cardiopulmonary bypass. Ann Thorac Surg 2002;74:400-5; discussion 405-6. [Crossref] [PubMed]
- Al-Ruzzeh S, Asimakopoulos G, Ambler G, et al. Validation of four different risk stratification systems in patients undergoing off-pump coronary artery bypass surgery: a UK multicentre analysis of 2223 patients. Heart 2003;89:432-5. [Crossref] [PubMed]
- Borde D, Asegaonkar B, Apsingekar P, et al. Risk Stratification in Off-Pump Coronary Artery Bypass (OPCAB) Surgery—Role of EuroSCORE II. J Cardiothorac Vasc Anesth 2015;29:1167-71. [Crossref] [PubMed]


