Is stent insertion via flexible bronchoscopy a feasible alternative to surgery in inoperable thyroid related tracheobronchial stenosis?
Introduction
Central airway obstruction occurs as a consequence of benign or malignant disease. In cases of significant disease, patients often present in significant respiratory distress requiring urgent intervention. While surgical resection with reconstruction is the treatment of choice, many patients are inoperable, too unwell, or have significant co-morbidities that exclude them from this form of therapy. Interventional therapeutic bronchoscopy often with airway stent insertion is an alternative treatment that can have an immediate effect in this cohort of patients.
A number of interventional bronchoscopy techniques exist which facilitate palliation of central airway obstruction. Benign disease is usually managed with airway dilatation with or without laser therapy (1). Malignant disease may be managed with electrocautery, laser vaporisation, brachytherapy, cryotherapy, tumour core-out and photodynamic therapy with or without stent insertion (1). Airway stenting also has a role to play in airway narrowing secondary to extrinsic compression (EC) for example, due to tumour, lymph nodes or goitre (1).
Many different forms of airway stents have been developed, but in general they can be classified in to three groups (I) silicone, (II) metal and (III) hybrid stents (2).
Here, we describe our experience with UltraflexTM self expanding metal stents using flexible bronchoscopy in the management of inoperable thyroid related tracheobronchial stenosis up to the point of the FDA statement on their use in benign disease in 2005.
Materials and methods
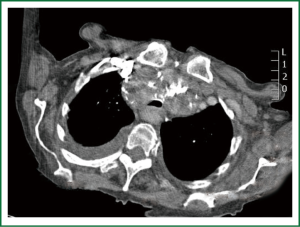
The department of respiratory medicine, Northern General Hospital Sheffield offers a tertiary referral service for the evaluation and management of patients with tracheobronchial stenosis who are not surgical candidates. All patients who had a SEMS inserted for thyroid related tracheobronchial stenosis (Figure 1) in on our department from 1999-2005 were reviewed. The medical notes, procedure sheet and pathology reports of these patients were reviewed to determine the aetiology, location and extent of the airways disease. Early and late outcomes were identified from the patient’s medical notes. Data gathered included patient demographics, clinical presentation, indication for stent, location and size of stent, sedative dose and any complication identified. Patients had at least one follow up bronchoscopy within 6 weeks of stent insertion. After this point, patients were followed indefinitely and underwent bronchoscopy if they had any change in respiratory status. Mean data ± standard deviation (SD) was performed using Graphpad Prism 5 statistical software (La Jolla, CA, USA).
Results
A total of five patients (4 female, 1 male) with a mean age (± SD) of 77.4±17.1 years had UltraflexTM uncovered (uc) stent insertion for thyroid related tracheobronchial stenosis over this period (Table 1). The aetiology included multinodular thyroid goitre (4 patients) and thyroid cancer (1 patient). Stridor was the most common presenting feature (3 patients) followed by dyspnoea (Table 1). EC was the most common finding at bronchoscopy with normal vocal cords in all cases. There was no infiltration seen at any stage. Four patients solely had obstruction of the thoracic trachea and one had obstruction of the left main bronchus (LMB). Stents were successfully inserted at each sitting and one patient required two stents to relieve the stenosis (patient 4). Stridor resolved in all patients post procedure and dyspnoea significantly improved in all patients apart from one who experienced profound hypoxia during the procedure requiring urgent oxygen therapy. Following this period she described significant improvement in symptoms compared to her presentation. There were no complaints of post-operative respiratory symptoms, such as coughing, discomfort, or other evidence of tracheobronchial irritation.

Full Table
Early complications included pneumonia and stent migration in patient 1 and 2 respectively. Late complications were not observed in these patients as both patients died within one year of the procedure; patient 1 from a co-morbid illness and patient 2 from the thyroid malignancy.
Late complications were observed in patients 3-5. These included granulation tissue development at three years and thereafter (requiring regular laser ablation) and stent strut fracture after approximately seven years. Patient 5 declined long term follow up despite our advice. He died 9 years later from cardiac disease.
The mean dose of sedation required was midazolam 2.6±0.7 mg (range, 0-4 mg).
Discussion
In our series we highlight the use of SEMS under sedation with flexible bronchoscopy as a therapy in patients that had inoperable disease and who would otherwise suffocate without intervention. All patients experienced immediately relief of symptoms post procedure in keeping with other studies (3-5) apart from one patient who had a hypoxic episode during the procedure. One patient experienced pneumonia post procedure which responded to antibiotics, while another patient had stent migration (which was repositioned under flexible bronchoscopy). Pneumonia, hypoxia and respiratory arrest have all been described previously in the literature (5-8).
Later complications including granulation tissue development occurred in all patients alive at 3 years. This complication which can lead to stent occlusion if not treated has been previously well described in other studies on tracheobronchial stenosis (3,4,6,7). Indeed Chung and colleagues reported the complication of granulation tissue in 11.2% of SEMS inserted for benign disease in their retrospective study (9). All patients were offered follow up interval bronchoscopy/monitoring but only two patients were regularly bronchoscoped and monitored as two patients died within a year and one patient declined long term follow up until their death nine years after stent insertion. Granulation tissue developed in the three patients that were monitored beyond a year. Patient 3 required laser therapy at year three and subsequently died within the next 12 months from an unrelated illness. Patient 4 required regular laser therapy from year 3 onwards and is still being monitored. This patient also fractured a strut in the metal stent which was detected at year 7 and consideration of stent removal is now underway. Metal fatigue and stent fracture have been previously described and are recognised as one of the major disadvantages of this type of stent (4,5). Fractured stents can be removed or observed in asymptomatic patients (10). Both rigid and flexible bronchoscopic techniques have been used to deal with this complication (10). Chung et al. described a stent fracture rate of 5.2% in their analysis of 72 patients that had SEMS inserted for benign tracheobronchial stenosis of all types (9). Removal of the stent via rigid bronchoscopy is generally required eventually, which in itself is associated with complications such as perforation, haemorrhage and pneumothorax (6,11). Overall, Chung and colleagues demonstrated that 42% of their patients with benign tracheobronchial stenosis experienced some form of complication after SEMS insertion with a median time to complication of 211 days (9). Their data highlights that SEMS are more effective in malignant palliative disease where the patients in general do not survive long enough to develop the significant complications. In the benign group however, the ease of deployment comes with a cost- the SEMS integrate into the airway, resulting in complications such as stent fracture, erosion, mucous retention, and granulation tissue, particularly in those whose life expectancy is not limited by their benign disease and in whom the stents can exist for years.
The use of SEMS for benign disease remains a controversial one with those for and against their use (4,12). In the USA in 2005, the Food and Drug Administration (FDA) recommended that the use of metallic tracheal stents in patients with benign airway disorders should only be used after thoroughly exploring all other treatment options (such as tracheal surgical procedures or placement of silicone stents). The use of metallic tracheal stents as a bridge to other therapies is also not recommended, because removal of these stent can result in serious complications (13). Despite the publishing of this report, there still are no respiratory society guideline recommendations for the use of SEMS in patients with benign central airway stenosis and no randomized controlled trial exist (4,14). Importantly, some centers appear to have continued to insert SEMS for benign disease, a fact that has been attributed to their ease of insertion with flexible bronchoscopy compared with the general anesthesia and rigid bronchoscopy expertise/training required for silicone stent insertion (15). Nonetheless, silicone stents offer significant benefits over SEMS and are the recommended choice for benign tracheobronchial stenosis. Advantages include, less granulation tissue, easier removal at a later date if required, less fractures, less cost, less airway perforation and in general they do not worsen the stenosis. The main disadvantages include the fact that they require rigid bronchoscopy with general anaesthesia for insertion, suffer more bacterial colonisation and migrate more frequently than SEMS (14,15).
The stents in this study were inserted prior to the 2005 recommendation and we concur that the use of SEMS in benign disease is associated with significant complications, the level of which are not experienced in malignancy related stenosis, as in general, these patients have reduced survival times. We also experienced higher complication rates than the studies exploring the use of silicone stents for this condition. Granulation tissue and strut fracture are important complications that arise in this cohort and become a particular problem in those with long survival. Regular follow up is particularly important in patients with SEMS and problems may arise where the patient declines or is unable to attend follow up. Moreover, more bronchoscopies are also required in this group than in those having silicone stents due to the problem with granulation tissue thus exposing the patient to increased procedural risk. Quality of life is also reduced in those who require long term regular bronchoscopic procedures. Our retrospective analysis reveals that our patients had a high complication rate (as they survive longer) when compared to their use in malignant disease or compared to the use of silicone stents in benign disease.
While the lifesaving benefit of SEMS has been described in many benign tracheobronchial stenoses including recently, lung transplantation, herein, we highlight its high complication rate in patients with thyroid related tracheobronchial stenosis who are too unfit for surgery (3,4,6,7,16). We agree that their use in benign disease should only be considered after all other therapeutic options have been explored.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wood DE, Liu YH, Vallières E, et al. Airway stenting for malignant and benign tracheobronchial stenosis. Ann Thorac Surg 2003;76:167-72; discussion 173-4. [PubMed]
- Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J 2006;27:1258-71. [PubMed]
- Madden BP, Datta S, Charokopos N. Experience with Ultraflex expandable metallic stents in the management of endobronchial pathology. Ann Thorac Surg 2002;73:938-44. [PubMed]
- Husain SA, Finch D, Ahmed M, et al. Long-term follow-up of ultraflex metallic stents in benign and malignant central airway obstruction. Ann Thorac Surg 2007;83:1251-6. [PubMed]
- Wilson GE, Walshaw MJ, Hind CR. Treatment of large airway obstruction in lung cancer using expandable metal stents inserted under direct vision via the fibreoptic bronchoscope. Thorax 1996;51:248-52. [PubMed]
- Saad CP, Murthy S, Krizmanich G, et al. Self-expandable metallic airway stents and flexible bronchoscopy: long-term outcomes analysis. Chest 2003;124:1993-9. [PubMed]
- Madden BP, Loke TK, Sheth AC. Do expandable metallic airway stents have a role in the management of patients with benign tracheobronchial disease? Ann Thorac Surg 2006;82:274-8. [PubMed]
- McGrath EE, Warriner D, Anderson P. Is there a beneficial role for a flexible bronchoscopic approach to oesophageal tumour-related tracheobronchial stenosis? Lung 2011;189:401-7. [PubMed]
- Chung FT, Chen HC, Chou CL, et al. An outcome analysis of self-expandable metallic stents in central airway obstruction: a cohort study. J Cardiothorac Surg 2011;6:46. [PubMed]
- Chung FT, Chen GY, Chou CL, et al. Remove airway ultraflex stents by flexible bronchoscope. Am J Med Sci 2012;343:267-72. [PubMed]
- Lunn W, Feller-Kopman D, Wahidi M, et al. Endoscopic removal of metallic airway stents. Chest 2005;127:2106-12. [PubMed]
- Rafanan AL, Mehta AC. Stenting of the tracheobronchial tree. Radiol Clin North Am 2000;38:395-408. [PubMed]
- Food and Drug Administration. FDA public health notification: complications from metallic tracheal stents in patients with benign airway disorders, 2005. Available online: www.fda.gov/cdrh/safety/072905-tracheal.html. Accessed December 05, 2010.
- Lund ME, Force S. Airway stenting for patients with benign airway disease and the Food and Drug Administration advisory: a call for restraint. Chest 2007;132:1107-8. [PubMed]
- Dutau H. Airway stenting for benign tracheal stenosis: what is really behind the choice of the stent? Eur J Cardiothorac Surg 2011;40:924-5. [PubMed]
- Gottlieb J, Fuehner T, Dierich M, et al. Are metallic stents really safe? A long-term analysis in lung transplant recipients. Eur Respir J 2009;34:1417-22. [PubMed]