Postoperative predictors of ipsilateral and contralateral recurrence in patients with primary spontaneous pneumothorax
Introduction
Primary spontaneous pneumothorax (PSP) usually occurs in young, tall, and lean men, especially smokers with no obvious underlying lung disease. It arguably results from rupture of subpleural blebs or bullae. The most frequent complication of PSP is recurrence, which is estimated to occur in 20% to 60% after conservative treatment (1,2). More than 50% of patients with PSP have contralateral blebs/bullae and about a quarter will develop contralateral pneumothorax (3). The British Thoracic Society (BTS) guidelines include first recurrence of contralateral pneumothorax and synchronous bilateral PSP as the only indications for surgery of the contralateral lung (4). However, surgery of the contralateral lung to prevent possible complications remains controversial (5-7). To date, only few studies on small populations have discussed both ipsilateral and contralateral recurrences of PSP. The purpose of our study was to identify the predictors of ipsilateral and contralateral recurrences of PSP and to review literatures on the association of blebs/bullae on high resolution computed tomography (HRCT) of the chest with PSP recurrence. Knowing the risk factors for PSP recurrence may enable us to optimize patient selection to avoid further recurrence and complications.
Methods
PSP patients
From January 2001 to December 2005, 878 patients were treated for pneumothorax at our hospital. Patients who were lost to follow-up or those who had secondary, traumatic, bilateral, or iatrogenic pneumothorax were excluded. Most patients who developed postoperative recurrence were referred back to our institution. For patients who did not develop recurrence or those who were referred to another hospital for recurrence, follow-up information was obtained from the outpatient clinic medical reports. All patients who were included in our study gave informed consent for medical research. This study has been approved by the Institutional Review Board/Ethics Committee of Tri-Service General Hospital (1-105-05-009).
Parameters
The medical records and operative notes of these patients were retrospectively reviewed. Data collected included detailed history, number of pneumothorax episodes and treatment modalities, age, sex, body mass index (BMI) in kg/m2, and smoking habits. According to the suggestion of the World Health Organization, BMI is a simple and widely used method for estimating body fat mass, and underweight was defined as <18.5 kg/m2. Pneumothorax was diagnosed by medical history and chest radiograph; HRCT of the chest was performed in all patients.
Managements for pneumothorax
Depending on the symptoms and radiologic findings, management included high-flow oxygen inhalation therapy, closed tube thoracostomy, and wedge resection by video-assisted thoracoscopic surgery (VATS) with mechanical pleurodesis. We used the Light index, which calculates the volume in cubes of the average lung diameter and the average hemithorax diameter, to quantify the size of the pneumothorax on chest radiographs. A pneumothorax <20% was treated with oxygen inhalation therapy, whereas a pneumothorax >20% was initially managed by closed tube thoracostomy. Indications for wedge resection by VATS included persistent (>4 days) air leak, tension pneumothorax at first presentation, hemopneumothorax, the occupation of the patient (diver, pilot, etc.), and recurrent pneumothorax. Wedge resection was performed using staplers, combined with mechanical pleurodesis with gauze. After surgery, a chest tube (18–20 F) was connected to an underwater seal drainage bottle. Suction (−10 to −20 cm of H2O) was initially applied to the chest drain and was disconnected when air leak has resolved on coughing or Valsalva maneuver. The chest tube was removed after the air leak had stopped for at least 24–48 hours.
Statistical analysis
Descriptive data were expressed as mean ± standard deviation, unless otherwise specified. Student’s t-test was used to analyze continuous variables, whereas chi-square test was used for comparison of categorical variables between groups of ipsilateral recurrence and contralateral recurrence. Probability for recurrent PSP was analyzed by the Kaplan-Meier method. A P value of less than 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 20.0 software (SPSS, Inc., Chicago, IL, USA).
Results
The study group comprised 504 men and 49 women. Among 553 patients with PSP who met the inclusion criteria, the 425 patients who underwent VATS bullectomy were reviewed retrospectively. Of these, 167 patients (43.26%) had recurrent spontaneous pneumothoraces. The patients were followed-up until December 2015; the average follow-up period was 124 months. All blebs/bullae identified on HRCT were localized to the apical segment of the lungs. No other lung anomalies were observed. The clinical demographics of the patients are shown in Table 1. Compared with the non-recurrent group, the recurrent group had similar gender distribution, but significantly differed in patients with smoking history (P=0.011), VATS bullectomy (P<0.001), younger age (P=0.002), and low BMI (P=0.033).
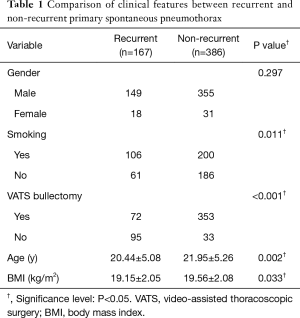
Full table
Univariate analysis of the clinical features affecting PSP recurrence is presented in Table 2. There were 107 (19.35%) patients with ipsilateral recurrence and 84 (15.19%) patients with contralateral recurrence. Compared with the non-recurrent group, the ipsilateral recurrent group had significantly higher proportion of patients with smoking history (P=0.034), VATS bullectomy (P<0.001), and low BMI (P=0.033), but similar gender distribution (P=0.183), HRCT findings of blebs/bullae (P=0.869), and age (P=0.106). Compared with the non-recurrent group, the contralateral recurrent group had significantly higher proportion of patients with no VATS bullectomy (P<0.001), with HRCT findings of blebs/bullae (P<0.001), in younger age (P<0.001), and low BMI (P=0.004), but similar gender distribution (P=0.816) and smoking history (P=0.188). There were 24 patients with bilateral PSP recurrence.
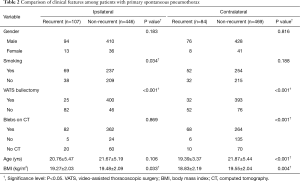
Full table
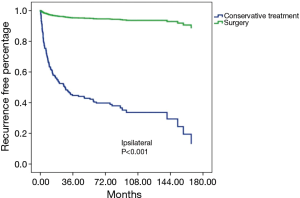
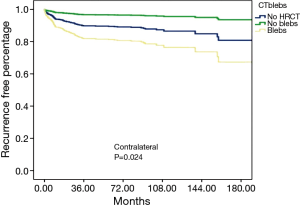
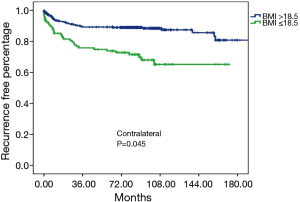
Table 3 shows the results of Cox regression analysis of the factors affecting ipsilateral/contralateral PSP recurrence. Statistically significant predictors were no VATS with bullectomy (OR: 16.629, P<0.001; Figure 1) for ipsilateral PSP recurrence, and presence of blebs/bullae on HRCT (OR: 3.215, P=0.024; Figure 2) and low BMI (OR: 1.560, P=0.045, Figure 3) for contralateral PSP recurrence. Gender and smoking habit were not independent predictors of ipsilateral or contralateral PSP recurrence.
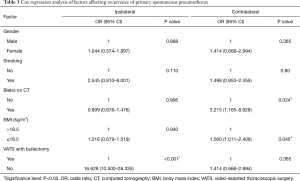
Full table
Discussion
Although not fatal, recurrent pneumothorax is the most common complication after an initial episode of PSP. Moreover, recurrent attacks require readmission to the hospital and additional medical costs. Therefore, identification and documentation of risk factors for recurrence may reduce these additional burdens. Although younger age, male sex, and low BMI were reported as risk factors for recurrence after the first attack of PSP in previous studies (1,5), independent predictors for ipsilateral or contralateral recurrence of PSP are still unclear. There has been no definite agreement on the strategies for prevention of recurrence after the first episode, and preventive surgery for the contralateral lung remains controversial. We hypothesized that the predisposing conditions for ipsilateral or contralateral recurrence might be related to different risk factors because of variant conditions in bilateral lungs. In our study, ipsilateral recurrence was independently associated with no surgical intervention (thoracoscopic bullectomy with mechanical pleurodesis); the key result was that preventive VATS bullectomy for the contralateral lung is suitable only for patients with bullae or blebs on HRCT scan and those who are underweight (BMI <18.5).
A literature review on patients with recurrent PSP revealed that the incidence of blebs/bullae on HRCT scan was 44.83% to 56% in the pediatric population and 47.27% to 78.57% in the adult population (Table 4) (5,6,8-13). Among the pediatric population studies, only the report by Young Choi et al. showed that blebs or bullae on HRCT were significantly related with development of ipsilateral recurrence. In the adult population studies, there were three reports with significance in contralateral PSP recurrence and only one study with significance in both PSP recurrences. After review of existing literature, this study was the only report that divided a PSP recurrence population into ipsilateral (93.87%) and contralateral (70.19%) groups, which were compared in terms of incidence of blebs/bullae on HRCT scan. Our results may be more reliable because of the large number and analysis of the same patient population for predictors of ipsilateral and contralateral recurrence.
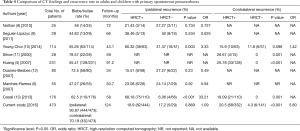
Full table
The role of blebs/bullae as a preexistent lesion for development of PSP has been questioned; in fact, some studies observed no correlation between its presence and the risk for PSP recurrence (6,8,9,11,12,14-17). However, there is some evidence on the lack of association between blebs and different recurrent patterns of PSP (ipsilateral or contralateral). In the previous studies (Table 4), 44.83% to 78.57% of patients with PSP had blebs on HRCT scan; our data showed a distinct distribution between ipsilateral (93.87%) and contralateral (70.19%) blebs. It is important to note that the quality of the CT scan should be assured first prior to considering surgery for prevention of PSP recurrence, especially contralateral recurrence. This will translate to shorter length of hospitalization and reduced need for chest tube drainage.
Prediction of contralateral recurrence is another controversial issue. Some authors suggested that presence of air-containing lesions on the contralateral lung was an independent predictive factor for contralateral pneumothorax and suggested single-stage bilateral VATS for PSP (5,11). On the other hand, Martinez-Ramos et al. showed that there is no association between the presence of bullae on CT scan and recurrence of PSP; therefore, they did not recommend surgery for PSP patients with bullae on CT scan (6). Sahn et al. proposed that the presence of bullae should not guide decision-making on prevention of PSP recurrence (7). Use of low radiation dose CT scan may mitigate the risks of radiation exposure, and lead to benefits outweighing risks (18).
Although somewhat unclear, the pathogenesis of PSP may be due to an imbalance in the development of the lungs and the body (19). Recurrence of PSP is more common at a younger age, because imbalanced development of the lungs and body cannot be corrected by surgery (20). According to the American College of Chest Physicians (21) and BTS guidelines (4), the preferred approach for prevention of recurrent pneumothorax is still surgical because of lower recurrence rates compared with instillation of sclerosing agents through a chest tube. However, the recurrence rate is still high at 5.9% to 24.5%, even after thoracoscopic stapled bullectomy (Table 5) (18,22-27). Therefore, Lee at al. proposed that visceral pleural coverage by cellulose mesh and fibrin glue after thoracoscopic bullectomy was not inferior to mechanical pleurodesis (28). Muramatsu et al. demonstrated a significantly reduced recurrence rate after thoracoscopic bullectomy with fleece-coated fibrin glue (TachoComb) (24).

Full table
Smoking is thought to be important in the pathogenesis of PSP (29). However, its role for the recurrence of PSP is controversial (1,30,31). In our study, smoking was not an independent predictor for ipsilateral or contralateral recurrence of PSP. Interestingly, smoking habit seemed to be significant and only in the ipsilateral recurrence group (Table 2). This might be due to a statistical bias because of the smaller population of smokers.
This study had several limitations, including the retrospective, single-center design. Although the number of patient in this study was the largest to date, there were only 107 cases of ipsilateral PSP recurrence and 84 cases of contralateral PSP recurrence. Therefore, there may have been selection bias, which limited the power of multivariate analysis.
The independent predictor for preventing ipsilateral PSP recurrence was VATS bullectomy. The presence of blebs or bullae in the contralateral lung on HRCT scan and low BMI after an initial episode of PSP may enable us to optimize patient selection for VATS bullectomy to prevent further recurrence and complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board/Ethics Committee of Tri-Service General Hospital (No. 1-105-05-009).
References
- Lippert HL, Lund O, Blegvad S, et al. Independent risk factors for cumulative recurrence rate after first spontaneous pneumothorax. Eur Respir J 1991;4:324-31. [PubMed]
- Sadikot RT, Greene T, Meadows K, et al. Recurrence of primary spontaneous pneumothorax. Thorax 1997;52:805-9. [Crossref] [PubMed]
- Chou SH, Li HP, Lee JY, et al. Is prophylactic treatment of contralateral blebs in patients with primary spontaneous pneumothorax indicated? J Thorac Cardiovasc Surg 2010;139:1241-5. [Crossref] [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Huang TW, Lee SC, Cheng YL, et al. Contralateral recurrence of primary spontaneous pneumothorax. Chest 2007;132:1146-50. [Crossref] [PubMed]
- Martínez-Ramos D, Angel-Yepes V, Escrig-Sos J, et al. Usefulness of computed tomography in determining risk of recurrence after a first episode of primary spontaneous pneumothorax: therapeutic implications. Arch Bronconeumol 2007;43:304-8. [Crossref] [PubMed]
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000;342:868-74. [Crossref] [PubMed]
- Nathan N, Guilbert J, Larroquet M, et al. Efficacy of blebs detection for preventive surgery in children's idiopathic spontaneous pneumothorax. World J Surg 2010;34:185-9. [Crossref] [PubMed]
- Seguier-Lipszyc E, Elizur A, Klin B, et al. Management of primary spontaneous pneumothorax in children. Clin Pediatr (Phila) 2011;50:797-802. [Crossref] [PubMed]
- Young Choi S, Beom Park C, Wha Song S, et al. What factors predict recurrence after an initial episode of primary spontaneous pneumothorax in children? Ann Thorac Cardiovasc Surg 2014;20:961-7. [Crossref] [PubMed]
- Sihoe AD, Yim AP, Lee TW, et al. Can CT scanning be used to select patients with unilateral primary spontaneous pneumothorax for bilateral surgery? Chest 2000;118:380-3. [Crossref] [PubMed]
- Ouanes-Besbes L, Golli M, Knani J, et al. Prediction of recurrent spontaneous pneumothorax: CT scan findings versus management features. Respir Med 2007;101:230-6. [Crossref] [PubMed]
- Casali C, Stefani A, Ligabue G, et al. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg 2013;95:249-55. [Crossref] [PubMed]
- Mitlehner W, Friedrich M, Dissmann W. Value of computer tomography in the detection of bullae and blebs in patients with primary spontaneous pneumothorax. Respiration 1992;59:221-7. [Crossref] [PubMed]
- Noppen M. CT scanning and bilateral surgery for unilateral primary pneumothorax? Chest 2001;119:1293-4. [Crossref] [PubMed]
- Schramel FM, Zanen P. Blebs and/or bullae are of no importance and have no predictive value for recurrences in patients with primary spontaneous pneumothorax. Chest 2001;119:1976-7. [Crossref] [PubMed]
- Smit HJ, Wienk MA, Schreurs AJ, et al. Do bullae indicate a predisposition to recurrent pneumothorax? Br J Radiol 2000;73:356-9. [Crossref] [PubMed]
- Noh D, Lee S, Haam SJ, et al. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg 2015;21:195-9. [Crossref] [PubMed]
- Fujino S, Inoue S, Tezuka N, et al. Physical development of surgically treated patients with primary spontaneous pneumothorax. Chest 1999;116:899-902. [Crossref] [PubMed]
- Huang H, Ji H, Tian H. Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery. Biosci Trends 2015;9:193-7. [Crossref] [PubMed]
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [Crossref] [PubMed]
- Horio H, Nomori H, Kobayashi R, et al. Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 2002;16:630-4. [Crossref] [PubMed]
- Sakamoto K, Takei H, Nishii T, et al. Staple line coverage with absorbable mesh after thoracoscopic bullectomy for spontaneous pneumothorax. Surg Endosc 2004;18:478-81. [Crossref] [PubMed]
- Muramatsu T, Ohmori K, Shimamura M, et al. Staple line reinforcement with fleece-coated fibrin glue (TachoComb) after thoracoscopic bullectomy for the treatment of spontaneous pneumothorax. Surg Today 2007;37:745-9. [Crossref] [PubMed]
- Nakanishi K. Long-term effect of a thoracoscopic stapled bullectomy alone for preventing the recurrence of primary spontaneous pneumothorax. Surg Today 2009;39:553-7. [Crossref] [PubMed]
- Chiu CY, Chen TP, Wang CJ, et al. Factors associated with proceeding to surgical intervention and recurrence of primary spontaneous pneumothorax in adolescent patients. Eur J Pediatr 2014;173:1483-90. [Crossref] [PubMed]
- Chang JM, Lai WW, Yen YT, et al. Apex-to-Cupola Distance Following VATS Predicts Recurrence in Patients With Primary Spontaneous Pneumothorax. Medicine (Baltimore) 2015;94:e1509. [Crossref] [PubMed]
- Lee S, Kim HR, Cho S, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005-11. [Crossref] [PubMed]
- Wallaert B, Gressier B, Marquette CH, et al. Inactivation of alpha 1-proteinase inhibitor by alveolar inflammatory cells from smoking patients with or without emphysema. Am Rev Respir Dis 1993;147:1537-43. [Crossref] [PubMed]
- Cheng YL, Huang TW, Lin CK, et al. The impact of smoking in primary spontaneous pneumothorax. J Thorac Cardiovasc Surg 2009;138:192-5. [Crossref] [PubMed]
- Uramoto H, Shimokawa H, Tanaka F. What factors predict recurrence of a spontaneous pneumothorax? J Cardiothorac Surg 2012;7:112. [Crossref] [PubMed]


