The comparison between novel and traditional three-dimensional image system in thoracoscopy: glasses-less vs. glass
Introduction
As the rapid development of high definition camera and high resolution screen, video-assisted surgeries have been used in the medical centers, especially in thoracoscopy and laparoscopy surgeries (1). Whereas it does not eliminate the limitations of conventional two-dimensional (2D) system including lack of depth of perception and lose of orientation (2). Therefore, three-dimensional (3D) system was introduced to the surgeon for better visualization and precision. It was firstly put into practice in the 1990s. Some studies compared 3D and 2D system in different experiments using ex vivo and in vivo models. The results demonstrated great preference on 3D system (2,3). However, it is neither routinely used nor is the standard equipment in most of the medical centers because of expensive cost. Furthermore, the obscure vision and discomfort side effect including dizziness, ocular fatigue and nausea when wearing the 3D glasses were also the main reasons accounting for its limitation in prevalence.
We have recently developed a “Glasses-less” 3D system for thoracoscopic surgery which allows the operator to conduct a surgical procedure in 3D vision without wearing 3D glasses. The novel glass-less 3D system may provide ideal vision and precision as traditional 3D system. However, no previous study has reported the performance of such novel system. Hence, we intend to compare the glasses-less and normal 3D system on thoracic surgeon in a standardized surgical operation to study the performance of the novel system.
Methods
Volunteers
The First International Course on Tubeless and Advanced VATS Lobectomy Techniques was held on December 7th 2015 in Guangzhou China. A number of 100 lecturers and guests from more than 40 countries and districts had participated in this international course. All of them were thoracic surgeon and anesthesiologists. We invited volunteers who were thoracic surgeon to finish a set of surgical procedures via conventional 3D system and “glass-less” 3D system, respectively. Each volunteer involved in this study had been informed about the questionnaires and the potential publication. The oral consents from the participants had been obtained.
3D system devices
The conventional 3D system consisted of KARL STORZ 3D/HD system and equipped with a 30° of view and 10 mm thoracoscope (Karl Storz, Tuttlingen, Germany) and a pair of 3D glasses. While, the “Glass-less” 3D system was equipped the same light source system, camera and thoracoscope as conventional one with the exception of 3D monitor which was customized by SuperD (SuperD, Shenzhen, China). 3D glasses were not necessary when using the “glass-less” 3D system but a special wireless head band which was a signal generator. A pair of sensors on top of the screen would receive the signal and output 3D vision based on the distant between the screen and operator (Figure 1).
Surgical procedure
The participants were asked to perform six running sutures within 3 cm wound on the standardized rubber models (Figure 2). Before the actual operation, the participants had the opportunity to do some practice runs until they were familiar with the procedures using 2D. One group performed the procedure first with conventional while the other performed the procedure with “Glasses-less” 3D. The participant was then asked to perform the similar procedures again in using the 3D system in a reverse order to what they had done earlier to avoid bias.
Questionnaires
Two questionnaires were given to the participants before and after surgical operations including pre-experienced and post-experienced questionnaires. The details of questionnaires were demonstrated in Tables 1,2.
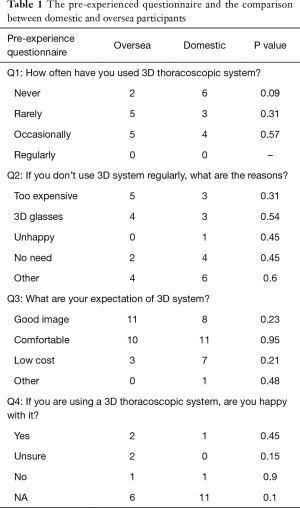
Full table
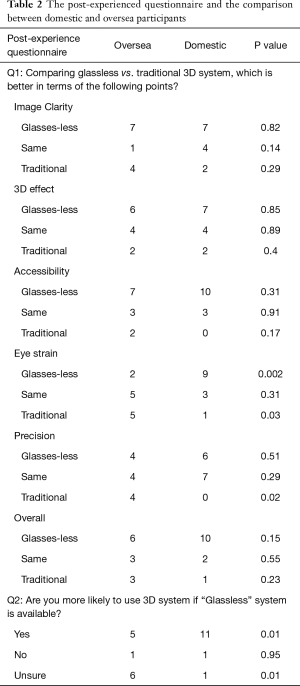
Full table
Statistical analysis
Primary outcome measures recorded were: operation duration and participant questionnaires. The individual operation durations of participants on conventional 3D and Glasses-less 3D were recorded respectively. Paired t-test was utilized to compare the performance of participants on two devices. The difference was considered statistically significant when P<0.05. All tests were two-sided.
Results
A total of 40 volunteers participated in this 3D device experienced activity. Among them, 25 participants had finished the surgical operation on each device and both questionnaires correctly. In the primary cohort, 13 participants were domestic and 12 were from oversea. The median time of the participants working in the thoracic surgery was 20 years ranging from 5 to 30 years.
In the pre-experienced questionnaire, 8 participants had never used a 3D thoracoscopic system. Meanwhile, 8 and 9 of them had rarely and occasionally used 3D thoracoscopic system, respectively. Referring to the reasons for unregularly used 3D system, 8 participants considered it was too expensive and 7 of them disliked the 3D glasses. Six thoracic surgeon considered the 3D system was not necessary. Moreover, 10 of them chose other reasons. Only 1 participant was unhappy about the 3D system. Majority of participants had expectations of 3D system including ideal image, comfortability and less running cost. Nevertheless, most of the participants had no experience on using 3D system, thus they were unsure about the feeling of 3D system utilization or chose not available option (NA) (Table 1).
In the post-experienced questionnaire, we noticed that a large proportion of participants preferred glass-less 3D system rather than the traditional one in terms of image quality (14/25), 3D effect (13/25), accessibility (17/25), comfortability (11/25), and overall evaluation (16/25). However, more participants consider no difference between two devices in the comparison of operating precision (11/25). Eventually, 16 of 25 participants would like to use more 3D system if the glass-less system was available. Meanwhile, 7 and 2 participants chose “No” and “Unsure”, respectively (Table 2).
In the comparison of operation duration, we observed no significant difference between glass-less group and traditional group (mean time: 244.2 vs. 244.8 s, P=0.981). In the sub-groups analysis, neither domestic participants (mean time: 231.4 vs. 243.3 s, P=0.632) nor foreign participants (mean time: 256.1 vs. 246.2 s, P=0.8) had various performance between two devices (Figure 3).

Discussion
A variety of 3D image systems have been developed and put into practice in the latest decades, since the first presentation of 3D stereograph in 1840s. Besides television, movies and other entertainment industries, it has been introduced to the medical field including computed tomography (CT), magnetic resonance imaging (MRI), laparoscopy and thoracoscopy (1,4).
The most significant superiority of 3D image system comparing to the 2D vision was the improved depth perception and spatial orientation (2,3). In order to identify the advantages of 3D image system, numbers of studies had been performed to compare 2D vision to 3D image system in vitro, whereas the results were various. In most of the studies, researchers reported significant better performance in 3D image system including item location and item transfer. However, no difference was observed in some performances such as cutting lines, suturing and knot tying. The reasons accounting for the contradictory results might be the limitations of the first generation 3D image system which were inappropriate frequency of image alteration and insufficiency of image clearance while wearing the 3D glasses.
As the 3D image device development, researchers performed more studies with the novel 3D image device in vivo including pig models and clinical patients (2,3,5,6). They reported that the 3D image quality and the side effect of observers had been significantly improved. After a certain period for 3D device familiarity, more surgeon preferred 3D device other than 2D device for a better accuracy of operation. However, 3D glasses were still required which might cause nausea, dizziness and eyestrains to the operators (5). Moreover, some users complained that they experienced a rim of dimmer vision while wearing the 3D glasses. Along with the high running cost, 3D image systems were only utilized in few departments of some larger medical centers rather than prevailing in most of them even those of academic institutes in the developed countries.
In order to get rid of the influence of wearing 3D glasses, we recently developed a novel 3D image device which was “Glass-free”. Moreover, we conducted a study to compare the performance of novel glasses-free 3D and traditional 3D systems. In the questionnaire section, a larger proportion of participants considered glasses-free 3D system was superior in terms of image quality, 3D effect and accessibility. The main reason accounting for this result might be that 3D glasses were not necessary while using novel 3D system. Therefore, the adverse side effects or experience which were caused by the glasses would be alleviated or even eliminated. In the comparison of surgical process performance, no significant difference was observed which indicated that both devices were able to provide stable and satisfied 3D image. As a result, most of them felt no significant difference between two devices in the question of perception.
However, limitations have to be admitted in glasses-less 3D system. The novel provided 3D image to the operator according to the distance between user and monitor. Therefore, users had to spend a period of time to adjust the system and stand in front of the monitor in a particular range of distance, otherwise the image would become vague. Moreover, the glass-less 3D system was only able to provide satisfied images to the operator solely. As a result, the assistant might have to look at another 3D screen or wear a pair of 3D glasses. Finally, there were only 40 thoracic surgeons had participated in the trial. Therefore, the sample size of the study was insufficient to make a persuasive conclusion. Furthermore, this study was finished via two objective questionnaires which might be lacking of subjective evaluation index.
In summary, our study presented a novel glasses-free image system which could reduce the unpleasant experience and side effects while wearing 3D glasses. Meanwhile, the image quality, 3D effect and accessibility of the novel system might be superior to the traditional system. Referring to perception and surgical performance, no significant difference was observed. However, the novel system had its own limitations which only provide 3D image to one user and required particular operating location. More studies on necessity, feasibility and economic aspect are warranted to identify the advantages and disadvantages of glasses-free 3D system.
Acknowledgements
None.
Footnote
Conflicts of Interest: The Glasses-less three-dimensional thoracoscopy monitor was produced and maintained by SuperD (Shenzhen, China). The authors have no other conflicts of interest to declare.
Ethics Statement: None of patients was involved in our report. Instead, we offered a rubber model of incision for the surgical procedure. Each volunteer involved in this study had been informed about the questionnaires and the potential publication of the study. The oral consents from the participants had been obtained.
References
- Zdichavsky M, Schmidt A, Luithle T, et al. Three-dimensional laparoscopy and thoracoscopy in children and adults: A prospective clinical trial. Minim Invasive Ther Allied Technol 2015;24:154-60. [Crossref] [PubMed]
- Agrusa A, di Buono G, Chianetta D, et al. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: A case-control study. Int J Surg 2016;28 Suppl 1:S114-7. [Crossref] [PubMed]
- Bagan P, De Dominicis F, Hernigou J, et al. Complete thoracoscopic lobectomy for cancer: comparative study of three-dimensional high-definition with two-dimensional high-definition video systems †. Interact Cardiovasc Thorac Surg 2015;20:820-3. [Crossref] [PubMed]
- Lusch A, Bucur PL, Menhadji AD, et al. Evaluation of the impact of three-dimensional vision on laparoscopic performance. J Endourol 2014;28:261-6. [Crossref] [PubMed]
- Hou Y, Guo W, Yang Z, et al. Comparative study of 3D thoracoscopic esophagectomy versus 2D thoracoscopic esophagectomy for esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi 2015;18:889-92. [PubMed]
- Luison F, Boyd WD. Three-dimensional video-assisted thoracoscopic pericardiectomy. Ann Thorac Surg 2000;70:2137-8. [Crossref] [PubMed]




