Effect of changing from the National Health and Nutritional Examination Survey III spirometry reference range to that of the Global Lung Initiative 2012 at Gold Coast Hospital and Health Service
Introduction
Spirometry is a vital tool in the diagnosis and monitoring of respiratory disorders. It is interpreted by comparing measured values to a reference range. Abnormal results are defined as falling outside the lower limits of normal of the reference range. The reference range should ideally approximate as closely as possible to the local population as matched by age, height, sex and ethnicity (1).
The Gold Coast Hospital and Health Service (GCHHS) pulmonary function testing (PFT) laboratories had previously used equations from the National Health and Nutritional Examination Survey III (NHANES III) spirometry dataset to assess individuals aged 18 to 80 years. These equations are based on spirometry results collected in North America between 1988 and 1994 from 2,281 healthy, non-smoking Caucasians aged between 8 and 80 years of age (2). The NHANES III reference equations were chosen for use as they had been drawn from the largest dataset previously available that matched the predominately Caucasian population of Gold Coast, Australia (3).
In 2012 a European Respiratory Society (ERS) task force called the Global Lung Initiative (GLI) released spirometry reference equations that were based on spirometry results collected worldwide from 55,428 healthy, non-smoking Caucasians aged 3 to 95 years (4). The purpose of the new dataset was to provide a continuous spirometry reference range that spanned all ages so as to improve the continuity of diagnosis and care for patients with respiratory disorders. As the GLI 2012 equations were derived from the largest spirometry dataset to date, including data from the NHANES III study, they are likely to be the equations favoured by many lung laboratories.
Since publication of the GLI 2012 spirometry reference equations multiple studies (5-7) have been performed to identify whether changing from the NHANES III to the GLI 2012 equations resulted in a change in diagnosis between obstructive ventilatory defect (OVD), tendency to a restrictive ventilatory defect (TRVD) and normal ventilatory patterns (NVPs). The purpose of this study was to determine if transitioning from the NHANES III to the GLI 2012 equations at the GCHHS PFT laboratories resulted in a change of diagnosis for the individuals tested.
Methods
Spirometry data were collected from patients undergoing investigation at the GCHHS PFT laboratories throughout February and March 2014. These data were then analysed using the NHANES III and GLI 2012 equations to determine a diagnosis of OVD, TRVD or NVP. The results were then evaluated to determine if a change in an individual’s diagnosis had occurred when transitioning between equations. This study was approved by the GCHHS Human Research Ethics Committee (HREC/14/QGC/35).
All patients between the ages of 18 and 80 years who underwent spirometry testing at GCHHS PFT laboratories in the given time period were included in the analysis. Sensormedics VMAX testing software available at the GCHHS PFT laboratories was used to generate predicted spirometry values from the NHANES dataset. Software available on the Spirexpert website (6,8) was used to generate predicted spirometry values from the GLI 2012 dataset.
OVD was defined as a forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) < lower limit of normal (LLN). TRVD was defined as FEV1/FVC ≥ LLN, FEV1 < LLN, and FVC < LLN. Mixed ventilatory defect (MVD) pattern was defined as FEV1/FVC < LLN, FEV1 < LLN, and FVC < LLN. Severity of OVD and TRVD was graded using the American Thoracic Society (ATS) and ERS 2005 guidelines (1). Severity of OVD was defined as the percentage of predicted FEV1: mild >70%, moderate 60–69%, moderately severe 50–59%, severe 35–49% and very severe <35%. Severity of TRVD was defined as the percentage of predicted FVC: mild >70%, moderate 50–70% and severe <50%.
Results
A total of 349 patients were investigated at the GCHHS PFT laboratories throughout February and March 2014. Individuals were excluded if they were >80 years of age (n=19) or <18 years of age (n=25). Test results where patients were not fully able to complete the assessment were also excluded (n=4). The total number of patients included in the final analysis was 301 comprised of 158 males and 143 females.
When the NHANES III equations were applied to the spirometry data from the 301 individuals included in the study the number diagnosed with each ventilatory pattern was: 102 (34%) with a NVP, 136 (45%) with an OVD, 52 (17%) with a TRVD, and 11 (4%) with a MVD. When the GLI 2012 equations were applied the number of individuals diagnosed with each ventilatory pattern was: 116 (39%) with a NVP, 136 (45%) with an OVD, 38 (13%) with a TRVD and 11 (4%) with a MVD. These results are shown in Table 1 with additional breakdown of diagnosis by sex.
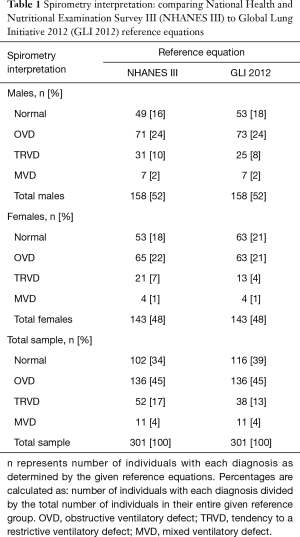
Full table
Of the 147 patients diagnosed as having an OVD using the NHANES equations (including the 11 with a MVD) the grading of severity was: 39 (27%) with a mild defect, 20 (14%) with moderate defect, 30 (20%) with a moderately severe defect, 40 (27%) with a severe defect, and 18 (12%) with a very severe defect. Of the 147 patients diagnosed as having an OVD using the GLI 2012 equations (including the 11 with a MVD) the grading of severity was: 37 (25%) with a mild defect, 23 (16%) with a moderate defect, 25 (17%) with a moderately severe defect, 41 (28%) with a severe defect, and 21 (14%) with a very severe defect. These results are shown in Table 2 with additional breakdown of OVD severity grade by sex.
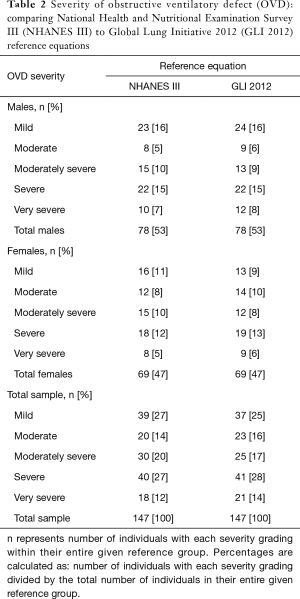
Full table
Of the 63 patients diagnosed as having a TRVD with the NHANES III equations the grading of severity was: 24 (38%) with a mild defect, 33 (52%) with a moderate defect and 6 (10%) with a severe defect. Of the 49 patients diagnosed as having a TRVD with the GLI 2012 equations the grading of severity was: 11 (23%) with a mild defect, 33 (67%) with a moderate defect, and 5 (10%) with a severe defect. These results are shown in Table 3 with additional breakdown of TRVD severity grade by sex.
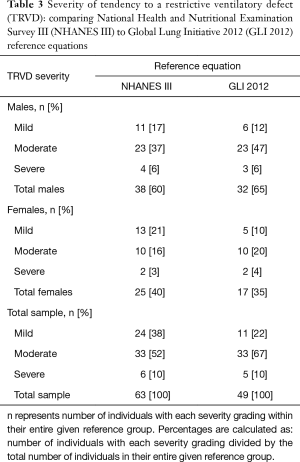
Full table
Transitioning from the NHANES III to the GLI 2012 equations resulted in a change in diagnosis in a total of 18 individuals (6.0%). The diagnosis changed from an OVD to a NVP for 2 individuals (0.7%), from a NVP to an OVD for 2 individuals (0.7%), and from a TRVD to a NVP for 14 individuals (4.7%). There was change in the proportion of individuals in nearly every grade of severity in both the OVD and the TRVD groups when transitioning from the NHANES III to the GLI 2012 equations. These changes did not show a propensity to either increase or decrease the severity of the grading.
Discussion
The GLI 2012 equations were derived from the largest spirometry dataset to date, with data collected from 26 countries including Australia (4). Spirometry data from a sample population at GCHHS was in fact provided for the GLI 2012 report. The GLI 2012 spirometry reference equations have been endorsed internationally by the ERS, the ATS, the American College of Chest Physicians, the Australian and New Zealand Society of Respiratory Science and the Asian Pacific Society of Respirology (9). Given their wide acceptance it is likely that the GLI 2012 equations will become the reference range of choice in countries where a Caucasian population predominates.
Linares-Perdomo et al. (5) noted significant differences in the predicted LLN for both FEV1 and FEV1/FVC when changing from the NHANES III to the GLI 2012 equations. They noted this to be most prominent in older and taller or shorter individuals, with the differences being large enough to result in possible differences in clinical management. Brazzale et al. (6) reported a 2.2% reduction in diagnosis of OVD and a 5.3% reduction in a diagnosis of TRVD when changing equations. Quanjer et al. (7) found a reduction in diagnosis of OVD in 1.2% of males and 2.5% of females when changing equations. This group also found a reduction in diagnosis of TRVD in 5.5% of males and 4.7% of females. This previously observed reduction in the number of individuals with a diagnosis of TRVD when changing from the NHANES III to the GLI 2012 equations was also noted in our study.
The aim of our study was to assist clinicians in anticipating changes in diagnosis of ventilatory defect and classification of severity if the GLI 2012 equations were to be introduced. If spirometry data are analysed using the new equations then there is likely to be a reduction in the number of patients diagnosed with TRVD. This is accounted for by the lower value for FVC LLN seen within the GLI 2012 dataset. It is important to note that spirometry is not diagnostic for restrictive ventilatory defects without static lung volumes. For this reason the terminology ‘tendency to a restrictive ventilatory defect’ (TRVD) is used throughout this article (10). In our study half of the individuals whose diagnosis changes from TRVD to NVP still had a total lung capacity below the LLN.
A clear advantage of changing to the GLI 2012 dataset is that it is drawn from individuals aged from 3 to 95 years compared to the NHANES III dataset that is drawn from individuals aged 8 to 80 years. This improves the consistency of disease monitoring in childhood as it reduces the need to transition between dataset equations. It also ensures that the results are more representative of individuals aged over 80 years (11).
The GLI 2012 dataset is likely to provide the spirometry equations of choice to many clinicians working in predominately Caucasian populations given its larger cohort size, broader age range and wide acceptance from several international respiratory organisations. When transitioning to these equations clinicians should be aware of the possibility of a reduction in diagnosis of TRVD, as demonstrated in our study.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948-68. [Crossref] [PubMed]
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 1999;159:179-87. [Crossref] [PubMed]
- Hall GL, Thompson BR, Stanojevic S, et al. The Global Lung Initiative 2012 reference values reflect contemporary Australasian spirometry. Respirology 2012;17:1150-1. [Crossref] [PubMed]
- Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40:1324-43. [Crossref] [PubMed]
- Linares-Perdomo O, Hegewald M, Collingridge DS, et al. Comparison of NHANES III and ERS/GLI 12 for airway obstruction classification and severity. Eur Respir J 2016;48:133-41. [Crossref] [PubMed]
- Brazzale DJ, Hall GL, Pretto JJ. Effects of adopting the new global lung function initiative 2012 reference equations on the interpretation of spirometry. Respiration 2013;86:183-9. [Crossref] [PubMed]
- Quanjer PH, Brazzale DJ, Boros PW, et al. Implications of adopting the Global Lungs Initiative 2012 all-age reference equations for spirometry. Eur Respir J 2013;42:1046-54. [Crossref] [PubMed]
- Philip H. Quanjer. Become an Expert in Spirometry. Software for interpreting lung function test results. Available online: http://www.spirxpert.com/download/download1a.html
- E-learning resources. Which Organizations Support the GLI-2012 Equations. Available online: http://www.ers-education.org/guidelines/global-lung-function-initiative/faq/which-organizations-support-the-gli-2012-equations.aspx
- Ben Saad H, El Attar MN, Hadj Mabrouk K, et al. The recent multi-ethnic global lung initiative 2012 (GLI2012) reference values don't reflect contemporary adult's North African spirometry. Respir Med 2013;107:2000-8. [Crossref] [PubMed]
- Hüls A, Krämer U, Stolz S, et al. Applicability of the Global Lung Initiative 2012 Reference Values for Spirometry for Longitudinal Data of Elderly Women. PLoS One 2016;11:e0157569. [Crossref] [PubMed]


