Safety and feasibility of uniportal video-assisted thoracoscopic surgery for locally advanced non-small cell lung cancer
Introduction
Conventional video-assisted thoracoscopic surgery (VATS) lobectomy for the treatment of early non-small cell lung cancer (NSCLC) has been well established (1-4). Despite the approaches of conventional thoracoscopic pulmonary resections are preferred for lung cancer because of many potential benefits such as decreased postoperative pain, diminished inflammatory response, decreased hospital length of stay, and faster access to adjuvant chemotherapy (5). However, its use for locally advanced lung cancer is still limited. Completeness of oncologic principles of anatomic resections, complete lymphadenectomy, technical challenges, and potential safety concern are the main reasons for the low adoption of VATS in advanced cases. So thoracotomy technique remains the gold standard for resections of advanced-stage NSCLC.
The experience has grown with VATS technique, studies have shown conventional three portal VATS lobectomy can be safely and effectively performed in patients with locally advanced lung cancer (6,7). Recent studies have reported that uniportal VATS lobectomy has been increasing applied in treatment of NSCLC with the improvements in both endoscopic instruments and surgical skills (8). Even this procedure can be used in advanced lung cancers or complex pulmonary resections such as sleeve lobectomies, vascular reconstruction, and large tumors (9,10). Since we started our uniportal approach for thoracoscopic lobectomy in December 2013, more than 95% of all lobectomies for NSCLC were performed thoracoscopically. The experience of UVATS technique we acquired, new curve and double articulate instruments developed, and new angulated staplers applied, increasing the indications for uniportal VATS lobectomy, as well as locally advanced NSCLC. As a result, UVATS is actually the next step in the evolution of minimally invasive thoracic surgery and represents the least aggressive form to treat lung cancer (11).
The purpose of this study is to assess the safety and feasibility of Uniportal VATS in the treatment of locally advanced NSCLC (T ≥4 cm, T3 or T4 tumors and/or neoadjuvant chemotherapy) and to compare the perioperative outcomes with open thoracotomy.
Methods
A retrospective observational study of patients who underwent lung resections between January 1, 2013 and September 31, 2015 for patients of NSCLC at Thoracic Surgery Department, the Second Affiliated Hospital of Zhejiang University School of Medicine. All the patients provided written informed consent before operation and were performed through a single, small incision by Dr. Junqiang Fan. All studies were done in accordance with hospital ethic committees.
Locally advanced clinical stage NSCLC were considered as tumors ≥4 cm, T3 or T4 tumors, and/or tumors that received neoadjuvant chemotherapy (6). Most of patients underwent routine perioperative pulmonary function testing, chest computed tomography, brain MRI, electrocardiography, and fused positron emission tomography-computed tomography. Mediastinal staging was performed by TBNA or EBUS-TBNA when preoperative CT showed lymph node bigger than 1cm at the mediastinum or PET/CT depicted mediastinal lymph nodes metastasis before resection or initiating neoadjuvant chemotherapy.
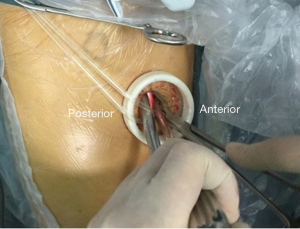
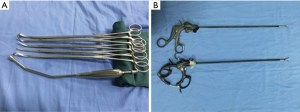
The procedures of U-VATS lobectomy has been described previous, which was similar to that reported by Gonzalez-Rivas et al. (12). Briefly, it was performed that only the incision about 3–5 cm (average 3.5 cm) long between the anterior axillary line and posterior axillary line over the fourth or fifth intercostal space without rib spreading. This incision was the same as universal incision that we used in the 3-port VATS technique. A 30-degree, 10-mm high definition camera thoracoscope was applied for panoramic view and placed at the posterior part of the incision during most of operative time (a plastic tube binding the thoracoscope fixed by a clamp for relieving the cameramen’s hand tiredness) (Figure 1). It was not necessary to use a trocar, conversely, a small disposable, plastic wound retractor was placed to stretch the incision. The plastic wound retractor improved camera angle of vision, and diminished compression of the intercostals space. At the beginning, the thoracoscopic instruments of UVATS were the same as that we used for conventional three portal VATS, later, the double articulate thoracoscopic instruments we used in UVATS procedure (Figure 2). For dissection, we used a Suction Instrument (Panther Healthcare, China) and electrocautery hook or ultra-sonic scalpel in each hand. The indication and contraindication considered as the same as conventional 3-portal VATS.
Conversions were defined as operations that began with uniportal VATS dissection and were finished as rib spreading thoracotomies. Uniportal VATS exploration without structural dissection that continued as thoracotomy did not qualify as a conversion and was considered to be a planned thoracotomy (6).
The groups were divided as follows: (I) U-VATS; (II) open. Variables studied in each patient were records, including age, sex, smoking habits, presence of associated comorbidities, length of hospital stay, days in intensive care unit, duration of chest tube, operative blood loss, operative time, number of lymph nodes retrieved, the number and percent of “nodal upstaging”, adhesion, postoperative complications, and time to initiate adjuvant chemotherapy. Complications included prolonged air leak, atrial fibrillation, bleeding, pneumonia, bronchopleural fistula, chylothorax, death, and 30-day mortality.
A descriptive analysis of the variables studied was performed. The quantitative variables are shown as mean ± standard deviation (SD), and categorical variables are presented using percentages. The Chi-square test or Fisher exact test was used for quantitative variables. The significance level is 0.05. Data analysis was performed using the SPSS software (version 17.0 for windows).
Results
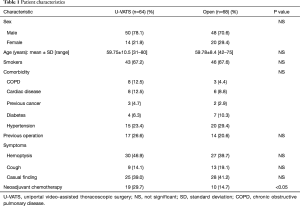
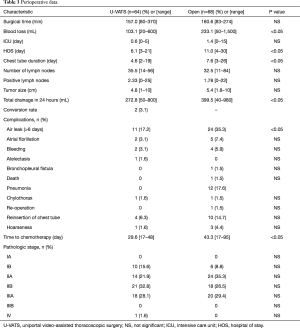
We developed our uniportal VATS approach in December 2013, until September 2015, we have continuously performed 416 major pulmonary resections with NSCLC using this uniportal technique. Only locally advanced NSCLC cases were included in this study, a total of 132 cases, U-VATS group 64 vs. open group 68 patients. The demographic characteristics of patients in both groups are shown in Table 1. Of the 132 patients in the final analysis, uniportal VATS resections was attempted in 64 patients and successfully completed in 62 patients. Two patients were converted to anterolateral open thoracotomy (by lengthening the single incision). Among these conversions, both were attributed to lymph nodes fused to pulmonary artery and bronchus. For a safe operation, we decided to convert to open thoracotomy promptly (there were no emergent conversions). The remaining 68 patients were performed in an anterior lateral open fashion with rib spreading. According to preoperative contrast-enhanced CT, a tumor involving pulmonary vessels made open thoracotomy directly. There were 60 patients in open group with tumor >4 cm while 42 patients in U-VATS group with tumor >4 cm. There were 15 patients with T3, 1 patient with T4 in Open group, and 18 patients with T3, no patient with T4 in U-VATS group. There were no significant differences in age, sex, smoking habits, and associated comorbidity between the groups. In our study, a higher percentage of patients in VATS group (29.7%) received neoadjuvant chemotherapy treatment than in thoracotomy group (14.7%) before surgery.
Full table
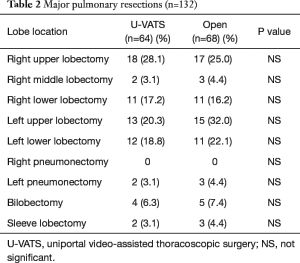
The type of resection performed and their frequency are described in Table 2. Lobectomy (U-VATS, 56 vs. open, 57 patients), pneumonectomy (U-VATS, 2 vs. open, 3 patients), bilobectomy (U-VATS, 4 vs. open, 5 patients) and sleeve lobectomy (U-VATS, 2 vs. open, 3 patients) were similar frequent between U-VATS and Open group. However, no right pneumonectomy was performed in both groups.
Full table
Perioperative details are summarized in Table 3. The difference in tumor size between groups was not statistically significant (median tumor size U-VATS 4.8 cm vs. open 5.4 cm). The mean number of lymph nodes dissection (U-VATS 35.5 vs. open 32.5) and positive lymph nodes (U-VATS 2.33 vs. open 1.78) were similar between the two groups. There was no statistically significant difference in median operative time between two groups. When comparing to the open group, less median blood loss in U-VATS group, as well as length of stay in ICU, HOS, Chest tube duration, and total drainage in first 24 hours. The most frequency of complication was air leak in U-VATS group, as well as in open group. However, the air leak was more frequency in open group than in U-VATS group (35.3 vs. 17.2). From the patients in U-VATS group, 57.8% of them were discharged in 5 days while 5.9% of patients in open group. There was only one perioperative death on the 55th postoperative day in open group after complex branchial sleeve resections. The cause of death was bronchopleural fistula and tumor metastasis. One patient required reoperation in open group for chylothorax. The time to access adjuvant chemotherapy after operation was significant less in U-VATS group (U-VATS 29.6 vs. open 43.3).
Full table
The most common pathological type in U-VATS group (30, 46.9%) was adenocarcinoma while in open group (30, 44.1%) it was squamous cell carcinoma. The stages I of tumors was more frequency in group U-VATS (17.2%) than in group open (8.8%). The stages I patients appeared after operation because of down period after neoadjuvant chemotherapy. And the other stage of tumors was not difference significantly between two groups.
Discussion
Recently, VATS lobectomy has been recommended by NCCN guidelines as the choice of surgery for NSCLC. Over the past 20 years since its birth, it is gradually well established for the treatment of lung cancer around the world, especially for the early stage of NSCLC. Compare to open thoracotomy, VATS lobectomy offers many potential benefits such as decreased postoperative pain, reduced hospital length of stay, diminished inflammatory response, faster access to adjuvant chemotherapy and faster recovery. Despite these advantages, majority of publications on VATS lobectomy are limited to the patients of early stage, it is recently even attempted in advanced lung cancer patients (13,14). However, the role of VATS for treatment of locally advanced NSCLC is still infrequent and has been remain controversial.
The concept of uniportal VATS was first reported by Migliore and his colleagues for simple thoracic operation over a decade ago (15). Until 2010, Dr. Diego Gonzalez-Rivas reported world’s first uniportal VATS major pulmonary resections, as a major milestone approach (16). Recent series studies have confirmed that uniportal VATS has several advantages, such as improved exposure directly during surgery, decreased postoperative pain and paraesthesias, and increased cosmetic effects. With experience gained, enhancement of the surgical instruments and improvement of high definition cameras, locally advanced lung cancers and complex resections, such as post chemotherapy resections, lobectomies with chest wall resections, pneumonectomy or sleeve resection are being performed by uniportal VATS in experienced centers (17).
In this study, we report the safety and feasibility of uniportal VATS for locally advanced NSCLC. The conversion rate is an important indicator to assess the safety of uniportal VATS techniques. The previous literature showed that conversion rates from VATS to open thoracotomy ranges from 2–23% (6), with these higher rates coming from patients with advanced lung cancers or complex cases. Two patients were converted to anterior lateral thoracotomy in our series (only 3.2%). The main reason for conversion was a tumor involving pulmonary vessels, and calcified lymph nodes fused to main vessels. Compared to planned open patients, there were obvious better performance in perioperative outcomes in U-VATS group like operative blood loss, chest of tube duration, and hospital stay. Actually, more patients in the uniportal VATS group received neoadjuvant therapy (29.7% vs. 14.7%). However, this treatment can easily induce hilar tissue inflammation, edema and vessel’s fragility, making the surgery even more difficult, but these complexity of hilar and lymph node dissection were performed successfully, due to our previous VATS experience. On the other hand, size reduced tumor can free large operational space and in favor of exposure. Recently, Gonzalez-Rivas and colleagues report that uniportal thoracoscopic surgery is a feasible approach for advanced NSCLC (9). Huang et al. published a study of VATS following neoadjuvant therapy with good postoperative results (7). Our experience suggests that surgeons who have performed more than 50 continuous uniportal VATS lobectomies would be successfully perform these challenging cases. During the operation, when vessels injury and bleeding could not be controlled, we had no hesitation in converting to open thoracotomy. The incision about 3–5 cm was enough to operate without spreading the rib. However, it was difficult to remove the entire lung when pneumonectomy or lobectomy with large tumors was performed. In general, we had to enlarge the skin incision to extract large lobes from 6 to 8 cm.
Mean operation time for uniportal VATS locally advanced NSCLC was lower than open thoracotomy (157.0 vs. 160.6 min), as unexpected, but is not significant. From the literature, our surgical time is even less than reported advanced tumors by using conventional three portal procedure. One reason is the small single incision is performed faster than those in long incision of open group. Comparing to the conventional three-port VATS, uniportal VATS provides visions based on a completely different geometric concept. In fact, the view of uniportal VATS directs to the target lesion as in open surgery (18). Conventional three-port VATS triangulation forces the surgeons to adapt to an unnatural vision is not favorable with standard two-dimensional monitors. The surgeon accustomed to open thoracic surgery has the basis of learning UVATS.
In our study, the incidence of postoperative complications in U-VATS group is lower than open group. The reason may be due to following factors: first, uniportal VATS is the least aggressive form to treat lung cancer now and less painful and predisposes patients to getting out the bed in early period after operation. Second, thoracoscopic approach has a locally magnifying ability, which is beneficial to the identification of pulmonary vessels, bronchia, and small bleeding spots, thereby reducing the occurrence of postoperative complications (19). Third, our rich experience in uniportal VATS major lung resection is also important to reduce the occurrence of postoperative complications. In these complications, a major cause of morbidity after lung resection was prolonged air leak, which always prolonged hospital stay. A prolonged air leak in this study was defined as persistent air leak for more than 6 days after major lung resection. The frequency of prolonged air leak observed in our uniportal VATS (17.2%) less than those in open group (35.3%). In other series, upper lobectomy was a greater risk factor for developing prolong air leak compared with other resection, because they often result in a large apical air space (20,21). In our series, prolonged air leak mainly observed in the case of upper lobectomy or bilobectomy. As a result, HOS in open group was longer than those in U-VATS group.
Uniportal approach, with only one small incision used for all instruments and camera insertion, is easy to interfere with each other, requires instrument better designed for operating. Furthermore, the clinical requirements from surgeons always drive the industry to develop novel, light, small, and procedure-specific instruments for UVATS to allow further reduction in incision size. The newly designed curved-tip endo-stapler will be a great choice for division of a vessel, especially the superior pulmonary vein.
The main limitation of this study is the retrospective design, short term follow up and non-randomized cohort of patients. A randomized trial of U-VATS and Open thoracotomy could not be performed. Because of the existence of some selection bias, we attempted to exclude patients with neoadjuvant chemotherapy to reduce the selection bias. However, there was no significant difference.
In summary, uniportal VATS major pulmonary resection for locally advanced NSCLC is a safe and feasible procedure in experienced center that provides a better perioperative outcome to those open cases. Further studies of long term survival for locally advanced cases need to be validated the oncologic outcomes of the uniportal VATS technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics board of Second Affiliated Hospital of Zhejiang University, School of Medicine (No. 2016-034).
References
- Hartwig MG, D'Amico TA. Thoracoscopic lobectomy: the gold standard for early-stage lung cancer? Ann Thorac Surg 2010;89:S2098-101. [Crossref] [PubMed]
- Naidoo R, Windsor MN, Goldstraw P. Surgery in 2013 and beyond. J Thorac Dis 2013;5 Suppl 5:S593-606. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [Crossref] [PubMed]
- Nagahiro I, Andou A, Aoe M, et al. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg 2001;72:362-5. [Crossref] [PubMed]
- Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [Crossref] [PubMed]
- Huang J, Xu X, Chen H, et al. Feasibility of complete video-assisted thoracoscopic surgery following neoadjuvant therapy for locally advanced non-small cell lung cancer. J Thorac Dis 2013;5 Suppl 3:S267-73. [PubMed]
- Zhu Y, Xu G, Zheng B, et al. Single-port video-assisted thoracoscopic surgery lung resection: experiences in Fujian Medical University Union Hospital. J Thorac Dis 2015;7:1241-51. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Pischik VG. Technical difficulties and extending the indications for VATS lobectomy. J Thorac Dis 2014;6:S623-30. [PubMed]
- Gonzalez-Rivas D. Recent advances in uniportal video-assisted thoracoscopic surgery. Chin J Cancer Res 2015;27:90-3. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Varela G, Thomas PA. Surgical management of advanced non-small cell lung cancer. J Thorac Dis 2014;6 Suppl 2:S217-23. [PubMed]
- Nakanishi R, Fujino Y, Yamashita T, et al. Thoracoscopic anatomic pulmonary resection for locally advanced non-small cell lung cancer. Ann Thorac Surg 2014;97:980-5. [Crossref] [PubMed]
- Migliore M, Deodato G. A single-trocar technique for minimally-invasive surgery of the chest. Surg Endosc 2001;15:899-901. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Shao W, Liu J, Liang W, et al. Safety and feasibility of video-assisted thoracoscopic surgery for stage IIIA lung cancer. Chin J Cancer Res 2014;26:418-22. [PubMed]
- Elsayed H, McShane J, Shackcloth M. Air leaks following pulmonary resection for lung cancer: is it a patient or surgeon related problem? Ann R Coll Surg Engl 2012;94:422-7. [Crossref] [PubMed]
- Cerfolio RJ, Bass CS, Pask AH, et al. Predictors and treatment of persistent air leaks. Ann Thorac Surg 2002;73:1727-30; discussion 1730-1.


