Unusual clotted haemothorax caused by spontaneous intramural haematoma of the oesophagus: a case report
Introduction
Spontaneous intramural haematoma of the oesophagus (SIHO) is an uncommon form of oesophageal injury related to dissection of the mucosa from the muscular layers, which may be an intermediate variant of Mallory-Weiss syndrome (mucosal tear at the lower end of the esophagus) and Boerhaave’s syndrome (spontaneous perforation of the oesophagus) (1,2). Although SIHO usually has a benign course, the mortality rate is 7–9% in patients with multiple comorbidities (3,4). Here, we describe a case of clotted haemothorax caused by SIHO in which uniportal video-assisted thoracic surgery (VATS) was successfully applied as a diagnostic and therapeutic method.
Case presentation
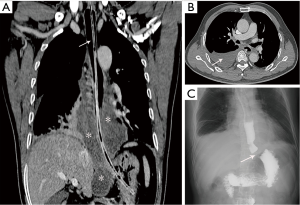
A 51-year-old man visited the emergency room complaining of sudden onset chest pain accompanied with dyspnea and vomiting for 1 hour after the breakfast. The patient had been on therapy with 100 mg aspirin and 5 mg amlodipine per day for 5 years due to previous stroke and hypertension. Physical examination revealed that the breath sound of the right chest was slightly decreased but no other abnormal findings. Chest contrast-enhanced computed tomography (CT) scan showed right pleural effusion and a large oesophageal mass which extended from the level of the carina to the abdominal esophagus (Figure 1A,B). No pulmonary artery thrombosis or aortic dissection was identified. Opacification of the oesophageal lumen with lipiodol showed no leakage but stricture of the gastroesophageal junction (Figure 1C). Oesophageal mucosa was normal on gastroscopic view. However, right thoracentesis showed the presence of haemothorax. Then a right chest tube was inserted at the 6th intercostal space between the middle and posterior axillary line, which drained 800 mL of obsolete uncoagulated blood. Electrocardiography and admission laboratory studies, including troponin levels and coagulation parameters, were normal. After 48 hours of fasting during the aforementioned assessment, the patient was gradually allowed to resume oral intake of fluid diet. His vital signs were stable, and the pleural drainage was less than 100 mL per day within 7 days.
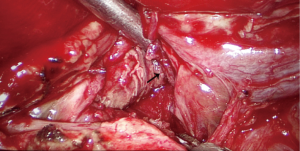
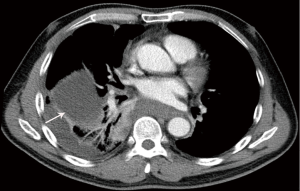
On the 7th day after admission, we did another chest CT scan for this patient which revealed partial atelectasis combined with encapsulated pleural effusion in the right chest (Figure 2), with suspicion of clotted haemothorax. Uniportal VATS exploration was then scheduled for this patient. The inferior mediastinal pleura and the pulmonary ligament were bluish via thoracoscopic view. After opening the mediastinal pleura and dissecting the pulmonary ligament, about 200 mL of obsolete blood and some ‘old blood clot’ effusion was evacuated (Figure 3). The diagnosis of SIHO was confirmed. The ruptured muscular layer of the oesophagus was sutured with 4-0 absorbable stiches after clearing the hemorrhage. The patient was resumed to intake fluid diet on postoperative day three and discharged home seven days after surgery uneventfully.
Discussion
Although the causes of SIHO may include advanced age, the presence of coagulation disorders, and the use of anticoagulant, antiplatelet, or thrombolytic drugs, the actual etiology of SIHO remains unclear (1). SIHO due to aspirin ingestion has been reported by Smith in 1974 (5). In this patient, the presence of SIHO may also be due to the long-term medication of aspirin.
Patients with SIHO usually present with sudden onset of retrosternal chest pain (84%) which occasionally radiate to the back, cause dysphagia, odynophagia (59%) and hematemesis (56%) (6). However, all these symptoms are non-specific. It is hard to distinguish SIHO from other life threatening causes of chest pain, such as acute myocardial infarction, pulmonary embolism, aortic dissection and Boerhaave’s syndrome (7). Thus, the diagnosis of SIHO was usually delayed until other more serious conditions were excluded (8). As for this patient, the diagnosis of SIHO was based on the exclusion of cardiovascular conditions and Boerhaave’s syndrome, and was finally confirmed by surgery.
SIHO generally has benign courses and process. The symptoms usually resolve within 3 weeks of conservative treatment (9). In a few patients, SIHO may cause other complications like uncontrollable bleeding, severe dysphagia and respiratory distress, which required surgical or endoscopic intervention (2,10,11). Clotted haemothorax caused by SIHO has never been reported previously. We first adopted conservative treatment for the present case. The decision to perform uniportal VATS was prompted by the possibility of clotted haemothorax. The ruptured oesophageal muscle was identified and sutured with absorbable stiches during the operation. The patient had a full and uneventful recovery from the procedure.
In conclusion, SIHO accompanied with clotted haemothorax is extremely rare. Although conservative treatment is adequate for the majority of patients with SIHO, uniportal VATS may be a suitable option if there was clotted haemothorax.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hajsadeghi S, Agah S, Iranpour A, et al. Dissecting intramural hematoma of esophagus after thrombolytic therapy: a case report. Asian Cardiovasc Thorac Ann 2015;23:224-6. [Crossref] [PubMed]
- Yen HH, Soon MS, Chen YY. Esophageal intramural hematoma: an unusual complication of endoscopic biopsy. Gastrointest Endosc 2005;62:161-3. [Crossref] [PubMed]
- Restrepo CS, Lemos DF, Ocazionez D, et al. Intramural hematoma of the esophagus: a pictorial essay. Emerg Radiol 2008;15:13-22. [Crossref] [PubMed]
- Hong M, Warum D, Karamanian A. Spontaneous intramural esophageal hematoma (IEH) secondary to anticoagulation and/or thrombolysis therapy in the setting of a pulmonary embolism: a case report. J Radiol Case Rep 2013;7:1-10. [Crossref] [PubMed]
- Smith G, Brunnen PL, Gillanders LA, et al. Oesophageal apoplexy. Lancet 1974;1:390-2. [Crossref] [PubMed]
- Cao DT, Reny JL, Lanthier N, et al. Intramural hematoma of the esophagus. Case Rep Gastroenterol 2012;6:510-7. [Crossref] [PubMed]
- Clark W, Cook IJ. Spontaneous intramural haematoma of the oesophagus: radiologic recognition. Australas Radiol 1996;40:269-72. [Crossref] [PubMed]
- Lu MS, Liu YH, Liu HP, et al. Spontaneous intramural esophageal hematoma. Ann Thorac Surg. 2004;78:343-5. [Crossref] [PubMed]
- Kumar V, Mallikarjuna HM. Gokulnath. A miniseries of spontaneous intramural esophageal hematoma in hemodialysis patients: a rare cause of dysphagia. Hemodial Int 2014;18:558-61. [Crossref] [PubMed]
- K C S, Kouzu T, Matsutani S, et al. Early endoscopic treatment of intramural hematoma of the esophagus. Gastrointest Endosc 2003;58:297-301. [Crossref] [PubMed]
- Ott DJ, Richter JE, Wu WC, et al. Radiographic evaluation of esophagus immediately after pneumatic dilatation for achalasia. Dig Dis Sci 1987;32:962-7. [Crossref] [PubMed]