A telemedicine grand round communication was held between the Guangzhou Institute of Respiratory Disease (GIRD), China, and the Firestone Institute for Respiratory Health (FIRH), Canada on July 22, 2015 to discuss about a man with recurrent episodes of cough, expectoration and wheezing for 3 years with aggravation during the previous 6 months.
A 43-year-old man with cough, expectoration and recurrent wheezing
Case presentation
A 43-year-old man was admitted to the Guangzhou Institute of Respiratory Disease (GIRD), the First Affiliated Hospital of Guangzhou Medical University because of recurrent episodes of coughing, expectoration and wheezing for 3 years with aggravation during the previous 6 months.
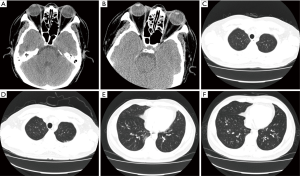
The patient began to cough with white phlegm after a cold in 2012. The cough was worse upon waking in the morning and laying down at night. He had no chills, fever, chest pain, chest tightness, palpitations, night sweats, hemoptysis or paroxysmal nocturnal dyspnea. He was diagnosed with ‘upper respiratory infection’ in a local hospital and received symptomatic treatment for several days that he could not recall clearly. His condition improved, but he still had occasional relapses. One month after the treatment, he suffered from an attack of wheezing during moderate activity and was admitted to a local hospital, in which he was diagnosed with ‘bronchial asthma’ and ‘type 2 respiratory failure’, from 1st December to 13th December 2012. Chest CT scan showed interstitial inflammation in the right middle and left upper lobe. Pulmonary function test suggested mild obstructive ventilatory dysfunction with FEV1 at 72.2% of predicted, FVC at 89.7% of predicted, and FEV1/FVC ratio at 66.81%. The bronchodilator reversibility test was positive: FEV1 increased >12% and >200 mL with inhaled Ventolin 400 µg (Figure 1). No abnormalities were noted in echocardiogram. Inflammation was observed in both bronchial trees on bronchoscopy. After receiving symptomatic treatment, the patient’s condition improved but did not normalize. Upon referral, he was admitted to our hospital for further treatment. The treatment included Methylprednisolone at a daily dose of 40 mg intravenously and oral Theophylline 0.2 g once every 12 hours for 3 days. After that, his condition improved and he was subsequently discharged. He continued to take Singulair, Ketotifen and Theophylline, as well as Symbicort 320/9 µg bid and Foster 100/6 µg bid. His symptoms were under control.
The patient was re-admitted on May 25, 2015, 6 months before which, his symptoms recurred and were worse in cold weather. He began to wheeze after mild activity and coughed with increasing white phlegm. He received intravenous treatment with unknown regimen in a local hospital for a couple of days, but his condition was not improved. So he was referred to our hospital for further treatment. Since the onset of the disease, his appetite stayed the same with normal stool and urine. He lost 6 kilograms in 6 months.
He had no known allergies, but he had been suffering from cataract for about 1 year, gallbladder polyps and fatty liver for about 4 years. He was not exposed to an epidemic area before admission. He had smoked for 10 years, which was about 5 pack years, and ceased smoking 10 years ago. He got married at 25 and got along with his wife well. He had one son and one daughter, both of whom were healthy. No relevant family history was identified and no one in his family had similar symptoms.
On admission, vital signs were stable. The temperature was 36.8 °C, the pulse was 90 beats per minute and regular, the blood pressure was 120/73 mmHg and the respiratory rate was 20 breaths per minute. He was well developed and moderately nourished and free from skin eruption. Multiple flaky red macules, about 2 to 4 centimeters in diameter, were noted on both lower extremities without pruritus. He felt mild pain when pressing the red macules. There was no spider angioma. Superficial lymph nodes were not enlarged. The respiratory movement was bilaterally symmetric. Breath sounds from both lungs were coarse and wheezes were heard during expiration. Heart sounds and the remainder of physical examination were normal. His annual lab examination in May 2015 showed elevated serum total IgE (1,072 kU/L) and high percentage of eosinophils in peripheral blood (27.8%). Fractional exhaled nitric oxide (FeNO) was 37 ppb. The proportions of induced sputum cell counts were as follows: neutrophils 62.5%, macrophages 31%, eosinophils 2% and lymphocytes 4.5%. In bronchoalveolar lavage fluid (BALF), the proportions of cells were as follows: neutrophils 53.5%, macrophages 10.5%, eosinophils 35% and lymphocytes 1%. Eosinophils in peripheral blood were normal, although bone marrow puncture showed active eosinophil hyperplasia when he received treatment in our hospital for 3 days. Sputum smear tests for fungi and TB were all negative for 4 times. Fungal sputum culture and antigen test were also negative. The results were negative for mycoplasma pneumonia and HIV. Other test results are shown in Table 1.
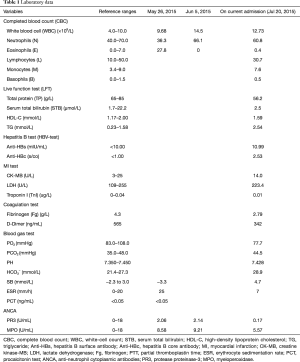
Full table
Since admission to our hospital, nebulized compound ipratropium bromide solution 2.5 mL every 8 hours and budesonide 2 mL every 12 hours had been administered. The patient’s condition was not improved. On June 8th in the hospital, the patient was treated with intravenous cyclophosphamide (CTX) 0.2 g every other day for 3 days, and then with oral CTX as subsequent therapy (Table 2) for 3 days, after which, his symptoms of wheezing and cough improved.
Full table
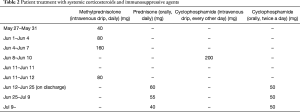
On the second day in the hospital, chest CT scans revealed signs of bronchiolitis obliterans on bilateral lungs and nodules were noted in the right lower lobe (Figure 2). Pulmonary function test suggested severe obstructive ventilatory dysfunction with FEV1 at 34.70% of predicted, FVC at 73.4% of predicted, and FEV1/FVC ratio at 38.58%. The bronchodilator reversibility test was positive: FEV1 increased >12% and >200 mL with inhaled Ventolin 400 µg. Diffusion capacity declined mildly and airway resistance was normal (Figure 1).
In turbinate mucosal tissue, basement membrane thickening, mucosal edema, scattered lymphocytes and few eosinophils was noted. Besides, the patient presented with focal epithelial squamous metaplasia, local thickening of basement membrane, submucosal edema, smooth muscle hyperplasia, increased lymphocytes and eosinophils on the mucous membrane of the lower right bronchus. Bronchiole wall was thickened on the right lower lobe, fibrous hyperplasia was noted, cellulose effused in alveolar cavities, focal lymphocytic infiltration was observed, bronchial wall and pulmonary interstitial presented with more eosinophil infiltration without vasculitis and granuloma.
Why is a grand round discussion warranted for this patient?
Dr. Qingling Zhang (Pulmonologist at GIRD):
After the treatment with a large dose of steroids and CTX for 3 days, the patient felt much better with no wheezing and only a bit of cough. The dose of CTX was reduced from 200 mg with intravenous drip every other day to 50 mg orally twice a day. With treatment, the patient’s condition further improved and the symptoms were relieved and his blood eosinophils count decreased. CT scans of chest and sinus showed milder inflammation in both lungs and sinus than before. In terms of lung function, spirometry on June 11 after high dose steroids treatment suggested mild obstructive ventilatory dysfunction, which was much better than his condition on admission in May before the steroids and CTX treatment. FEV1 increased to 77% of predicted. This patient was discharged on the 12th day (July 12). Then he was followed up in clinic, the systemic corticosteroid was gradually stepped down from a daily dose of prednisone 60 to 40 mg in 4 weeks and maintain CTX 50 mg orally twice a day. Recently, we re-examined his lung function. His spirometry results were a bit worse than the previous one in June and suggested moderate obstructive ventilatory dysfunction with FEV1 66% of predicted. Peak flow monitoring indicated that the values been improved greatly since June 8th when we started high dose steroids as well as CTX, and the values had been stable in the following outpatient clinic until now. This patient met four items of the diagnostic criteria of Eosinophilic Granulomatosis with Polyangiitis [EGPA, formerly known as Churg-Strauss syndrome (CSS)], including asthma, peripheral blood eosinophils greater than 10%, abnormalities in the paranasal sinus, and non-fixed pulmonary infiltrates. We were considering this patient might be with EGPA, which only affected the lung. Therefore, the purposes of today’s discussion are as follows: (I) could this patient be diagnosed with EGPA or chronic eosinophilic pneumonia (CEP)? Or has he suffered from a special phenotype of severe asthma? (II) how to prevent the side effects from using high dose steroids and CTX? (III) how to manage his further treatment including the steroids and immunosuppressive agent, as well as the side effects?
Prof. Nanshan Zhong (Grand round moderator, Pulmonologist at GIRD):
This case raised two questions. First, whether the patient could be diagnosed with EGPA, or just be diagnosed with very severe asthma (refractory asthma), or some other diseases like CEP? Secondly, how to manage the relatively large dose of corticosteroids and related side effects?
Before the discussion, we shall provide chest imaging data and pathologic data. First of all, I would like to invite Dr. Zeng to present the radiological information.
Images and pathological discussion
Dr. Qingsi Zeng (Radiologist at GIRD):
The first CT scan was performed in March 2013. It showed decreased attenuation of both lungs, air trapping, and diffuse thickening of bronchial walls. The second chest CT scan performed 7 months later (Oct 2013) revealed improvement of the thickening of bronchial wall and the recoiled pattern disappeared after treatment. The lesions included centrilobular nodules, tree-in-bud sign in the upper and lower lobe and the thickening of bronchial walls showed on May 2015 were more remarkable than that in 2013 (Figure 2). The CT findings indicated the disease was progressing. But the latest CT scan after two months of treatment (July 2015) showed the infiltration disappeared and both lungs were clear. It’s confusing that the thickening of the bronchial wall still recurred this year even after effective treatment and improvement this month (July 2015). The dynamic CT series (July 2015) suggested the patient was recovering. All these findings indicate small airway diseases, mostly like a kind of untypical severe asthma. The sinus CT scan showed inflammation of bilateral maxillary sinus and ethmoidal sinus.
Prof. Nanshan Zhong:
Apart from the changes of bronchus, whether the patient had pneumonia when his symptoms recurred is extremely important for us to make diagnosis, for example, CEP or others, even CSS. May I ask Dr. Zeng, do you think this patient had pneumonia from the radiological point of view?
Dr. Qingsi Zeng:
We don’t think this patient had pneumonia because we cannot see any ground-glass opacity or consolidations. We just saw very tiny lesions with small centrilobular nodules and tree-in-bud. All evidence from CT scans is related to airway diseases.
Prof. Nanshan Zhong:
Are there any separate or tiny signs of pneumonia?
Dr. Qingsi Zeng:
No, we don’t think so.
Prof. Nanshan Zhong:
OK. This is very important for us to think about the diagnosis. Let’s move to the pathological information session. I would like to invite Dr. Gu to introduce the histological data.
Dr. Yingying Gu (Pathologist at GIRD):
Biopsies of the nasal mucosa, mucosa membrane of bronchus and lung were conducted on this patient. Let me introduce the biopsy of the nasal mucosa first. Sample of the nasal mucosa was obtained, covered by pseudostratified columnar ciliated epithelium predominantly. Widening of basement membrane was noted. Edema was seen under the mucosa and it looked pale. Scattering lymphocyte and a few eosinophils were infiltrated. A specimen of the bronchial mucosa revealed that pseudostratified columnar ciliated epithelium was predominant. Eosinophils infiltration and edema were observed under the mucosa. Another slice of the bronchial specimen also showed obvious edema on the mucosa with more eosinophils infiltration. There were no signs of vasculitis presented on the small vessels. The slice of transbronchial lung biopsy showed a lot of eosinophils and lymphocytes infiltration in the interstitial tissue, however, no eosinophilic angiitis was noted around the small vascular walls. A few eosinophils exudation were found in the alveolar space, while more eosinophils were infiltrated in the alveolar septum (Figure 3). The first diagnosis we considered was EGPA. The second consideration was CEP, and the possibility of idiopathic hypereosinophilic syndrome (IHES) should be excluded. In terms of the diagnosis of EGPA for this patient, there were no typical pathological changes of angiitis and granulomatosis, but the clinical symptoms and presentations were systemic, including chronic gastritis, rashes on the skin. From the microscopy, eosinophils infiltrations were noted in nasal mucosa, bronchus, and the lung. In the early stage of EGPA, the pathological changes of vasculitis and granulomatosis may not be presented. Usually, it takes several years to show the changes of angiitis and granulomatosis with the development of the disease. Therefore, a possibility of EGPA was considered first, and the second differential diagnosis of CEP should be excluded. Eosinophilic infiltrations in the interstitial lung tissue may also be presented in the case of CEP, but the changes are mostly localized in the lung, not systemic. Compared to EGPA, the severity of eosinophilic infiltration of CEP is often milder. The third diagnosis we excluded was IHES because the clinical presentation of this patient was not supportive; meanwhile, the cell count of eosinophils in the peripheral blood was normal and the level of eosinophils in the bone marrow was a bit higher after the treatment.
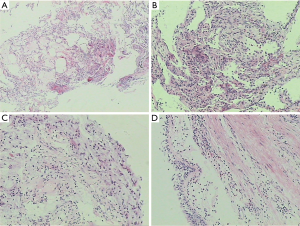
Overall, we tend to diagnose this case with EGPA according to the clinical presentation and pathological findings, as well as the comparison of three differential diagnoses.
Prof. Nanshan Zhong:
Dr. Gu, how do you think about the diagnosis of severe asthma based on the pathological findings?
Dr. Yingying Gu:
For severe asthma, the pathological changes usually are localized in the bronchial mucosa, smooth muscle hypertrophy accompanied with mucous gland hyperplasia should also be seen, and there are not many eosinophilic infiltrations in the lung. However, obvious eosinophilic infiltration was presented in the lung of this patient, so I prefer to a diagnosis of systemic disease.
Prof. Nanshan Zhong (in summary):
The pathologist has different opinions on the diagnosis. The radiologist’s diagnosis seems to be severe asthma based on the imaging findings. There is no much radiological clue showing the lung parenchymal infiltration. However, the histological examination showed eosinophilic infiltration in the bronchus and the alveoli, as well as in the lung interstitial space. The diagnosis of the patient is controversial.
Now, I would like to invite experts from the Firestone Institute for Respiratory Health (FIRH) to share their opinions.
Differential diagnosis
Dr. Paul O’Byrne (Pulmonologist at FIRH):
This gentleman, first of all, has had episodes of severe, variable airway obstruction. When he has been acutely ill, his lung function has been very severely impaired. When he is well, his lung function is not normal, but not far from normal. Secondly, he has atopy. He has an elevated total IgE over 1,000 kU/mL. However, we are not given any information about what he might be sensitized to. One of the tests that I think we’d consider here would be a very simple skin prick tests which might be helpful to provide evidence of some important allergens which he is sensitized to. If possible, avoiding these allergens might help to improve his clinical symptoms. The third component of this case is his eosinophilia. We can confidently exclude a diagnosis of eosinophilic pneumonia, as the radiologist indicated that there was no evidence of consolidation in the lungs with the extensive radiographic investigations. In my opinion, the diagnosis of EGPA requires pathological evidence of those changes. However, you have pathology which shows no evidence of angiitis, vasculitis or granulomatous. Therefore, at this moment, I am fairly confident that EGPA is probably not the reason why this man was so sick.
What he does have is, in my opinion, severe eosinophilic asthma. The asthma is documented by variable airway obstruction and the eosinophilia was being shown in his blood stream and BAL fluids, although the sputum eosinophils were very borderline and probably not elevated. He did respond very well when treated with intravenous and higher doses oral corticosteroids. So, the question, is whether there is anything else that could be causing the severe eosinophilia. Could this be, for example, allergic bronchopulmonary aspergillosis (ABPA), which can cause severe eosinophilia? However, the radiology makes that extremely unlikely. There are no characteristic upper lobe changes that we see with ABPA. The question becomes whether anything else can be done to establish the diagnosis. He was very thoroughly investigated, including lung tissue biopsy. The only additional test to do at this moment would be some skin prick testing (SPT) to identify the relevant environmental allergens. The immunological testing ANCA was negative, and ESR was not markedly elevated.
Another comment is that one of the biopsies we looked at was the airway mucosal biopsy. To me, it looked very much like an asthmatic airway biopsy, with a thickening of the submucosal basal membrane and a great deal of airway smooth muscle in that biopsy, much more than we see in a normal, non-asthmatic individual.
Altogether, I would not pursue the question of him having, at least at this moment, any evidence of vasculitis.
Dr. Gerard Cox (Pulmonologist at FIRH):
I don’t think EGPA is the most likely diagnosis, but if it was present, one might find it in the following way.
Firstly, the skin lesion that is referred to, we heard that was acne, which might be a side effect of prednisone possibly but not necessarily evidence of vasculitis. But if the patient had any rash that was unexpected, unusual and uncommon, I think it would be a good idea to biopsy that rash and see what tissue changes are present. Secondly, the pathologist made an excellent point about vasculitis presentation and the angiitis (EGPA), and why didn’t have a changing in presentation over time. If we see a patient at the very beginning of the presentation, they might not have the entire syndrome present. However, he has been sick for 3 years, which should be almost long enough for most things to come out. Nevertheless, it would be a good idea to recheck his ANCA levels sometime in the future. A number of our patients with CSS had a very low level of ANCA, usually just above the upper limit of normal range and they can certainly vary up and down.
We heard about a few other symptoms including gastritis. Obviously, if eosinophilic gastritis or eosinophilic esophagitis was present, that would make a diagnosis of EGPA much more solid. The biopsies of the airway (nose, bronchus and lung) showing eosinophils, according to Dr. O’Byrne’s argument about all that eosinophilic inflammation, supposed to be a track for allergic asthma and allergic rhinitis. Therefore, I think we have to find the eosinophilic infiltration outside the respiratory tract. In my opinion, stomach or esophagus given the symptoms of reflux and gastritis would be a good place to look for eosinophilic inflammation. I heard something about eye symptoms, and I wonder if he has got any evidence of vasculitis affecting his eyes. In our situation, we will ask for a specialist to see the patient when we worry about that because we don’t feel confident at the bedside excluding vasculitis of various levels of his eye. That would strengthen the argument that this is a vasculitis syndrome if it was found.
Moreover, there were some tests done showing a possible involvement of the heart because some of the enzymes were raised in the blood. We would repeat that assessment with an ECG to look for any problems there, as well as echocardiogram as a minimum. At the ATS meeting this spring in Denver, there was a presentation on EGPA with cardiac involvement where they showed with PET scanning. They found involvement of the myocardium in their patients with EGPA more often than expected. So if you want to find evidence of another organ involved to prove and make the case for EGPA, I think the heart would be a good place to look at if PET scanning is available. The last, mononeuritis has such different symptoms from allergy and asthma, so if the patient has anything suggests mononeuritis syndrome, that might change Dr. O’Byrne’s opinion away from this being severe, allergic asthma affecting all the respiratory tract.
Discussion about management
Dr. Paul O’Byrne:
Another comment is in relation to his treatment since he is being treated with cyclophosphamide. Of all the medications he’s on, cyclophosphamide is the one I have the most concern about side effects. I would stop cyclophosphamide due to the absence of pathological evidence of vasculitis. I would manage him with systemic corticosteroids. Then I think about what else may be additional useful treatment. One thing that might be available and could be a value is anti-IgE, omalizumab. There is evidence that omalizumab can be helpful in reducing the risk of severe exacerbations in patients with severe refractory asthma. A recent study (1) supported that this approach is the most likely to work in patients who had an elevated eosinophilia at least in the airways. That is one possibility. The second issue is optimizing his inhaled medications (dose of the inhaled corticosteroids). I would certainly treat him with a combination inhaler of ICS and LABA because the patient has variable airway obstruction and inflammation, both of those are appropriate. I personally would introduce the combination budesonide/formoterol in this treatment plan because it can be useful as a maintenance treatment and as a rescue. We did not hear about how much rescue medicine the patient is taking but I suspect from his history that it is probably several times a day. So if this is true, then he should get a rescue treatment containing corticosteroid, as well as a bronchodilator. We often also consider whether using higher doses of additional ICS, such as budesonide or fluticasone given in addition to budesonide/formoterol and try to optimize the inhaled medication doses.
Dr. Andrew McIvor (Pulmonologist at FIRH):
I fully agree with Dr. O’Byrne about what he said, but I would like to make a small comment. One thing that I noticed is that the patient was on montelukast. There have been reported a black box warning about montelukast perhaps a potentiation of CSS. There are two ways this syndrome may present. Sometimes, people with severe asthma are on steroids, and if montelukast is added in, they seem to get a little bit better. But when the oral steroids are dropped, then the patients seem to develop full-blown CSS. Perhaps it wasn’t related to the drug whatsoever, but it was related to change in treatment. Churg-Strauss can also present in people with quite mild asthma associated with allergic rhinitis, who then go on to develop lower vasculitic symptoms and the montelukast could be added in because it was presumed to be mild asthma. To these patients, we should always look at the benefits that can occur from increasing treatment, and this is just one thing that I think we should bring up for teaching aspect.
Dr. Gerard Cox:
Regarding to the management, I think he’s already having trouble with prednisone side effects since he’s mentioned having cataracts, gastritis, acne and fatty liver. So, these are already showing that he is at risk for more complications from steroids. Therefore we will be very interested in a drug other than prednisone to help control his disease. You have heard about a very good suggestion from Prof. O’Byrne about anti-IgE therapy. If that isn’t available to you and if intensive inhaled therapy isn’t sufficient, when we give somebody in this situation with difficult asthma, lung eosinophilia, or maybe another syndrome, we might often use methotrexate before we used cyclophosphamide, particularly for young patients. He is only 43, and we would worry about longer-term consequences of malignancy with somebody who was treated with oral cyclophosphamide for a long period of time. If you have to give him a nonsteroid drug to get away from prednisone and you don’t get biologic one available to you, methotrexate might be a cheap and economic way to get in there.
Final summarization
Dr. Paul O’Byrne:
Putting all things together, I think this man has severe refractory asthma with eosinophilia. I would optimize his inhaled treatment and would consider, at least think about omalizumab. When available, the patient will probably do very well with the anti-IL5 approaches such as mepolizumab, or benralizumab, which will be available very soon.
Dr. Nanshan Zhong:
I would like to make a summary of our discussions. Currently, the diagnosis should be considered as severe asthma rather than EGPA because there is no evidence of consolidation in the lung according to CT scan images, and no histological evidence of vasculitis and eosinophilic granuloma were found from the lung biopsies. However, the diagnosis of EGPA cannot be completely excluded. If eosinophilic infiltration can be found in other organs outside the lung, for example, stomach, eyes, or heart, then EGPA should be considered and further observation is needed. For treatment, cyclophosphamide should be used cautiously and oral steroid seems problematic due to the side effects. Additional inhaled corticosteroid such as budesonide should be considered. Meanwhile, the patient had a very high level of IgE, so the anti-IgE therapy might be useful. The management of allergic rhinitis should also be strengthened. Therefore, at this moment, we agree with your opinions and treat the patient following the direction of severe asthma. Xolair will be available very soon in China and we can try, but anti-IL5 is not available yet. We are going to follow up very carefully with this patient as well to monitor any change of eosinophilic infiltration in other organs and modify the diagnosis accordingly.
Acknowledgements
We would like to express our sincere gratitude to Dr. Hongyu Wang for her kind coordination on the Grand Round between GIRD and FIRH, as well as her diligent work on structuring and revising this paper. We are grateful to Dr. Qingling Zhang for providing the case, to Dr. Zheng Zhu, Dr. Ming Ding, Dr. Ruchong Chen for drafting the manuscript, to Dr. Jiaxing Xie and Dr. Zhengdao Lai for verifying the clinical case information, to Dr. Qingsi Zeng and Dr. Yu Deng for their radiological comments, to Dr. Yingying Gu for pathological comments, and to Prof. Rongchang Chen for his facilitating the organization of Ground Round, to Prof. Nanshan Zhong for his coordination during the Ground Round, to Prof. Paul O’Byrne, Prof. Gerard Cox and Prof. Andrew McIvor for their valuable comments on the case, to Prof. Martin Kolb for editing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hanania NA, Wenzel S, Rosén K, et al. Exploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA study. Am J Respir Crit Care Med 2013;187:804-11. [Crossref] [PubMed]



