Clinical implications of genetic heterogeneity in multifocal pulmonary adenocarcinomas
Multifocal lung cancers are being more commonly observed in clinical practice along with an increase in the use of computerized tomography (CT) scan and lung cancer screening (1). This is partly because patients with multifocal lung cancers do not necessarily present with symptoms related to metastatic disease. In fact, they are often asymptomatic at the time of diagnosis (2). It is well documented that some patients with multiple lung cancers with predominant ground glass opacity (GGO) continue to be asymptomatic for many years (3). GGO is a radiographic descriptive term, often defined as a focal area of increased lung attenuation on CT scan through which normal parenchymal lung structures (i.e., airways and vessels) can still be visualized. Lung cancers with a lepidic growth pattern can exhibit a GGO appearance because the tumor cells grow only along the alveoli, thus permitting aeration of the alveoli. It is well known that only one histological type of lung cancer can exhibit this growth pattern—adenocarcinoma.
Nevertheless, GGO does not necessarily mean adenocarcinoma since several pathological conditions can appear as GGO. GGO may correlate with minimally invasive adenocarcinoma (MIA), adenocarcinoma in situ (AIS) or atypical adenomatous hyperplasia (AAH) (4). The presence of a solid component in the GGO, however, is suggestive of the existence of invasive adenocarcinoma. Adenocarcinoma with GGO appearance has a tendency to manifest in a multifocal fashion. Over the years, many authors have documented several unique characteristics of multifocal adenocarcinomas. For instance, they tend to occur among female non-smokers and may exhibit a lower tendency for nodal or extra-thoracic metastasis than other types of lung cancer. The upcoming eight edition of American Joint Commission on Cancer (AJCC) staging for lung cancer recognizes multifocal adenocarcinoma as a unique disease entity and adopts the size of the largest nodule for staging. A letter “m” in parentheses will denote the multifocal nature of the disease (5). When several malignant lung nodules are found at the same time and they are of similar histology, it can be difficult to differentiate pulmonary metastatic disease from multiple primary lung cancers. However, when GGOs are seen in the nodules, multiple primary cancers are likely because GGOs are not characteristic of metastatic nodules. Indeed, one of the criteria to differentiate multiple primary lung cancers from pulmonary oligometastasis proposed by Martini and Melamed in 1975 is the presence of AIS component in each lesion (6). In a pooled analysis of 467 patients with resected presumed multiple lung cancers, those with all-adenocarcinoma histology had the best prognosis (7). In fact, the prognosis of these patients was numerically better than those who had multiple histological types: a situation in which the diagnosis of multiple primary lung cancers could not be questioned (8). Although the clinical, histological and biological characteristics of this entity have been well characterized, knowledge about its molecular characteristics has only just begun to emerge.
In a recent publication, Liu and colleagues shed new insights about molecular markers associated with multifocal adenocarcinomas, specifically regarding the pattern of epidermal growth factor receptor (EGFR) mutations (9). EGFR mutations are well characterized as a biomarker associated with targeted therapy. In 2004, a pivotal publication revealed that somatic mutations in the tyrosine kinase domain of the EGFR gene can increase growth factor signaling, leading to neoplastic proliferation (10). EGFR mutations in exons 18–21, highly predict tumor response to EGFR tyrosine kinase inhibitors (TKI), such as gefitinib, erlotinib, afatinib, and osimertinib. In the study by Liu et al., 78 patients with multifocal adenocarcinomas presenting as GGO were analyzed for EGFR mutations in exons 18–21. Each of these patients underwent surgery for removal of at least 2 independent GGO lesions. The concordance pattern of EGFR mutations in these resected multifocal adenocarcinomas of the lung was assessed. The investigators identified at least one EGFR mutation in at least one specimen in nearly 50% of patients. The analysis further showed that only 8% of patients with an EGFR mutation had an identical mutation identified in the paired specimen collected from another lesion. The authors concluded that the majority of multifocal adenocarcinomas seem to have arisen as independent events.
Although multiple studies have previously described the heterogeneity of molecular markers in multifocal adenocarcinomas (Table 1), the study by Liu and colleagues is the largest study to our knowledge. Some of these studies have examined not only the pattern of EGFR gene mutations, but also other gene mutations, such as in the KRAS gene or loss of heterozygosity as mechanisms to study the clonality of adenocarcinomas. It should be noted that the prevalence of EGFR mutations is highest among Asian populations and therefore are particularly useful for distinguishing tumor clonality in this population (15). Publications on multifocal adenocarcinomas from studies performed in Western countries report much lower EGFR mutation rates with less power to draw meaningful conclusions. For instance, in Germany (13) and USA (11), the observed EGFR mutation rates were only 7% and 5%. In these publications, the proportion of patients with apparent different clonality of cancers based on different mutations in different lesions varied widely from 31% to 75%. Of course, these numbers are dependent on the number of genes tested as well as the patient populations tested. Furthermore, comparison of these results may be confounded by methodological issues, such as differences in microdissection and tumor cellularity requirements. Low tumor cellularity can lead to a falsely negative result. Moreover, heterogeneity of the pathological lesion types included in the studies could further complicate data interpretation. Higher numbers of early or premalignant lesions such as MIA, AIS or AAH may lead to fewer EGFR mutations detected. It is well documented that the occurrence of mutations typically progresses over time, starting from premalignant lesion to invasive adenocarcinoma (16). Nevertheless, it can be concluded that a substantial proportion of patients with multifocal adenocarcinomas have multiple neoplastic clones with heterogeneous genetic alterations.
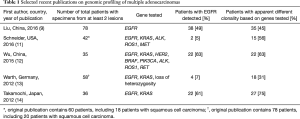
Full table
The observed heterogeneity of molecular markers has several important clinical implications. First, the finding has an implication for current biomarker testing practice for lung cancer. Typically, a diagnostic molecular marker test is performed once on one specimen per patient. However, for multifocal adenocarcinomas, multiple tests will need to be performed on multiple lesions to know for sure whether there are any actionable mutations in a given patient. For patients with many lesions, it remains unclear how many tests are needed to be performed on how many specimens to be sure. Furthermore, some testing algorithms which stop testing of different tumor sites for EGFR mutations whenever a KRAS mutation is discovered will need to be reconsidered. In general, KRAS and EGFR mutations are mutually exclusive (17). However, for patients with multifocal adenocarcinomas, a KRAS mutation may be present along with an EGFR mutation in a single patient due to the presence of multiple cancer clones (18). Molecular pathology laboratories need to be aware that multiple specimen(s) may be sent with a need for independent testing from a patient with multifocal adenocarcinomas. Lastly, there has been an increase in the use of liquid biopsy blood testing for detection of cancer molecular markers based on circulating tumor DNA. It remains unknown whether the most therapeutically relevant clone will show up in the blood of these patients and this warrants further studies.
Second is the implication for staging. Molecular pathology can be useful in differentiating multifocal adenocarcinomas from pulmonary metastases. Although morphological distinction can be helpful since there are several distinct morphological subtypes of adenocarcinomas, it may not be sufficient. Also, interpretation of morphology can be subjective and previous studies have documented disagreement among pathologists in difficult adenocarcinoma cases (19). Therefore, characteristic molecular markers can provide additional critical information for characterizing the relationship between different lesions. Difference in patterns of markers in different lesions supports the existence of multiple primary cancers. This can change the staging of such patients and influence treatment options. Currently, the upcoming AJCC staging adopts a broad language regarding the use of molecular pathology for staging of lung cancer. Additional studies will be needed to standardize and improve the integration of molecular testing into practice for lung cancer staging.
Third is the implication for treatment. Although surgery is the mainstay of multiple primary lung cancers, some cases may be inoperable or may not be amendable to surgery. In this scenario, systemic therapy is the treatment of choice. Systemic therapy in the form of chemotherapy, TKI, or immunotherapy can be considered. For TKI, the genetic heterogeneity of multifocal adenocarcinomas may pose a challenge to achieve a control of disease in all cancer sites. For instance, in the paper by Liu and colleagues, 38 of 78 patients of Asian descent (48.7%) had an EGFR mutation in at least one lesion, but 23 of these 38 patients were also wild type for EGFR in a different lesion, leaving only 15 of 78 patients (19.0%) with EGFR mutations in all lesions. Given the fact that TKI therapy does not inhibit growth in lesions that lack EGFR mutations, it can be inferred that only the 19.0% subset of these patients with EGFR mutations in all lesions has a chance for control of disease in all sites. On the other hand, given the practical point that it may not be feasible to perform a biopsy on all of the lesions for patients with multifocal adenocarcinomas, it is possible that there is an actionable mutation left undetected and therefore, therapeutic opportunity with TKI, albeit partial benefit at best, may be missed. Would an empirical treatment with various TKIs be justified? This is relevant for the current state of practice with EGFR TKI use in the United States now restricted only for patients with a proven EGFR mutation. Such restriction of EGFR TKI may pose an unfortunate disadvantage to obtain a palliative benefit among patients with multifocal adenocarcinomas whose molecular testing was not aggressively pursued, especially among patients with Asian descent in whom the prevalence of EGFR mutations may be in excess of 50%.
In conclusion, the marked genetic heterogeneity between multifocal adenocarcinomas in the same patient can be useful to document different tumor clones. EGFR analysis of multiple tumor sites is particularly informative among people with Asian ancestry due to the relatively high prevalence of EGFR mutations in this population. The work by Liu and colleagues further lays the framework for future research to exploit the richness of molecular aberrations in this unique subtype of lung cancer.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vazquez M, Carter D, Brambilla E, et al. Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 2009;64:148-54. [Crossref] [PubMed]
- Garfield DH, Cadranel JL, Wislez M, et al. The bronchioloalveolar carcinoma and peripheral adenocarcinoma spectrum of diseases. J Thorac Oncol 2006;1:344-59. [Crossref] [PubMed]
- Dumont P, Gasser B, Rougé C, et al. Bronchoalveolar carcinoma: histopathologic study of evolution in a series of 105 surgically treated patients. Chest 1998;113:391-5. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Detterbeck FC, Marom EM, Arenberg DA, et al. The IASLC Lung Cancer Staging Project: Background Data and Proposals for the Application of TNM Staging Rules to Lung Cancer Presenting as Multiple Nodules with Ground Glass or Lepidic Features or a Pneumonic Type of Involvement in the Forthcoming Eighth Edition of the TNM Classification. J Thorac Oncol 2016;11:666-80.
- Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg 1975;70:606-12. [PubMed]
- Tanvetyanon T, Finley DJ, Fabian T, et al. Prognostic nomogram to predict survival after surgery for synchronous multiple lung cancers in multiple lobes. J Thorac Oncol 2015;10:338-45. [Crossref] [PubMed]
- Tanvetyanon T, Finley DJ, Fabian T, et al. Prognostic factors for survival after complete resections of synchronous lung cancers in multiple lobes: pooled analysis based on individual patient data. Ann Oncol 2013;24:889-94. [Crossref] [PubMed]
- Liu M, He WX, Song N, et al. Discrepancy of epidermal growth factor receptor mutation in lung adenocarcinoma presenting as multiple ground-glass opacities. Eur J Cardiothorac Surg 2016;50:909-913. [Crossref] [PubMed]
- Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004;350:2129-39. [Crossref] [PubMed]
- Schneider F, Derrick V, Davison JM, et al. Morphological and molecular approach to synchronous non-small cell lung carcinomas: impact on staging. Mod Pathol 2016;29:735-42. [Crossref] [PubMed]
- Wu C, Zhao C, Yang Y, et al. High Discrepancy of Driver Mutations in Patients with NSCLC and Synchronous Multiple Lung Ground-Glass Nodules. J Thorac Oncol 2015;10:778-83. [Crossref] [PubMed]
- Warth A, Macher-Goeppinger S, Muley T, et al. Clonality of multifocal nonsmall cell lung cancer: implications for staging and therapy. Eur Respir J 2012;39:1437-42. [Crossref] [PubMed]
- Takamochi K, Oh S, Matsuoka J, et al. Clonality status of multifocal lung adenocarcinomas based on the mutation patterns of EGFR and K-ras. Lung Cancer 2012;75:313-20. [Crossref] [PubMed]
- Steuer CE, Behera M, Berry L, et al. Role of race in oncogenic driver prevalence and outcomes in lung adenocarcinoma: Results from the Lung Cancer Mutation Consortium. Cancer 2016;122:766-72. [Crossref] [PubMed]
- Yatabe Y, Takahashi T, Mitsudomi T. Epidermal growth factor receptor gene amplification is acquired in association with tumor progression of EGFR-mutated lung cancer. Cancer Res 2008;68:2106-11. [Crossref] [PubMed]
- Tam IY, Chung LP, Suen WS, et al. Distinct epidermal growth factor receptor and KRAS mutation patterns in non-small cell lung cancer patients with different tobacco exposure and clinicopathologic features. Clin Cancer Res 2006;12:1647-53. [Crossref] [PubMed]
- Ye C, Wang J, Li W, et al. Novel Strategy for Synchronous Multiple Primary Lung Cancer Displaying Unique Molecular Profiles. Ann Thorac Surg 2016;101:e45-7. [Crossref] [PubMed]
- Stang A, Pohlabeln H, Müller KM, et al. Diagnostic agreement in the histopathological evaluation of lung cancer tissue in a population-based case-control study. Lung Cancer 2006;52:29-36. [Crossref] [PubMed]


