Optimizing the exposure in minimally invasive mitral surgery: a new left atrial retractor system
Introduction
Since Lillehei and colleagues report concerning the first case of mitral valve repair dated back 1957, using femoral artery cannulation for cardiopulmonary bypass (CPB) and approaching the mitral valve through a right thoracotomy, minimally invasive techniques have progressively challenged traditional approaches in cardiothoracic surgery (1). Accordingly, minimally invasive surgery (MIS) has been increasingly accepted in the surgical community as an alternative to conventional sternotomy, with the advantages of a reduced trauma, fewer blood transfusions, fewer septic wound, a shorter recovery time, improved functional recovery, and a better cosmetic result. In addition, MIS has shown in some reports to improve post-operative respiratory function and reduce post-operative pain, blood loss and blood transfusion related to minimal surgical dissection (2). Some limited reports indicated an improvement in the incidence of postoperative renal failure and rate of post procedural atrial fibrillation (3). Right from the start, it has been clear that to perform a safe, easy and effective procedure, through such small surgical access, a proper and accurate visualization of the mitral valve is essential. The main goal is to achieve an excellent exposure in order to reproduce all surgical technique performed through a standard access; particularly regarding mitral repair strategy. An appropriate exposure of the left atrium is crucial for a successful and durable mitral valve repair or replacement. The small surgical access makes mandatory a perfect retraction of the cardiac chamber allowing a complete visualization of the entire annulus, the leaflets and sub-valvular apparatus of the mitral valve. To achieve optimal exposure, “ad hoc” atrial retractors are used. The adoption of video assistance during the procedure, particularly with a full HD or 3D system, consents visualization, illumination and magnification. Its use has been advocate also during standard procedures (4-6).
The aim of this paper is to provide an overview of the state of the art on the current available devices for the exposure of the left atrial chamber in the setting of minimally invasive mitral surgery.
State of art
In the full sternotomy approach, mitral valve exposure is obtained with a retractor handled by the assistant or attached to the sternal retractor. To improve the visualization of the mitral valve, a retracting arm, secured with a side crossbar to the sternal retractor, is seldom used (7).
During mitral MIS, an optimal exposure is crucial due to the smaller working port and the reduced field where surgical instruments move. Even with the support of video assistance able to allow an optimal visualization of the whole mitral valve apparatus, a correct exposure during MIS procedures is mandatory and represent a key step of the set up. In order to improve the exposure and facilitate the surgical maneuvers, different atrial retractors have been designed over the years (8-10).
Currently, atrial retractors are divided in Trans Working Port or Trans Thoracic.
Trans-working-port retractors
The trans-working port retractors are designed to be positioned through the working port, without the need of a supporting bar through the chest wall. This brings advantages, first, avoiding an additional incision in the intercostal space with the risk of vessels injuries. Trans-working-port retractors are more versatile because the blade can be placed anywhere due to the flexible movement of the shaft.
A drawback of this system is related to his position through the working port; this necessarily reduces the direct vision area and the movement of surgical instruments, making the use of the camera indispensable for all the steps of the procedure. The presence of the different bars of support around the working port represents a risk of locking the sutures. In addition, in case of deep surgical field, with the mitral plane far from the chest, an appropriate retraction is not possible through a small incision due to the “conflict” between the retractor and the chest wall. In truth Trans working-port, atrial retractors are not practical in case of very small surgical access like in port-access surgery.
To avoid further impairment through the working port, a different retractor concept has been developed. The MitraXS, (Cardio Life Research, Louvain la Nueve, Belgium) made of a polycarbonate sheet, is a self-expanding, pliable, left atrial retractor that may be easily inserted in the atrium from the mini-thoracotomy, and does not require any supporting arm. It gently retracts the atrial walls, creating a conical space, which leaves a free 1-cm rim of atrial muscle all around the mitral annulus, protecting atrial wall by accidental damage but providing little space for suturing. Furthermore, this kind of retraction may increase the risk of injury of aortic cusps and left ventricular outflow tract, because the mitral annulus is pushed toward the interventricular septum (11,12).
Trans-thoracic wall retractor
Generally, the trans-thoracic wall retractor provides very stable mitral valve exposure because it has a system, which fixes the bar of the retractor trough the chest wall. Although this instrument provides surgeons with stable exposure of the mitral valve, this kind of system also carries the potential risk of injury to the mammary or intercostal vessels during insertion of the bar. Using a more lateral mini-thoracotomy, far-off from the sternum, is recommended to avoid this undesirable/unwanted complication.
Alternatively, an additional holder arm (pneumatic, mechanic or electric) is used, and fixed to the surgical bed pulling up the supporting bar himself and the blade. They can feature, in addition, a self-adjusting pivot blade with or without an adjustable angle mechanism or a self-wiping hinge. The device (bar) is usually inserted through the fourth intercostal space, 2–4 cm medial to the internal commissure of the working port. The blade itself is hinged and has an adjustable angle system that provides great exposure regardless of any anatomic variance. In other devices, an additional lateral blade may be used to retract the left atrial wall at the posterior-medial commissural area of the mitral valve. This lateral “wing” is placed and fixed, with a special screwdriver, by the surgeon in order to push away the lateral wall of the left atrium.
To achieve a reproducible and satisfactory exposure, sufficient knowledge, skill and experience with the instrument is necessary because the shaft position itself can affect surgeon’s view.
With the trans-thoracic system, the working port remains free of obstacle, reducing therefore the risk for the suture to lock around the working port and any other “conflicts” with the instruments.
Among transthoracic retractor, we have to mention the robotic mitral valve procedure. With this approach the surgeon operate through a ½ inch port incision, made through the right chest wall, utilizing the magnified view of the mitral valve provided by the robotic camera. In these cases the use of a transthoracic retractor is mandatory and it is crucial an accurate sizing due to the small surgical field and the risk of conflict between the retractor and the robotic arms.
New concept
In the current setting for MIS with the available devices, the retraction of the left atrium is not always ideal because of several technical aspects:
- First of all, the atrium often is not completely open, especially the postero medial portion of the wall;
- As a consequence the inter atrial septum may collapse into the cavity.
The latter condition makes the complete visualization of the mitral valve very challenging, both in direct vision as well as through video-assisted visualization. Particularly the most tricky area is the posterior-medial commissure, between A3 and P3 that is often completely covered by the atrial wall.
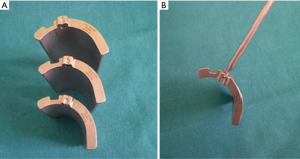
We present a new device recently commercialised (Karl Storz GmbH, Tuttlingen, Germany), characterized by asymmetric and curved shape, allowing in one movement, to retract both the superior and postero medial aspect of the left atrium and to push away the lateral wall of the chamber. Different sizes are available (from 4.5 cm × 5 cm to 6.5 to 5 cm) depending on the atrial volume; in addition, it is possible to use a blade with several degree of curvature to push out the lateral wall of the atrium. (Figure 1A) The blade extend to the right the cavity allowing a complete exposure of the anatomy of the valve. A metal bar hold as usual the blade and is fixed through the chest using a holder system (Figure 1B).
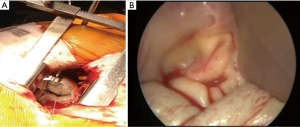
Blade retractor insertion is extremely easy; it can be inserted using the holder arm or forceps. The curved and asymmetric shape of the blade is easily inserted through the thoracotomy and retracts broadly the atrium. (Figure 2A) Direct or video assisted view is easily achieved through the working port allowing a comfortable mitral operation. The retractor does not need any additional manoeuvres to push the lateral wall of the atrium. It covers around 3/5 of the atrium surface expanding completely the chamber and allowing easily movements inside. Once the procedure is completed, it can be easily removed in one single and not time-consuming manoeuvre.
Methods
The effectiveness of this retractor was evaluated in 40 patients undergone minimally invasive mitral surgery in the last 2 years. Patients provided informed consensus to the use of this device. There were 18 female and 22 male patients with a mean age of 60±15 years and a EuroSCORE II of 2.6±1.9. The procedure was a redo in two cases. The origin of mitral valve lesions was rheumatic in 9 patients, degenerative in 28 patients, endocarditis in 1 patients, and bio-prosthesis dysfunction in 2 patients.
The device has been successfully used for both mitral valve repair (n=30) and replacement (n=10). Moreover the exposure resulted optimal, with a mean placement time of 40±15 seconds and an optimal surgical field for all the mitral repair techniques; we principally performed the repairs with ring implantation and posterior leaflets resection (80%). Mean CPB and clamping time were 110±15 minutes and 65±20 minutes. With this device, mitral ring or prosthesis insertion is extremely handy and we did not have any case of dislodgement of the device during the procedure. We did not report any case of mammary artery injury or atrial tear during insertion or retraction. Valve visualization was easily achieved both under direct vision and through video assisted approach (Figure 2A).
We didn’t observe an increased rate of repair with the new device if compared with the previous retraction system but an optimal exposure was obtained at the first attempt with no need of further repositioning the device or need for additional stiches during the procedure to further improve visualization.
We didn’t observe any distortion of the valve anatomy, allowing the analysis of valve dysfunction very easy and reliable in all repair procedures (Figure 2B).
Those results were compared with the results we obtained with the use of a standard left atrial retractor and we didn’t obtained a statistically significant difference in CPB and X clamp time, but the simplicity of the insertion made the exposure of the valve very slick.
For patient that had a repair the echocardiogram at the time of discharge showed no residual mitral regurgitation in 18 patients (60%), trivial regurgitation in 8 patients (26.7%) and mild regurgitation in 4 patients (13.3%). For the patients that had a replacement, 1 patient out of 10 was found with a para valvular leak (10%).
Discussion
MIS valve surgery allows enormous advantages in terms of faster recovery after operation as well as reduction of some of the complications in cardiac surgery. Nevertheless, since an optimal exposure of the mitral valve is the first step to achieve in MIS, there is an increased need for dedicated tissue retractors that can be deployed and maneuvered through smaller incisions. Moreover, we think is mandatory to achieve the same number in terms of performed mitral repairs and long terms results in comparison of standardised surgical procedures validated during the last two decades. Minimize the length of skin incision; achieving at the same time an optimal visualization of the whole mitral valve apparatus in order to perform mitral valve operation, encompassing various repair techniques is thus the only way to really compete with standard surgical techniques. Video assistance and the concept of specialized atrial retractors have obvious and non-negligible theoretical and applicative implications in several surgical scenarios strongly supporting us toward this way.
Conclusions
This new atrial retractor for minimally invasive mitral surgery (Karl Storz GmbH, Tuttlingen, Germany) is easy to use with an excellent efficacy in terms of visualization, exposure and surgical access to the mitral valve as compared to conventional retractors. Since testing the device, we have embraced its use in most of our MIS procedures. According to our experience and the results of this series, this retractor makes the technique of MIS easier and more reproducible.
We strongly believe this new atrial retractor could represent a new tool able to let an optimal surgical exposure helping several surgeons in their daily clinical practice. Of course, future studies are encouraged to test this retractor and confirm our results.
Acknowledgements
None.
Footnote
Conflicts of Interest: Prof E. Greco is co-inventor of the patent related to the mitral retractor of Karl Storz GmbH, Tuttlingen, Germany.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Lillehei CW, Gott VL, Dewall RA, et al. Surgical correction of pure mitral insufficiency by annuloplasty under direct vision. J Lancet 1957;77:446-9. [PubMed]
- Chirichilli I, D'Ascoli R, Rose D, et al. Port Access (Thru-Port System) video-assisted mitral valve surgery. J Thorac Dis 2013;5 Suppl 6:S680-5. [PubMed]
- McCreath BJ, Swaminathan M, Booth JV, et al. Mitral valve surgery and acute renal injury: port access versus median sternotomy. Ann Thorac Surg 2003;75:812-9. [Crossref] [PubMed]
- Greco E, Zaballos JM, Alvarez L, et al. Video-assisted mitral surgery through a micro-access: a safe and reliable reality in the current era. J Heart Valve Dis 2008;17:48-53. [PubMed]
- Greco E, Mestres CA, Cartañá R, et al. Video-assisted cardioscopy for removal of primary left ventricular myxoma. Eur J Cardiothorac Surg 1999;16:677-8. [Crossref] [PubMed]
- Ruvolo G, Speziale G, Bianchini R, et al. Combined coronary bypass grafting and mitral valve surgery: Early and late results. Thorac Cardiovasc Surg 1995;43:90-3. [Crossref] [PubMed]
- Cosgrove DM. A self-retaining retractor for mitral valve operations. J Thorac Cardiovasc Surg 1986;92:305-6. [PubMed]
- Okamoto K, Yozu R. Designing innovative retractors and devices to facilitate mitral valve repair surgery. Ann Cardiothorac Surg 2015;4:364-9. [PubMed]
- Yozu R, Okamoto K, Kudo M, et al. New innovative instruments facilitate both direct-vision and endoscopic-assisted mini-mitral valve surgery. J Thorac Cardiovasc Surg 2012;143:S82-5. [Crossref] [PubMed]
- Ishikawa N, Sun YS, Nifong LW, et al. Port-access atrium retractors for totally endoscopic mitral valve surgery: theTornado Retractor, the Butterfly Retractor, and the Semiautomatic Butterfly Retractor. Surg Endosc 2008;22:2088-90. [Crossref] [PubMed]
- Murzi M, Solinas M, Bevilacqua S, et al. A new left atrial retractor for minimally invasive mitral valve surgery. J Card Surg 2009;24:175-7. [Crossref] [PubMed]
- Jegaden O, Sassard T, Shafy A, et al. Evaluation of a new left atrial retractor for minimally invasive mitral valve surgery. J Thorac Cardiovasc Surg 2011;141:297-9. [Crossref] [PubMed]


