Unusual cause of massive hemothorax: spontaneous rupture of nonfunctioning mediastinal paraganglioma
Introduction
Mediastinal paraganglioma is a rare neurogenic tumor that originates from paraganglia, which can either be functional when catecholamine is secreted or nonfunctional. Most nonfunctional mediastinal paraganglioma are usually found incidentally. This paper reports a case of spontaneous rupture of nonfunctional mediastinal paraganglioma, which causes massive hemothorax. Fortunately, the patient has finally received a successful complete resection.
Case presentation
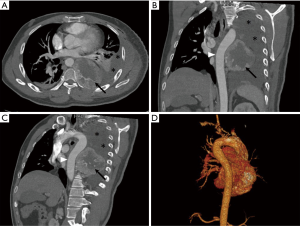
A 39-year-old man was admitted to our department for posterior mediastinal tumor with spontaneous hemothorax in the left thorax. The man underwent emergency surgical thoracic exploration because of an unexplained hemothorax in another hospital a week ago. During the operation, a ruptured nourishing vessel in the surface of the mediastinal tumor was found. However, the radical surgery was abandoned due to the large size and rich nourishing vessels of the tumor, and just a simple surgical ligation of ruptured vascular was performed to stop the bleeding. The patient had a clinical history of cartilage synovioma resection in the left hip joint eight years ago. He did not have hypertension, heart disease, and hidrosis. An enhanced computed tomography (CT) of the chest before second operation revealed an 8 cm × 8 cm posterior mediastinal tumor with uneven density on the left side of the vertebrae (Figure 1A,B,C, arrows) and a moderate amount of pleural effusion (Figure 1A,B,C, asterisks). The thoracic aorta was tortuous due to tumor compression (Figure 1B,C, arrowheads). The three-dimensional (3-D) reconstruction of heart and aorta revealed no obvious nourishing blood vessels of tumor arose from the thoracic aorta (Figure 1D). The patient was treated with intravenous hemostatics (aminomethylbenzoic acid and etamsylate) for a week. After systemic evaluation, the hemothorax of the patient stabilized and the routine blood examination results were normal. Subsequently, the second thoracotomy was performed through the original incision. Intraoperatively, an 8 cm × 8 cm encapsulated, highly vascular tumor located in the posterior mediastinum without active bleeding was found after the hematocele in the thorax was cleared. The tumor had invaded the chest wall and had adhered to the thoracic aorta. Finally, a complete resection of the tumor with the partial parietal pleura was performed after the careful separation and ligation of the nourishing vessels.
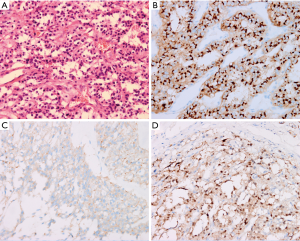
Histologically, the tumor comprised cells arranged in nests (“Zellballen”) with vascular stroma (Figure 2A). Immunohistochemistry analysis revealed that chromogranin, synaptophysin, and S-100 protein were highly expressed (Figure 2B,C,D), but epithelial membrane antigen and pan-cytokeratin were negative in the tumor. The patient was finally diagnosed with nonfunctional mediastinal paraganglioma.
Discussion
Paraganglioma is a kind of rare neuroendocrine tumor that originates from the paraganglia. The most common location of this tumor is the head, neck, and retroperitoneum. Mediastinum paraganglioma are uncommon, accounting only for 2% of all cases (1). According to its ability to synthesize and release catecholamines, paraganglioma is classified as either functional or nonfunctional.
Most of the mediastinal paraganglioma are nonfunctional, asymptomatic, and usually found incidentally. In our case, hemothorax as the first manifestation occurred in the patient because of the spontaneous rupture of the tumor. To our knowledge, this is the first reported case of spontaneous rupture of nonfunctioning mediastinal paraganglioma to date, although a rare similar condition has been reported in other sites (2).
Ruptured phaeochromocytomas are more frequently reported in the literature due to the hypersecretion of catecholamines. However, the pathogenesis of spontaneous rupture of nonfunctioning paraganglioma is unclear, and the potential for the complication may be associated with some factors including the highly vascular nature and the ischemic necrosis resulted from growth too fast.
Regarding the diagnosis of mediastinal paraganglioma, CT and magnetic resonance imaging (MRI) are useful imaging methods, providing information about the location and size of lesions. Because mediastinal paraganglioma are hypervascular tumors that can exhibit remarkable contrast agent enhancement on CT or MRI. Based on the hypervascular feature, transthoracic needle biopsy is not recommended for preoperative diagnosis because this process may cause catastrophic bleeding (3).
According to some research, the behavior of mediastinal paraganglioma presents the characteristics of a malignant tumor, including invading the adjacent mediastinal organs and distant metastasis. Complete resection is the preferred treatment for mediastinal paraganglioma. Nevertheless, the highly vascular nature of these tumors also brings huge surgical risks. Massive bleeding during tumor excision has been reported (4). Therefore, preoperative angiography is recommended to evaluate the tumor vascular supply. Preventive embolization can reduce perioperative bleeding if necessary.
In some cases, when the tumor location is close to the heart or major vessels, or the tumor directly invades these structures, cardiopulmonary bypass is also adopted to ensure a safe operation. But even so, the rate of complete resection of mediastinal paraganglioma is only 76.9% (5). Fortunately, the majority of patients who underwent successful resection has a favorable prognosis with no evidence of recurrence.
In conclusion, the spontaneous rupture of mediastinal paraganglioma is an unusual cause of hemothorax. This rare condition should be suspected when a large mediastinal mass accompanied with pleural effusion is found in CT images. Complete resection is the preferred treatment for mediastinal paraganglioma, and most mediastinal paraganglioma patients experience favorable prognosis after complete resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Abad C, Jiménez P, Santana C, et al. Primary cardiac paraganglioma. Case report and review of surgically treated cases. J Cardiovasc Surg (Torino) 1992;33:768-72. [PubMed]
- Yau KK, Siu WT, Li MK. Unusual cause of acute abdomen --- ruptured retroperitoneal paraganglioma. Asian J Surg 2008;31:32-5. [Crossref] [PubMed]
- Boulogianni G, Chourmouzi D, Sivitanidis E, et al. An incidental nonfunctioning mediastinal paraganglioma (2009: 11b). Aorticosympathetic paraganglioma. Eur Radiol 2010;20:506-9. [Crossref] [PubMed]
- Lin MW, Chang YL, Lee YC, et al. Non-functional paraganglioma of the posterior mediastinum. Interact Cardiovasc Thorac Surg 2009;9:540-2. [Crossref] [PubMed]
- Brown ML, Zayas GE, Abel MD, et al. Mediastinal paragangliomas: the mayo clinic experience. Ann Thorac Surg 2008;86:946-51. [Crossref] [PubMed]


