Effects of recombinant human brain natriuretic peptide on the prognosis of patients with acute anterior myocardial infarction undergoing primary percutaneous coronary intervention: a prospective, multi-center, randomized clinical trial
Introduction
Primary percutaneous coronary intervention (PCI) is the current internationally preferred treatment for acute myocardial infarction (AMI) (1). Although some patients received PCI within the effective time window after onset, there was no obvious decrease in the in-hospital mortality rate and major complications in AMI patients in China for the past 10 years. The in-hospital mortality rate was within 5–15% (2). Therefore, further investigations are warranted to optimize its therapeutic benefits for AMI and develop novel therapies to decrease the mortality rate of AMI.
Brain natriuretic peptide (BNP) is a 32-amino-acid ring-shaped polypeptide that increases the urinary excretion of water and sodium, relaxes blood vessels and inhibits sympathetic activity (3-7). Since its use as a drug for heart failure in 2001 (8), recombinant human brain natriuretic peptide (rhBNP) has been increasingly used for the treatment of AMI, accompanied by cardiac insufficiency. Thereafter, several clinical trials (9-12) have reported that intravenous rhBNP after AMI onset, even if accompanied by cardiac insufficiency, reduced myocardial infarct size, improved cardiac function and reduced major adverse cardiac events (including cardiac death). Many studies conducted by Chinese groups regarding the therapeutic effects of rhBNP on AMI have been reported, but most of these studies were single-center trials with a small sample size. Hence, randomized controlled clinical trials that involve a large sample size are needed to investigate its applicability, drug use time and dose, and its precise clinical efficacy and safety of rhBNP for the treatment of AMI. In this multi-center randomized controlled study, we investigated the effects of intravenously administering rhBNP during the early stage after PCI on serum enzyme data, cardiac function parameters and cardiovascular events in patients with acute anterior myocardial infarction (MI), aiming to determine the prognostic value of rhBNP in AMI.
Methods
Subjects
A total of 421 patients with acute anterior or extensive anterior MI, who underwent PCI between October 2012 and August 2014, were collected from 20 Chinese hospitals and included into this study. Inclusion criteria: within 12 hours after onset (or with permanent ischemic symptoms despite being over 12 hours after onset), patients within 18–75 years of age, patients of either gender, and patients who provided a signed written informed consent. The diagnosis of acute anterior or extensive anterior MI is defined as the detection of the increase in cardiac biomarker values [creatine kinase-MB (CK-MB) or cardiac troponin (cTnT)] with at least one value above the 99th percentile upper reference limit (URL) and with at least one of the following: (I) symptoms of ischemia; (II) new or a presumed new significant ST-segment elevations in leads V1–V5 with or without elevations in leads V6, I and aVL; (III) the presence of pathological Q waves in these leads; (IV) imaging evidence of new regional anterior wall motion abnormality (13). Exclusion criteria: previous history of coronary artery bypass surgery; complicated by acute inferior and/or posterior and/or right ventricular MI; cardiogenic shock or systolic blood pressure ≤90 mmHg after the use of vasopressor agents; mechanical complications (perforation of ventricular septum, rupture of the mitral chordae tendineae); severe hepatic and renal inadequacy; suspected aortic dissection; a previous history of MI; a previous history of rheumatic heart valve disease, cor pulmonale or hypertrophic obstructive cardiomyopathy; patients with diseases that influence prognosis such as acute inflammation and malignant tumors.
Design/grouping
This study is a prospective, multi-center, randomized controlled clinical trial approved by the Ethics Committee of The People’s Hospital of Liaoning Province (No. 2011-01-003). All patients included in this study provided a written informed consent. The included patients were randomly divided into two groups: the rhBNP group and control group (the same surgical procedure without the use of rhBNP). Diagnostic criteria and routine medication were performed in strict accordance with the Clinical Guidelines for the Diagnosis and Treatment of ST-Segment Elevation MI (14). Patients in the rhBNP group did not receive intravenous nitrate during the rhBNP treatment period. The patient’s physician determined whether intravenous nitrate was used after rhBNP withdrawal, including the drug type, dose and course of treatment. Furthermore, the patient’s physician also determined whether angiotensin converting enzyme inhibitors (ACEIs) were used 24 hours after rhBNP, including the drug type, dose and course of treatment. Patients in the control group received the treatment protocol created by physicians, including intravenous nitrate (nitroglycerin or isosorbide dinitrate injection) and oral ACEI. Interventional therapy and a manipulation strategy were performed in accordance with China’s Guidelines for Percutaneous Coronary Artery Treatment in 2012 (15). Sample size was evaluated according to the change in amplitude of the left ventricular ejection fraction (LVEF) value. At postoperative 6 months, if the difference in LVEF value between the two groups was 3%, with a standard deviation (SD) of 9%, an error alpha of 0.05, and a beta of 0.10 (i.e., 1-β=0.90), the calculated sample size required for each group would be 189. If the expulsion rate of 10% was considered, the sample size would be 208. Thus, 416 patients should be included into the study.
Randomization: grouping and numbering were performed randomly. In brief, each serial number and group name were written in a piece of paper and sealed in envelopes. Then, these envelops were randomly selected by each center. In each center, patients were grouped according to the information written on the paper prior to emergent interventional therapy. Patients who could not undergo interventional therapy due to various causes were rejected. These were performed until the sample size reached 208 patients per group. Finally, 213 patients were included in the rhBNP group and 208 patients were included in the control group.
rhBNP dose and administration
In the rhBNP group, rhBNP (Approval No. S20050033; Chengdu Nuodikang Biological Pharmaceutical Co., Ltd., Chengdu, Sichuan Province, China) was used as early as possible after admission, which was applied not later than 2 hours after interventional therapy. One ampoule of rhBNP (0.5 mg) was dissolved with 50 mL of liquid (5% glucose solution or 0.9% NaCl). Its recommended use is 0.01 µg/kg per minute. This treatment lasted for 72 hours. Blood pressure was measured once every 15–20 minutes within the first 2 hours of medication and once every one or 2 hours thereafter. After 24 hours, blood pressure was measured based on the degree of disease stabilization. If blood pressure could not be stabilized, rhBNP dose was appropriately reduced until withdrawal. The rhBNP dose was appropriately increased when obvious heart failure symptoms appeared.
Outcome measures and follow-up observation
The primary endpoint outcome was the LVEF value, which was determined by two-dimensional Doppler echocardiography with the Simpson method at postoperative 6 months. All measurements were taken by two experienced sonographers in each center, who were blinded to the trial groupings. Furthermore, all sonographers undertook a joint training to reduce measuring errors. Secondary endpoint outcomes included serum concentrations of cTnT, CK-MB isoenzyme, and N-terminal pro-brain natriuretic peptide (NT-proBNP), and echocardiographic parameters at postoperative days 1–7, as well as echocardiographic parameters at postoperative 6 months, and the major adverse cardiac events that would occur within 6 months after the procedure. This includes possible or diagnosed ventricular fibrillation, cardiac death, relapsed angina pectoris or MI, and acute left heart failure.
- The primary indices were measured or recorded as follows: baseline data: gender, age, body weight, infarct region, baseline blood pressure, heart rate and coronary heart disease risk factors, and the type and dose of the major drugs used;
- Interventional therapy data: coronary angiography data, the target diseased region and imaging features, procedures and results of interventional therapy, material brand and dose, and drug use and patient vital signs;
- Prior to interventional therapy: serum concentrations of cTnT, CK-MB and NT-proBNP; hepatic and renal function; serum ions; 18-lead electrocardiogram; Killip classification;
- At postoperative day 1: serum concentrations of cTnT and CK-MB; 12-lead electrocardiogram;
- At postoperative day seven or prior to discharge: serum concentrations of cTnT, CK-MB and NT-proBNP and renal function; stroke volume (SV) measured by two-dimensional Doppler echocardiography, left ventricular end-diastolic diameter (LVEDd) and LVEF;
- At postoperative 6 months: SV, LVEDd and LVEF were measured by two-dimensional Doppler echocardiography; the incidence of major adverse cardiac events was evaluated.
Statistical analysis
Measurement data are expressed as mean ± SD, and were statistically analyzed using one-way analysis of variance, paired t-test and independent samples t-test. Count data were expressed as frequency, and were analyzed using the Chi-squared test. P<0.05 was considered statistically significant. All statistical analyses were performed using SPSS 15.0 software (SPSS, Chicago, IL, USA).
Results
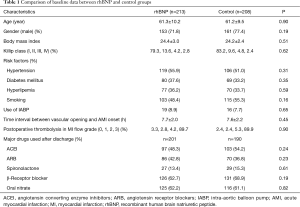
Comparison of baseline data between the rhBNP and control groups
There were no statistically significant differences in age, male/female ratio, body weight, Killip classification, intra-aortic balloon pump application, time interval between infarction-related vascular opening and AMI onset, and postoperative thrombolysis in MI flow grade between the rhBNP and control groups. There was also no significant difference in the use of drugs [ACEIs, angiotensin receptor blockers (ARB), spironolactone, β-receptor blocker or nitrate] between the rhBNP and control groups (Table 1). Nearly all included patients used aspirin, clopidogrel, ticagrelor, or statins (data not shown).
Full table
rhBNP use and blood pressure change
In the rhBNP group, the time interval between the use of rhBNP and AMI onset was 6.8±2.0 hours (3.5–14.0 hours); and rhBNP use lasted for 48.8±16.4 hours (3.0–87.0 hours). In the rhBNP group, rhBNP dose was reduced in 17 (8.0%) patients due to unstable blood pressure, and nine (4.2%) patients withdrew from rhBNP use due to hypotension. In the control group, 13 (6.3%) patients did not use or withdrew from intravenous nitrate use due to unstable blood pressure.
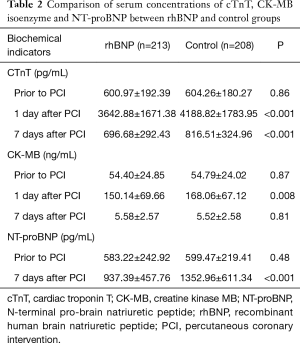
Comparison of serum enzyme data between the rhBNP and control groups
There were no significant differences in serum concentrations of cTnT and CK-MB prior to PCI between the rhBNP and control groups. At postoperative day one and seven, serum concentrations of cTnT were significantly lower in the rhBNP group than in the control group (P<0.001). At postoperative day one, serum concentrations of CK-MB were significantly lower in the rhBNP group than in the control group (P=0.008, Table 2).
Full table
Comparison of serum concentrations of NT-proBNP between the rhBNP and control groups
There was no significant difference in serum concentrations of NT-proBNP between the rhBNP and control groups. At postoperative day seven, serum concentrations of NT-proBNP were significantly lower in the rhBNP group than in the control group (P<0.001, Table 2).
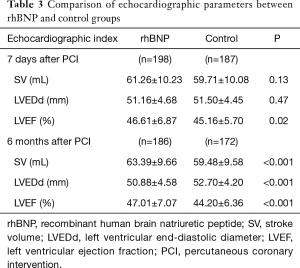
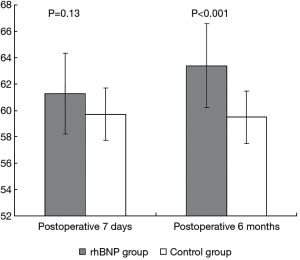
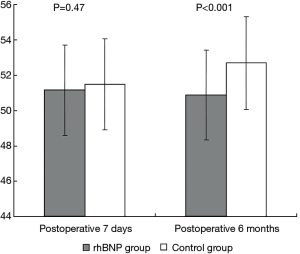
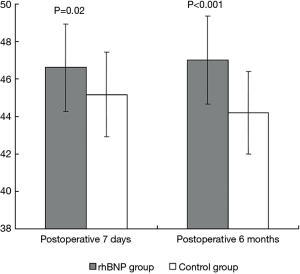
Comparison of echocardiographic parameters between the rhBNP and control groups
There was no significant difference in SV and LVEDd between the rhBNP and control groups at postoperative day seven. However, LVEF was significantly greater in the rhBNP group than in the control group (P=0.02). At postoperative 6 months, LVEDd was significantly lower in the rhBNP group than in the control group (P<0.001), and SV and LVEF were significantly greater in the rhBNP group than in the control group (both P<0.001; Table 3, Figures 1-3).
Full table
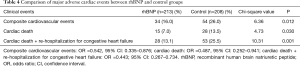
Comparison of major adverse cardiac events between the rhBNP and control groups
At postoperative 6 months, the incidences of composite cardiovascular events (16.0% vs. 26.0%, P=0.012), cardiac death (7.0% vs. 13.5%, P=0.030), and cardiac death + re-hospitalization for congestive heart failure (13.1% vs. 25.5%, P=0.001) were significantly lower in the rhBNP group than in the control group (Table 4). Furthermore, clinical endpoint events were also markedly reduced.
Full table
Discussion
Over the last 20 years, great progress has been made in the treatment of AMI. Diagnostic and treatment techniques have evolved from the establishment of the coronary care unit (CCU) mode to intravenous thrombolysis and direct PCI. This contributed to the decreased AMI mortality rate of 30% in the 1970s to approximately 5% (0.7–8.8%) at present (16). However, despite the constant improvement in myocardial salvage in patients with AMI and the gradual application of intravenous thrombolysis and direct PCI techniques, the mortality rate of AMI inpatients and major complications have not been reduced further in the last 10 years; and the mortality rate increased to 5–15% (2). Therefore, the treatment of AMI appears to have reached a plateau. In order to further decrease the mortality rate of AMI, existing advanced techniques should be continuously used, existing treatment strategies should be optimized, and novel treatment techniques, methods, strategies, as well as new drugs and instruments, should be developed.
BNP is a circulating hormone synthesized and secreted by the heart, and is present in atrial and ventricular muscle cells and vascular endothelial cells. BNP exerts action on guanylate cyclase-coupled natriuretic peptide receptor A on effector cell membranes. Activated guanylate cyclase converts guanosine triphosphate into cyclic guanosine monophosphate (cGMP). cGMP, as a second messenger, reactivates downstream enzyme signaling pathway-cGMP-dependent protein kinase 1, exerting a variety of effects (17). Under pathological conditions, the renin-angiotensin-aldosterone system is excessively activated, and the compensatory secretion of BNP is increased. BNP is a natural neuroendocrine antagonist that prevents the effects of rennin, aldosterone, norepinephrine and endothelin; and inhibits the excessive activation of the neuroendocrine system. BNP is also a natural factor against cardiac remodeling that regulates the levels of cytokines and inflammatory factors through regulating the expression of fibrosis genes. Furthermore, it directly exerts effects on cardiac fibroblasts to reduce the extracellular matrix of myocardial cells and alleviate interstitial fibrosis and myocardial hypertrophy (18-21). In addition, BNP selectively expands coronary and lung circulation, increases coronary blood flow and reduces the consumption of myocardial oxygen (22).
Chen et al. (22) treated 24 patients with acute anterior MI with low doses of rhBNP (0.006 µg/kg per minute) within 24 hours after successful PCI for 72 successive days. They revealed that rhBNP at 0.006 µg/kg per minute did induce adverse events, but significantly enhanced the plasma levels of cGMP and inhibited the activity of plasma aldosterone. Compared with baseline data, LVEF values were significantly increased, and the left ventricular end-systolic volume index was significantly decreased at postoperative 1 month.
Kitakaze et al. (10) investigated the effects of rhBNP on myocardial infarct size, left ventricular function and the clinical prognosis in patients with AMI after PCI. They included 569 patients with AMI, which were randomly divided to receive rhBNP (n=277, rhBNP 0.025 µg/kg per minute for three successive days) or placebo (n=292, glucose in water). In rhBNP- and placebo-treated patients, the left anterior descending artery was infarcted in 55.3% and 52.3% of cases; and Killip I cardiac function was present in 88.6% and 90.3% of cases, respectively. These results revealed that MI size in the rhBNP group decreased by 14.7% (P=0.016) compared with placebo. At postoperative 6–12 months (mean: 200 days), LVEF in the rhBNP group increased by 5.1% compared with placebo (44.7% vs. 42.5%, P=0.024). At postoperative 1.5–3.6 years (mean: 2.7 years), there were no significant differences in survival rate [hazard ratio (HR): 0.693; 95% confidence interval (CI): 0.269–1.788; P=0.446] or in the incidence of major adverse cardiac events (HR: 0.833; 95% CI: 0.608–1.140; P=0.252) between the rhBNP and control groups. However, the incidence of cardiac death + re-hospitalization for congestive heart failure in the rhBNP group was reduced by 73.3% compared with placebo (HR: 0.267; 95% CI: 0.089–0.799; P=0.011).
In our study, 421 patients with acute or extensive AMI were treated with or without rhBNP at the standard dose (maintenance dose recommended for acute heart failure) for 72 successive hours based on PCI and routine medication, and we investigated the effects of rhBNP use on cardiac enzyme data, left ventricular function and the incidence of major adverse cardiac events that would occur during postoperative 6 months, as well as patient tolerance to rhBNP. Our results revealed that rhBNP significantly decreased the serum concentrations of cTnT (at postoperative days one and seven) and NT-proBNP (at postoperative day seven), increased LVEF (at postoperative day seven and 6 months) and SV (at postoperative 6 months), and reduced LVEDd (at postoperative 6 months), compared to the control group. rhBNP use significantly decreased the incidence of composite cardiovascular events, cardiac death, and cardiac death + re-hospitalization for congestive heart failure. The incidence of composite cardiovascular events decreased from 26.0% (control group) to 16.0% (P=0.012), the incidence of cardiac death decreased from 13.5% (control group) to 7.0% (P=0.030), and the incidence of cardiac death + re-hospitalization for congestive heart failure decreased from 25.5% (control group) to 13.1% (P=0.001). The decreased incidence of cardiac death + re-hospitalization for congestive heart failure was the most significant.
The prognosis of patients with MI is closely related to the site of MI (23). Generally speaking, AMI located at the anterior wall has a larger infarction area, and yields a higher incidence of complicated left ventricular insufficiency; leading to higher acute or long-term mortality rate than other infarction sites. Intravenous thrombolysis or PCI shows better therapeutic effects on acute anterior MI. Since previous studies reported that rhBNP can improve negative left ventricular remodeling and protect left ventricular function (17-22), we presumed that rhBNP use has better therapeutic effects on acute anterior MI than in other infarction sites. Therefore, we investigated whether rhBNP has beneficial effects on this site, and determined its therapeutic intensity. Previous studies (23,24) have selected patients with acute anterior MI, who received pPCI treatment as subjects. Although trial design, patient selection and exclusion criteria, occasional rhBNP use and dose, and control drugs differed among these studies, all these results revealed that rhBNP significantly improved left ventricular remodeling and systolic function within postoperative 1 month. In studies conducted by Kitakaze et al. (10) and Hillock et al. (25), the infarction sites of patients were not limited. The study conducted by Kitakaze et al. (10) was a randomized single-blind trial, in which a large sample size (trial group, n=277 patients; and control group, n=292 patients) was used. Glucose in water was selected as the control drug and a large dose of rhBNP was used (0.025 µg/kg per minute is significantly greater than the 0.01 µg/kg per minute recommended for heart failure). Although Kitakaze et al. (10) reported obvious effects in reducing MI size, increasing LVEF, alleviating reperfusion injury, and decreasing the incidence of cardiac death + re-hospitalization for congestive heart failure, they did not observe any differences in patient survival rate and in the incidence of total major adverse cardiac events between the trial and control groups during the follow-up period [mean postoperative duration: 2.7 years (range, 1.5–3.6 years)]. Better trial outcomes might be obtained in patients with acute anterior MI. Hillock et al. (25) reported that during the 30–90-day follow-up period, improvements in left ventricular end-systolic volume and LVEF in the rhBNP group were more obvious than in the physiological saline control group. However, major adverse cardiac events were not observed, and the follow-up period was relatively short. In the present study, we only included patients with acute anterior or extensive MI. Our results revealed that at postoperative day seven, LVEF in the rhBNP group was greater than in the control group. At postoperative month 6, LVEF in the rhBNP group improved, and SV and LVEDd in the rhBNP group were better than in the control group. Furthermore, at postoperative 6 months, the incidences of composite cardiovascular disease, cardiac death, and cardiac death + re-hospitalization for congestive heart failure were significantly lower in the rhBNP group than in the control group, and the total therapeutic effects were better than that reported by Kitakaze et al. (10). These findings suggest that rhBNP shows better therapeutic effects in patients with simple acute anterior or extensive MI. Recently, Li et al. (26) investigated 93 patients with acute anterior wall MI undergoing primary PCI, who randomly accepted rhBNP treatment. They made a conclusion that administration of rhBNP before PCI with post-conditioning procedure can further improve myocardial perfusion, limit myocardial infarct size, ameliorate cardiac dysfunction, and postpone left ventricular early-stage and long-term remodeling in STEMI patients undergoing primary PCI.
BNP inhibits the activation of the renin-angiotensin-aldosterone system, selectively expands coronary arteries, and reduces MI size. These indicate that BNP is suitable for managing the pathological changes of early MI. Theoretically, after the onset of AMI, rhBNP should be used as early as possible, regardless of whether patients are undergoing emergent interventional therapy. In most clinical trials, rhBNP was used after PCI [rhBNP use was at approximately 5−6 hours after AMI onset in the study conducted by Kitakaze et al. (10)]. However, in the study conducted by Kasama et al. (24), rhBNP use was initiated prior to PCI (within 6 hours after AMI onset). Although the protocol rhBNP was scheduled to be administered as early as possible after patient admission and no later than 2 hours after the end time of the PCI procedure, most patients in the trial did not arrive at the hospital in a timely manner after the onset of chest pain. This resulted in the meantime interval between initial rhBNP use and the onset of AMI being delayed up to 6.7 hours (3.8–13.6 hours). Therefore, we failed to realize the original intention of the early application of rhBNP. If we could use rhBNP earlier, a better outcome might have been expected.
In the study conducted by Kitakaze et al. (10), more patients withdrew from the rhBNP group (29/255, 11.37%) due to low blood pressure, compared with the control group (1/280, 0.36%). There were two possible reasons: a large dose of rhBNP (0.025 µg/kg per minute) was used and the use of ACEI, and ARB and oral nitrates was not limited in the initial stage of treatment. Furthermore, 44.7% of patients included in the present study had vascular infarction at the left circumflex branch (6.4%) or right coronary artery (38.3%), with MI sites at the posterior wall or the right ventricle. These patients were generally sensitive to vasodilators. Thus, they were not likely to be tolerant to rhBNP. A study conducted by Hayashi et al. (27) reported data from patients with first time acute anterior MI, who received rhBNP or nitroglycerin at the same dose of 0.025 µg/kg per minute after receiving PCI and with a stable blood pressure determined by two measurements in the care unit, with no ACEI or oral nitrate use during the rhBNP use period. Their results revealed that rhBNP at 0.025 µg/kg per minute on blood pressure had similar effects to the equivalent dose of nitroglycerin. In the study conducted by Hillock et al. (25), although rhBNP was used at a routine dose (0.01 µg/kg per minute, lasted for 60 successive hours on average), ACEIs were not limited in the initial stage of the trial. Therefore, in the initial 8–12 hours of rhBNP use, mean blood pressure was significantly lower in the rhBNP group than in the control group (69.1±1.9 vs. 85.2±3.8 mmHg, P=0.001); and two patients with symptomatic hypotension (2/14, 14.3%) were reported in the rhBNP group. Chen et al. (22) used low dose rhBNP (0.006 µg/kg per minute) and added a low dose of ACEI during the 12–24 hours of rhBNP use. However, these two patients (2/12, 16.7%) withdrew from rhBNP due to symptomatic hypotension. Their results revealed that the incidence of symptomatic hypotension was not elevated in patients with acute anterior MI, compared with previously administered AMI patients. However, their sample size was small (n=12). Hence, their trial outcomes should be further validated.
In the present study, we used a routine dose of rhBNP (0.01 µg/kg per minute, lasted for 49 hours on average). However, ACEIs were not used during the initial 24 hours of rhBNP use; and the administration of ACEIs after 24 hours was determined by physicians. Our results revealed that 8.0% (n=17) of patients reduced their rhBNP dose due to unstable blood pressure and 4.2% (n=9) of patients withdrew from rhBNP due to hypotension in the rhBNP group; while 6.3% (n=13) of patients in the control group did not take or withdrew from intravenous nitrates due to unstable blood pressure. According to these findings and other present studies, symptomatic hypotension is an inevitable phenomenon during the treatment with rhBNP. This is probably related to the site of MI, the development of the disease itself, rhBNP dose and the effects of ACEI, and ARB and oral nitrates including β-receptor blockers. Therefore, rhBNP for the treatment of AMI should be used in patients exhibiting stable hemodynamics. In addition, appropriate rhBNP doses should be ensured, blood pressure should be closely monitored during rhBNP use, and the use of ancillary drugs should be delayed or the dose should be reduced.
This study has some limitations. This study is an open-label trial. In the control group, the types and dose of intravenous nitrates were not unified, which may lead to slight influences on the patient baseline data, the measurement of experimental parameters, and the assessment of clinical events. In addition, differences in ultrasonic machine brands and patterns and individual manipulation may have influenced the measurement of echocardiographic data. Six-month follow-up results can help to determine the preliminary clinical effects of rhBNP. The long-term therapeutic effects of early rhBNP administration in patients with acute anterior or extensive MI need to be further followed up.
Conclusions
For patients with acute anterior or extensive MI, who are planned to undergo PCI within an effective time window, rhBNP at a routine dose should be initiated as early as possible to decrease the serum concentrations of cTnT, CK-MB and NT-proBNP, increase LVEF, and decrease the incidence of composite cardiovascular diseases, cardiac death, and cardiac death + re-hospitalization for congestive heart failure during the subsequent postoperative 6 months. All of which improve the prognosis of patients with AMI.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of The People’s Hospital of Liaoning Province (No. 2011-01-003) and written informed consent was obtained from all patients.
Supplementary
Affiliations and principal investigator (arranged according to the number of included patients):
Department of Cardiology, The People’s Hospital of China Medical University (The People’s Hospital of Liaoning Province), Shenyang 110016, Liaoning Province, China (Zhi-Lin Miao, Ai-Jie Hou, Long Yuan, Ru-Ming Guan, Yun-Qi Shi, Li Liu, Li-Jie Cui, Na Duan, Fei Xia, Zhan-Quan Li);
Department of Cardiology, the 463rd Hospital of PLA, Shenyang 110042, China (Hong-Yun Zang);
Department of Cardiology, Tieling Central Hospital, Tieling 112000, China (Ru-Gang Huang);
Department of Cardiology, Dalian Municipal Central Hospital, Dalian 116013, China (Xiao-Qun Zheng, Hai-long Lin);
Department of Cardiology, Dandong Central Hospital, Dandong 118002, China (Wei Wang);
Department of Cardiology, Affiliated Hospital of Liaoning University of Traditional Chinese Medicine, Shenyang 110033, China (Ping Hou);
Department of Cardiology, the Third Affiliated Hospital of Liaoning Medical University, Jinzhou 121001, China (Zhi Zhang);
Department of Cardiology, the Fourth Affiliated Hospital of China Medical University, Shenyang 110032, China (Yuan-Zhe Jin);
Department of Cardiology, Tie Mei Coal Group General Hospital, Diaobingshan 112700, China (Ye Ma);
Department of Cardiology, Liaoyang Central Hospital, Liaoyang 111000, China (Li-Jun Zhao, Jie Li);
Department of Cardiology, Liaoning Provincial Jinqiu Hospital, Shenyang 110016, China (Ming Zhang);
Department of Cardiology, the 313th Hospital of PLA, Huludao 125000, China (Zhan-Xiu Zhang);
Department of Cardiology, Fushun Central Hospital, Fushun 113123, China (Li-li Zhang);
Department of Cardiology, Liaoyang Petrochemical General Hospital, Liaoyang 111003, China (Guang-Kai Cui);
Department of Cardiology, Affiliated Zhongshan Hospital of Dalian Medical University, Dalian 116013, China (Lian-Na Xie);
Department of Cardiology, First Affiliated Hospital of Liaoning Medical University, Jinzhou 121001, China (Gui-Zhou Tao);
Department of Cardiology, Second Affiliated Hospital of Liaoning Medical University, Shenyang 110002, China (Jing-Ru Ma);
Department of Cardiology, Yingkou Development Zone Central Hospital, Yingkou 115007, China (Qing-Tao Yu);
Department of Cardiology, Shenyang Weikang Hospital, Shenyang 110021, China (Xu-Jie Fu);
Department of Cardiology, Second People’s Hospital of Liaoyang City, Liaoyang 111000, China (Yi-Nan Li).
References
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361:13-20. [Crossref]
- Li J, Li X, Wang Q, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet 2015;385:441-51. [Crossref]
- McCullough PA. Clinical applications of B-type natriuretic peptide levels in the care of cardiovascular patients. Minerva Cardioangiol 2004;52:479-89.
- Cowie MR, Mendez GF. BNP and congestive heart failure. Prog Cardiovasc Dis 2002;44:293-321. [Crossref]
- Connell JM, Davies E. The new biology of aldosterone. J Endocrinol 2005;186:1-20. [Crossref]
- Fazlinezhad A, Rezaeian MK, Yousefzadeh H, et al. Plasma Brain Natriuretic Peptide (BNP) as an Indicator of Left Ventricular Function, Early Outcome and Mechanical Complications after Acute Myocardial Infarction. Clin Med Insights Cardiol 2011;5:77-83.
- Mayr A, Mair J, Schocke M, et al. Predictive value of NT-pro BNP after acute myocardial infarction: relation with acute and chronic infarct size and myocardial function. Int J Cardiol 2011;147:118-23. [Crossref]
- Fonarow GC. Nesiritide: practical guide to its safe and effective use. Rev Cardiovasc Med 2001;2 Suppl 2:S32-5.
- Kuga H, Ogawa K, Oida A, et al. Administration of atrial natriuretic peptide attenuates reperfusion phenomena and preserves left ventricular regional wall motion after direct coronary angioplasty for acute myocardial infarction. Circ J 2003;67:443-8. [Crossref]
- Kitakaze M, Asakura M, Kim J, et al. Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (J-WIND): two randomised trials. Lancet 2007;370:1483-93. [Crossref]
- Lyu T, Zhao Y, Zhang T, et al. Natriuretic peptides as an adjunctive treatment for acute myocardial infarction: insights from the meta-analysis of 1,389 patients from 20 trials. Int Heart J 2014;55:8-16. [Crossref]
- Zhang J, Fu X, Jia X, et al. B-type natriuretic peptide for prevention of contrast-induced nephropathy in patients with heart failure undergoing primary percutaneous coronary intervention. Acta Radiol 2010;51:641-8. [Crossref]
- China Society of Cardiology of Chinese Medical Association; Editorial Board of Chinese Journal of Cardiology. Guideline for diagnosis and treatment of patients with ST-elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi 2010;38:675-90.
- Section of Interventional Cardiology, Chinese Society of Cardiology of Chinese Medical Association. Editorial Board of Chinese Journal of Cardiology. Chinese guideline for percutaneous coronary intervention(pocket guideline). Zhonghua Xin Xue Guan Bing Za Zhi 2012;40:271-7.
- Dégano IR, Salomaa V, Veronesi G, et al. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart 2015;101:1413-21. [Crossref]
- Burnett JC Jr. Vasopeptidase inhibition: a new concept in blood pressure management. J Hypertens Suppl 1999;17:S37-43.
- Burger AJ. A review of the renal and neurohormonal effects of B-type natriuretic peptide. Congest Heart Fail 2005;11:30-8. [Crossref]
- Tamura N, Ogawa Y, Chusho H, et al. Cardiac fibrosis in mice lacking brain natriuretic peptide. Proc Natl Acad Sci U S A 2000;97:4239-44. [Crossref]
- Oliver PM, Fox JE, Kim R, et al. Hypertension, cardiac hypertrophy, and sudden death in mice lacking natriuretic peptide receptor A. Proc Natl Acad Sci U S A 1997;94:14730-5. [Crossref]
- Manolescu DC, Jankowski M, Danalache BA, et al. All-trans retinoic acid stimulates gene expression of the cardioprotective natriuretic peptide system and prevents fibrosis and apoptosis in cardiomyocytes of obese ob/ob mice. Appl Physiol Nutr Metab 2014;39:1127-36. [Crossref]
- Michaels AD, Klein A, Madden JA, et al. Effects of intravenous nesiritide on human coronary vasomotor regulation and myocardial oxygen uptake. Circulation 2003;107:2697-701. [Crossref]
- Chen HH, Martin FL, Gibbons RJ, et al. Low-dose nesiritide in human anterior myocardial infarction suppresses aldosterone and preserves ventricular function and structure: a proof of concept study. Heart 2009;95:1315-9. [Crossref]
- Nienhuis MB, Ottervanger JP, Dambrink JH, et al. Comparative predictive value of infarct location, peak CK, and ejection fraction after primary PCI for ST elevation myocardial infarction. Coron Artery Dis 2009;20:9-14. [Crossref]
- Kasama S, Toyama T, Hatori T, et al. Effects of intravenous atrial natriuretic peptide on cardiac sympathetic nerve activity and left ventricular remodeling in patients with first anterior acute myocardial infarction. J Am Coll Cardiol 2007;49:667-74. [Crossref]
- Hillock RJ, Frampton CM, Yandle TG, et al. B-type natriuretic peptide infusions in acute myocardial infarction. Heart 2008;94:617-22. [Crossref]
- Li S, Fu X, Dai Y, et al. Effects of pretreatment with recombinant human B-type natriuretic peptide on infarct size in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Zhonghua Xin Xue Guan Bing Za Zhi 2015;43:954-9.
- Hayashi M, Tsutamoto T, Wada A, et al. Intravenous atrial natriuretic peptide prevents left ventricular remodeling in patients with first anterior acute myocardial infarction. J Am Coll Cardiol 2001;37:1820-6. [Crossref]


