Clinical analysis of eight patients with blunt main stem bronchial injuries
Introduction
Blunt main stem bronchial injuries are rare but potentially life-threatening injuries which can caused by a great diversity of direct or indirect traumas. Karmy-Jones investigated 1,178 patients dying due to blunt trauma and only 33 (2.8%) developed a blunt main stem bronchial injury (1). Most of the patients die at the site of injury due to asphyxia, which associated with a high mortality of 30% and early intervention is the key to survival (2). Trauma history is the premise for correct diagnosis of blunt main stem bronchial injuries and special clinical sign, such as pneumoderma in the neck and chest, pneumomediastinum, pneumothorax can give invaluable clues to the diagnosis. Conventional radiology tests such as X-ray and computed tomography (CT) are useful of primary diagnostic tools in initial trauma examination (3). Bronchoscopy is crucial to the precise diagnosis of blunt main stem bronchial injuries in a patient with suspected airway injury, which can show the detail of injury, such as size, site and extent (4). The first and most important priority in blunt main stem bronchial injuries is to ensure adequate airway, and surgical approach is the preferred method for ventilation reestablishment.
Methods
This report retrospective1y analyzed eight cases of main stem bronchial injuries induced by blunt chest trauma between 2013 and 2016 in Tangdu Hospital, Fourth Military Medical University.
Results
Characteristics of the study group
In the analyzed group, eight patients were diagnosed with blunt main stem bronchial injuries and treated by surgery. There were four women patients (50%) and four men patients (50%) with the mean age of 28.4 years (ranging from 14 to 43 years). In four patients there was an injury to the left main stem bronchus, in three patients to the right main stem bronchus and in one patient to the ambilateral main stem bronchus (Table 1).

Full table
Diagnose of the injuries
All patients were admitted to our hospital from peripheral hospital with history of blunt chest trauma. One patient was intubated with single lumen endotracheal tube. Mean time between injury and treatment in our hospital was 4.25 days (range, 1–12 days).
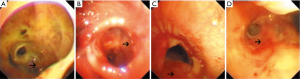
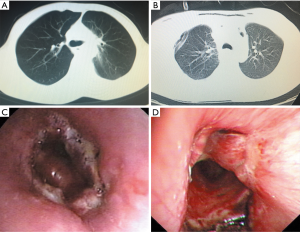
The most frequent sign was chest pain, followed by pneumoderm in the neck and chest, respiratory distress, dyspnea and haemoptysis. In all cases chest X-ray and CT were gained on emergency ward to check for subcutaneous emphysema, pneumothorax, pneumomediastinum and pulmonary atelectasis, as well as to obtain more details on anatomy (Figure 1). Moreover, fiber-optic bronchoscopy was done with investigation of the size, site and extent of lesion on emergency ward or on operating room (Figure 2). Mean size of airway injury was 1.04 cm (range, 0.5–2 cm). Oesophagoscopy was also applied to exclude esophageal rupture, esophagotracheal fistula, and so on.

Treatment of the injuries
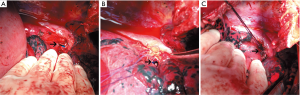
Emergent operation was performed in two patients and elective operation in six patients. The principle of surgical treatment is that interrupted primary repair with PDS 4-0 was adopted in cases with simple clean main stem bronchial injuries and debridement of devitalized tissue including granulation tissue and cartilage, end to end anastomosis with absorbable sutures was performed in cases with serious tainted damage (Figure 3). In our group, the primary repair was performed via right thoracotomy in two patients and via left thoracotomy in one patient, and the end to end bronchial anastomosis was performed via right thoracotomy in two patients and via left thoracotomy in the remaining three patients. In one case the anastomotic stoma was additionally covered with a pericardium. There was no air leakage through the anastomosis site at positive pressure of 30 cmH2O. Closed drainage of pleural cavity and posterior mediastinum drainage were routinely performed. After operation, all the patients were transferred to the intensive care unit (ICU), and fibrobronchoscopy was performed routinely so as to clear bronchial secretions and check integrity of anastomotic stoma. Additional, intravenous antibiotics and aerosol inhalation mucolytic agent were administered. The average hospitalization time was 20.63 days (range, 12–37 days).
There was no death in this group. Arterial blood gases after bronchial repair showed markedly improved. One patient with left main stem bronchi injury developed anastomotic stricture 1 month after surgery, and was healed by granulation tissue resection and cryotherapy under fibrobronchoscopy. No main stem bronchus injury-related complications were noted in the remaining seven patients and they were able to take part in normal activities (Figure 4). The follow-up fibrobronchoscopy was performed at 3 months after surgery which confirmed complete healing and good patency of the airway in all patients.
Discussion
Main stem bronchial injury occurring after blunt trauma is a rare scenario that requires skillful handling of airway (5). The reported incidence in literature is less than 2.8% (1,6). While it is a highly lethal cause of asphyxia at the moment of injury, and universally fatal in misdiagnosed patients or in incorrect managed cases with a high rate of mortality. Here, we report a series of eight cases of blunt main stem bronchial injury with good results.
Blunt main stem bronchial injuries can caused by a great diversity of direct or indirect traumas. However, the exact mechanisms of blunt main stem bronchial injuries have not heretofore been elucidated. Three theories have been reported account for the mechanism of blunt main stem bronchial injuries (7). One is the shearing force increased at the cricoids cartilage and carina. Second one involves the development of tensile force due to anteroposterior compression of the chest. The third one theory relates to the reflex closure of glottis while intrathoracic pressure rising suddenly. This leads to a rapid increase in airway pressure, especially in the ambilateral main stem bronchus. As the left main stem bronchus is fixed and protected by adjacent major vessels, while the right main stem bronchus lack of supporting structures and heavier right lung on the shorter right bronchus, more right main stem bronchus injuries been found. Nevertheless, in our patients only 3 out of 8 patients (37.5%) suffered from right main stem bronchus injuries, while 4 out of 8 patients (50%) suffered from left main stem bronchus injuries. Most of our patients (50%) suffered from left chest trauma may account for the difference.
Make a diagnosis of blunt main stem injuries immediately is difficult. It was reported that blunt main stem bronchus injuries are not diagnosed immediately in 25% to 68% of the cases (8). The clinical manifestations are non-specific and can vary from chest pain, cough, respiratory distress, dyspnea, haemoptysis to mediastinal emphysema, subcutaneous emphysema or pneumothorax (9). Almost all of the patients suffered from chest pain. Furthermore, subcutaneous emphysema, respiratory distress and dyspnea are frequent clinical features occurring in 77–85% of the patients (10). A massive air leak and the inability to re-expand the lung after tube thoracotomy are highly indicative of a main stem bronchus injury which was also seen in 4 of our patients (11). Additional, in our patients, eight cases complained of chest pain, six cases complained of respiratory distress, four cases with subcutaneous emphysema in the neck and chest, 1cases with haemoptysis.
Routine radiological tests such as X-ray and CT are extremely important in the early diagnosis of main stem bronchial injuries. Moreover, thorax CT maintains its effectiveness in inspecting trauma and it is availability in detecting the appearance of possible great vessel injuries, hemopericardium or mediastinal hematoma (12). It may show pneumoderm, pneumomediastinum, pneumothorax, pulmonary atelectasis, respiratory tree deviation or specific site of the separation. Complete disconnection of the main stem bronchi may make for the typical findings of atelectasis, “absent hilum” or collapsing of the lung away from the hilum towards to diaphragm is the classic imaging manifestations features of main stem bronchus injuries and known as “falling lung sign of Kumpe” (13). Pneumothorax, especially intractable pneumothorax with prolonged air leakage, should increase the suspicion of main stem bronchial injuries. Fibrobronchoscopy provides the resultful precise diagnostic study in a patient with suspected main stem bronchus injuries. The advantages of fibrobronchoscopy are that it can be performed quickly and easily even in the accompanying multi-organ injuries. Additional, it can be applied securely in the operating room with general anesthesia before operation. Check and examine the tracheobronchial tree carefully with fiber-optic bronchoscopy reveals the detail of injury, such as size, site and extent. Moreover, it is important that if fibrobronchoscopy is to be performed in an intubated patient, the endotracheal tube should be withdrawn carefully in order not to miss out small injury and proximal airway injury. In our patients, the thorax CT was performed in the emergency ward that provides useful clues for suspected main stem bronchial injuries. The definitive diagnosis of main stem injuries was confirmed by fibrobronchoscopy in endoscope room or in operating room, which provides the site, size, and extent of injury accurately.
Surgical treatment of the injuries of main stem bronchus can be extremely challenging. In patients, who cannot be managed conservatively, the most optimal therapeutic strategy is the surgical treatment as early as possible. Even in some minor injuries patients, granulation and structure may develop around the injuries; surgery also is the preferred method. The mortality for those who underwent primary repair was lower than those who underwent resection of the injured bronchus and distal lung parenchyma (3% vs. 13%) (8). In our patients, all the eight cases adopted the surgical therapy, and no one died during the perioperative period. Among them, emergent operation was performed in two patients and elective operation in the remaining six patients.
The right main stem bronchus, right atrium, superior vena cava, azygos vein and most of intrathoracic esophagus can be easily displayed by a right thoracotomy, while the left mainstem bronchi, descending thoracic aorta, distal part of aortic arch and proximal left subclavian artery can be easily exposure by a left thoracotomy. In our patients, four patients with left main stem bronchi injuries underwent left posterolateral thoracotomy through the fifth intercostal space, while the remaining four patients underwent right posterolateral thoracotomy, also through the fifth intercostal space. The principle of surgical treatment is that interrupted primary repair with PDS 4-0 was adopted in cases with simple clean main stem bronchial injuries and debridement of devitalized tissue including granulation tissue and cartilage, end to end anastomosis with absorbable sutures was performed in cases with serious tainted damage. Moreover, in cases with serious ambilateral main stem bronchial damage, all devitalized tissue should be debrided with the attention of preserving as much viable airway as possible (14). In our patients, end to end bronchial anastomosis was performed in five patients and primary repair in the remaining three patients. Primary repair was performed in three patients for their fresh and clean lesions. Meanwhile, for the late diagnosis patients, the optimal surgical treatment strategy is bronchial resection with reconstruction except the patients with unreconstructable lesions or destructed distal lung. It is noteworthy that appropriate seam of absorbable interrupted sutures assures airtight anastomosis and eliminates the discrepancy between the distal and proximal bronchus. It also ensures minimal anastomotic granulations. In our patients, there was no death under perioperative. Two emergency surgeries were necessary owing to worsening oxygen saturation, pneumothorax, and hemodynamics. It is encouraging that no pneumonectomy was performed in our group, even in the patient with ambilateral main stem bronchial injuries.
Blunt main stem bronchial injuries are rare but potentially life-threatening injuries. Early diagnosis and early surgical treatment are crucial to reducing death rate. Fibrobronchoscopy is the optimized diagnostic tool and surgical approach is the preferred method for patients with these life-threatening complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee of Tangdu Hospital (No. 201647).
References
- Karmy-Jones R, Wood DE. Traumatic injury to the trachea and bronchus. Thorac Surg Clin 2007;17:35-46. [Crossref]
- Nishiumi N, Inokuchi S, Oiwa K, et al. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg 2010;89:232-8. [Crossref]
- Chen JD, Shanmuganathan K, Mirvis SE, et al. Using CT to diagnose tracheal rupture. AJR Am J Roentgenol 2001;176:1273-80. [Crossref]
- Gil T, Warmus J, Włodarczyk J, Grochowski Z, et al. Iatrogenic injuries to the trachea and main bronchi. Kardiochir Torakochirurgia Pol 2016;13:113-6. [Crossref]
- Pandey V, Meena DS, Choraria S, et al. Tracheobronchial Injury caused by Blunt Trauma: Case Report and Review of Literature. J Clin Diagn Res 2016;10:UD01-3.
- Devitt JH, Boulanger BR. Lower airway injuries and anaesthesia. Can J Anaesth 1996;43:148-59. [Crossref]
- Kirsh MM, Orringer MB, Behrendt DM, et al. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann Thorac Surg 1976;22:93-101. [Crossref]
- Kiser AC, O'Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001;71:2059-65. [Crossref]
- Sengupta S, Saikia A, Ramasubban S, et al. Anaesthetic management of a patient with complete tracheal rupture following blunt chest trauma. Ann Card Anaesth 2008;11:123-6. [Crossref]
- Visvikis GA, Hinrichs CA, Shah K. Virtual endoscopy for evaluation of tracheal laceration. Emerg Radiol 2002;9:162-4. [Crossref]
- Gabor S, Renner H, Pinter H, et al. Indications for surgery in tracheobronchial ruptures. Eur J Cardiothorac Surg 2001;20:399-404. [Crossref]
- Altinok T, Can A. Management of tracheobronchial injuries. Eurasian J Med 2014;46:209-15. [Crossref]
- Wintermark M, Schnyder P, Wicky S. Blunt traumatic rupture of a mainstem bronchus: spiral CT demonstration of the "fallen lung" sign. Eur Radiol 2001;11:409-11. [Crossref]
- Mitchell JD, Mathisen DJ, Wright CD, et al. Clinical experience with carinal resection. J Thorac Cardiovasc Surg 1999;117:39-52; discussion 52-3. [Crossref]


