|
Original Article
Outcomes of a hybrid technique for video-assisted thoracoscopic surgery (VATS) pulmonary resection in a community setting
Roger H Kim1, Kazuaki Takabe2, Charles G Lockhart3
1Division of Surgical Oncology, Department of Surgery, Louisiana State University Health Sciences Center – Shreveport and Feist-Weiller Cancer Center, Shreveport, LA, USA; 2Division of Surgical Oncology, Department of Surgery, Virginia Commonwealth University School of Medicine and Massey Cancer Center, Richmond, VA, USA; 3Thoracic Surgery Institute, Bon Secours Health System, Richmond, VA, USA
Corresponding Author: Roger H. Kim, MD. 1501 Kings Hwy, P.O. Box 33932, Shreveport, LA 71130-3932, USA. Tel: 318-675-6123; Fax: 318-675-6171. E-mail: rkim@lsuhsc.edu.
|
|
Abstract
Background: Video-assisted thoracoscopic surgery (VATS) for pulmonary resection was first described 18 years ago; however, it has yet to gain widespread acceptance in community hospitals in the United States. The majority of surgeons who routinely perform VATS resections work in academic or government institutions. There is little data reporting outcomes of VATS pulmonary resections by community-based surgeons. This article reports the outcomes of a hybrid technique for VATS pulmonary resection in a single-surgeon, community-based practice.
Methods: A retrospective study was performed on all VATS pulmonary resections performed from January 2000 to March 2008 by a community-based, solo-practice surgeon using a hybrid VATS technique, which utilizes dual access through a thoracoscopy port and a utility incision.
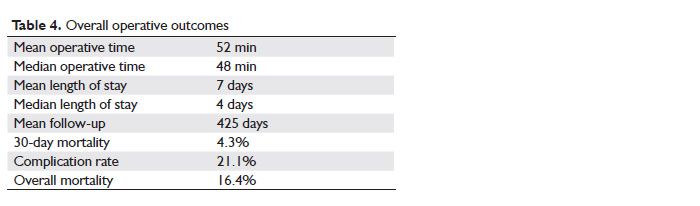
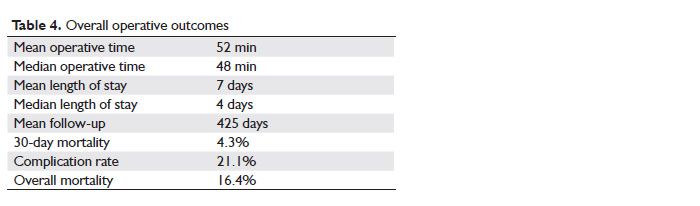
Results: A total of 1170 VATS pulmonary resections were performed over the study period, which is the largest single-surgeon series on VATS pulmonary resection to our knowledge. Among them, 746 cases were for malignant disease. Mean operative time was 52 minutes (median 48 minutes). Mean length of stay was 7 days (median 4 days). Mean length of ICU stay was 1.4 days, with 83% of patients having no days spent in the ICU. Mean length of chest tube duration was 4.5 days. The morbidity rate was 21.1 %, with neuropraxia as the most frequent complication. Perioperative mortality was 4.3% and overall mortality was 16.4%, with a mean follow-up of 425 days.
Conclusion: This series shows that our hybrid VATS approach to pulmonary resection is safe and feasible at community hospital-based practices.
Key words
VATS; video-assisted thoracoscopy; pulmonary resection; minimally invasive; community-based; lung cancer
J Thorac Dis 2010;2:210-214. DOI: 10.3978/j.issn.2072-1439.2010.11.5
|
|
Introduction
Video-assisted thoracoscopic surgery (VATS) for pulmonary resection was first described in 1992 ( 1), however, the technique has not yet gained widespread acceptance. Only 5% of the estimated 40,000 lobectomies performed each year in the United States are done via VATS ( 2), and a mere 2-3% of lobectomies in the United Kingdom are performed with this technique ( 3). The majority (78.8%) of surgeons who routinely perform VATS work primarily in academic or government institutions ( 4). Among the proposed factors contributing to the slow adoption of VATS among community-based surgeons are the perceived complexity of the technique, inadequate instrumentation and resources, and concern regarding the potential compromise of surgical and oncologic principles ( 5, 6). There is a relatively paucity of data reporting the outcome of VATS in the community setting. We previously described a hybrid technique that enables a single surgeon to routinely perform VATS pulmonary resection in a community-based practice ( 7). This present paper reports on the outcomes obtained with this technique over an 8-year period and is, to our knowledge, the largest single-surgeon series on VATS pulmonary resection.
|
|
Materials and methods
Patients
From January 2000 through March 2008, 1170 patients underwent VATS pulmonary resections utilizing a hybrid technique. All procedures were performed at a community hospital (Chippenham Medical Center, Richmond, Virginia) by a single surgeon (CGL). Institutional Review Board approval was obtained for this retrospective review.
Surgical technique
The hybrid technique for VATS pulmonary resection has been previously described ( 7). In brief, a 10-mm thoracoscopy port is placed in the eighth interspace and an ( 8-10) cm utility incision is created in the fifth interspace. A rib-spreader is gently applied to provide exposure. Rib resection is not performed. Both instrumentation and visualization can be performed through either the utility incision or the through the thoracoscopy port, allowing for maximal adaptability in tailoring the hybrid technique for each individual procedure. Furthermore, the utility incision permits immediate access to the operative field for urgent control of bleeding that would otherwise be difficult to control through a conventional thoracoscopic approach.
Outcomes
The following variables were collected analyzed: patient age and gender; diagnosis; histopathology; extent of pulmonary resection; operative time; length of hospital stay; length of intensive care unit (ICU) stay; duration of chest tube; postoperative complications; intraoperative and perioperative mortality; long-term mortality.
|
|
Results
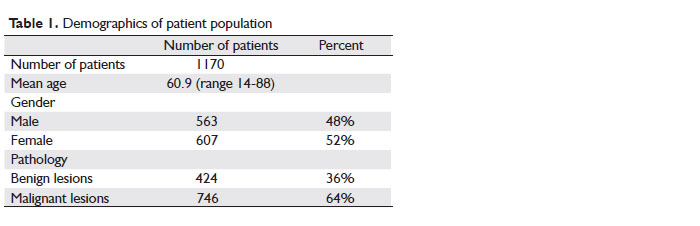
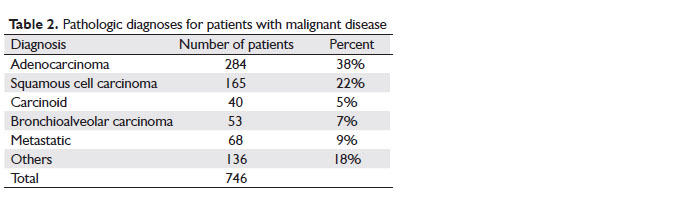
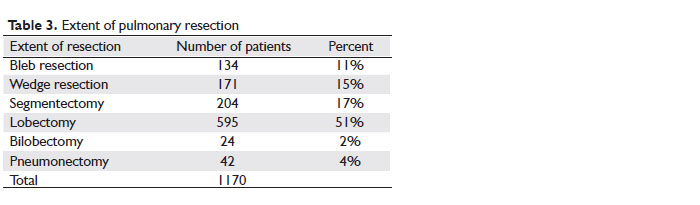
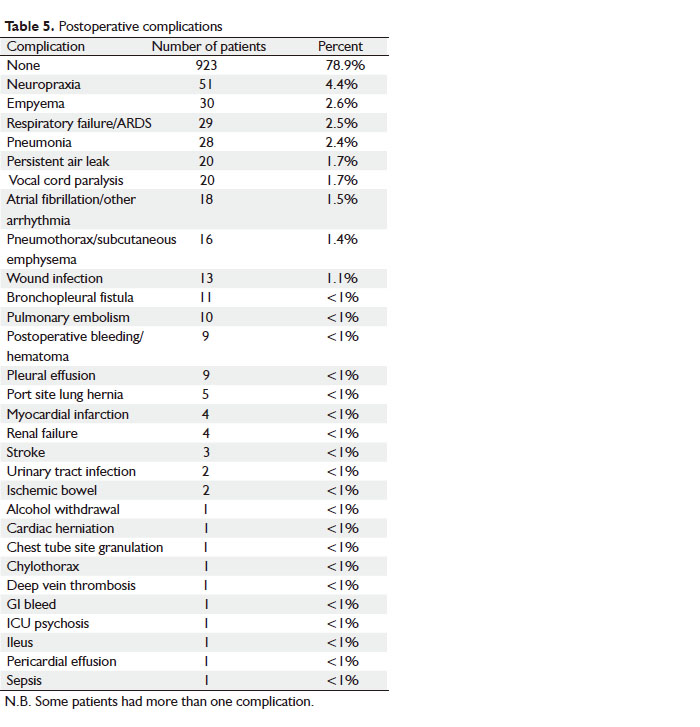
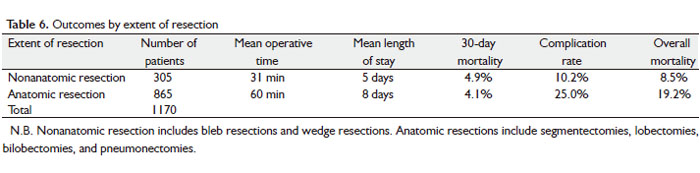
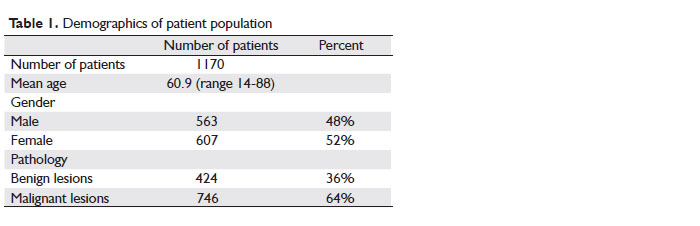
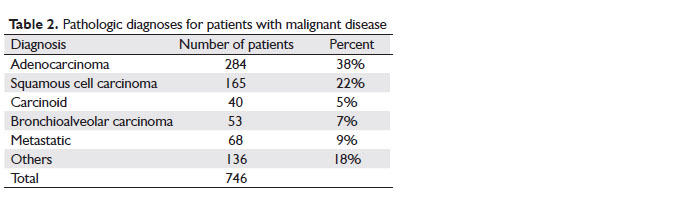
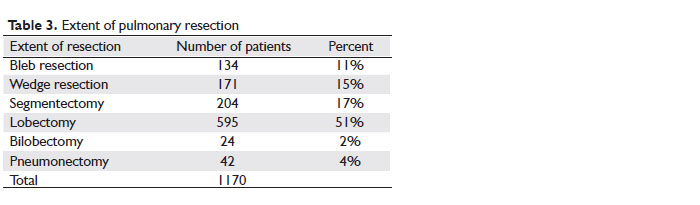
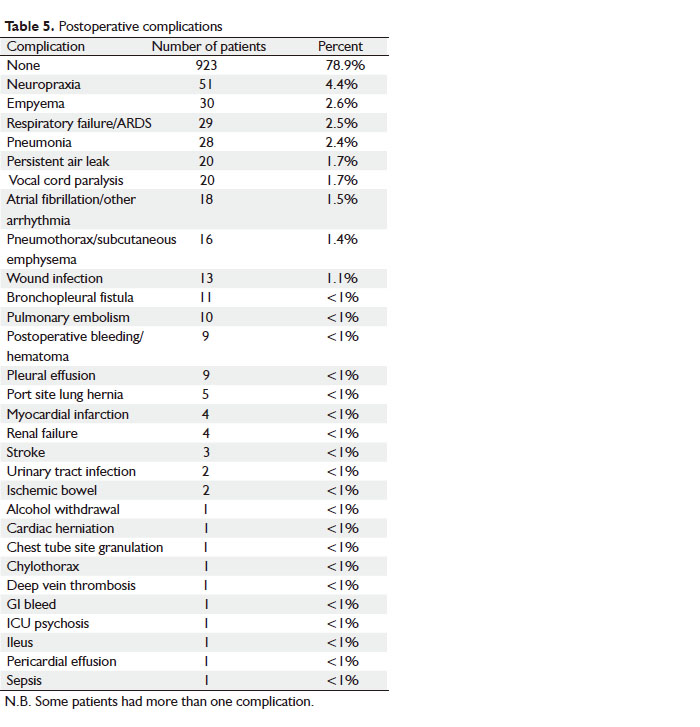
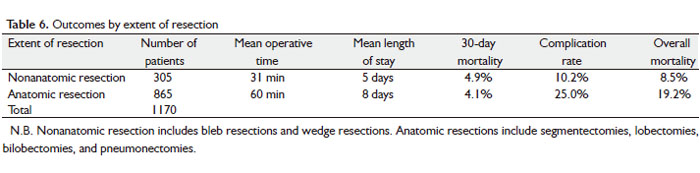
From January 2000 through March 2008, 1170 patients underwent VATS pulmonary resections at Chippenham Medical Center. All procedures were performed by a single surgeon (CGL), who first started utilizing this hybrid technique in 1994. The demographic information is summarized in Table 1. There were 607 women (52%) and 563 men (48%), with a mean age of 60.9 years (range, 14-88). 424 patients (36%) had benign lesions, and 746 (64%) had malignant lesions. The pathologic diagnoses for patients with malignant disease are summarized in Table 2. The types of resections performed are shown in Table 3. There were no conversions to conventional thoracotomy in any patients. Operative outcomes are summarized in Table 4. The mean operative time was 52 minutes with a median of 48 minutes. The mean length of hospital stay was 7 days, with a median of 4 days. Information on intensive care unit (ICU) stay was available for 416 patients (36%). Of these patients, the mean length of ICU stay was 1.4 days, with 345 patients having no days spent in the ICU (83%). Data on chest tube duration was available for 452 patients (38%). The mean length of time with a chest tube forthese patients was 4.5 days. The number of patients with postoperative complications was 247, with an overall complication rate of 21.1%. The majority of patients (78.9%) had no complications. The types of postoperative complications are summarized in Table 5. The most common complication was neuropraxia. When neuropraxia is excluded as a complication, the overall complication rate was 17.4%. Table 6 summarizes the operative outcomes by extent of resection. Nonanatomic resection was defined as bleb resections and wedge resections, while anatomic resection was defined as segmentectomies, lobectomies, bilobectomies, and pneumonectomies.
There were no intraoperative deaths, however, 50 patients (4.3%) died in the perioperative period (within 30 days of surgery). Overall mortality was 192 patients (16.4%), during a mean follow-up of 425 days.
|
|
Discussion
The body of evidence supporting the VATS approach to pulmonary resection continues to increase. In a randomized study of 61 patients undergoing VATS lobectomy versus open lobectomy for Stage I non-small cell lung cancer, Kirby and colleagues reported a significantly lower incidence of postoperative complications in the VATS group (6% versus 16%) ( 8). In another randomized trial conducted in Japan, there was no statistical difference in 5-year survival (90% versus 85% at 5 years) or recurrence rates for patients undergoing VATS or open lobectomy, leading to the conclusion that the VATS approach is not oncologically inferior to the open approach ( 9). Demmy reported a shorter length of stay and faster return to activity in VATS lobectomy group compared to matched controls who underwent open lobectomy, despite higher risk patients in the VATS group ( 10). In their review of the current literature, Alam and Flores concluded that VATS lobectomy can be performed safely with mortality and complication rates equivalent to open lobectomy, with less postoperative pain and with equal to or shorter length of stay ( 5). In their series of 349 VATS lobectomies, Loscertales and colleagues achieved low morbidity (12.89%), perioperative mortality (1.43%), and 5-year survival of 80.1%, and concluded that long term survival from lung cancer should not be affected by surgical approach and asserted that VATS lobectomy should be the treatment of choice for early stage non-small cell lung cancer ( 11). In spite of this growing body of evidence, VATS pulmonary resection has yet to become widespread, especially in the community setting ( 12). Only one out of 20 pulmonary lobectomies performed in the United States is performed by VATS ( 2). Adoption of VATS has been even slower in the United Kingdom, where this technique is estimated to be performed at half the rate in the United States ( 3). VATS pulmonary resection is generally regarded as technically demanding and, for the most part (78.8%), has been performed only in high-volume academic centers ( 4). This is especially true for completely thoracoscopic VATS pulmonary resections, which has, to our knowledge, only been performed in high-volume academic practices ( 13). Our hybrid technique of VATS incorporates the routine use of a utility incision, which provides a combined visual and technical advantage in performing VATS pulmonary resection safely and efficiently. We have previously described in detail the technical advantages of this hybrid approach, which include dual visualization, double light source illumination of the operative field, flexibility in instrumentation, and the “safety-valve” nature of the utility incision in control of hemorrhage ( 7). These advantages have allowed the VATS approach to be utilized in a single surgeon, community-based practice, with the vast majority of procedures performed with only a single scrub nurse as an assistant, demonstrating that this technique can be adopted in settings where highly trained assistants, such as surgical residents or fellows, may not be readily available. In addition, this hybrid technique can be easily adapted to any extent of pulmonary resection, from nonanatomic bleb or wedge resections, to anatomic resections such as lobectomies or pneumonectomies. The ease of adoption and adaptability of this technique in the community setting has resulted in what is, to our knowledge, the largest single-surgeon series of VATS pulmonary resections. There have been multiple reports of exceptional survival after VATS lobectomy, with results equivalent to those of conventional thoracotomy ( 14, 15). Lewis reported a mean survival of 86% at 18.6 months ( 16). Others have reported survival rates of 94.4% at 4 years ( 17) and 90% at 5 years ( 9). One series reported hospital stays of 5.3 days and chest tube durations of 4.0 days ( 10), while McKenna reported a median length of stay of 3 days ( 2). In this series detailing the outcomes of our hybrid VATS approach, we report overall survival (83.6%), length of stay (median 4 days), and chest tube duration (mean 4.5 days) that compares favorably with these results from conventional VATS approaches. In addition, there were no conversions to thoracotomy in our series. Furthermore, these results were obtained in a series that includes patients that underwent VATS pneumonectomies. Similarly, multiple authors have demonstrated equivalent or lower complication rates after VATS lobectomy when compared to thoracotomy ( 18, 19). In a randomized trial conducted in Germany, there were fewer complications after the VATS approach (14.2%) when compared to thoracotomy (50%) ( 20). Reported morbidity after VATS pulmonary resections ranges from 7.7% to 29.9% ( 2, 21-25). The complication rate in this series was 21.1%, which compares favorably with reported results from conventional VATS approaches. In addition, we included neuropraxia as a complication in our results, which most other studies do not report as a complication ( 2, 26). When neuropraxia was excluded, the complication rate in this series was 17.4%. Because this was a retrospective series, data regarding postoperative pain was not available. Although there is the potential for increased pain due to routine use of a utility incision in our hybrid VATS approach, most techniques for VATS pulmonary resection requires some form of incision for specimen retrieval ( 2, 21). Rib resection, which has been shown to be a significant factor in post-thoracotomy pain ( 27), was not performed in our approach. In addition, the length of stay for our patients was comparable to that of conventional VATS approaches, a result that would have been less likely if our hybrid VATS approach was associated with increased pain. Furthermore, chest tubes were in place for a relatively short duration in our series, which has the potential to decrease postoperative pain. Postoperative pain has been shown to be decreased for VATS pulmonary resections, with less use of opiods and shorter hospital stays when compared to thoracotomy ( 27). This series demonstrates that our hybrid VATS approach to pulmonary resection is safe and feasible at community hospital-based practices and results in outcomes similar to that of conventional VATS pulmonary resections. Our hope is that this hybrid technique may allow an increase in adoption of these procedures in smaller, community-based practices. This, in turn, may increase the proportion of pulmonary resections done by VATS, resulting in a potentially greater number of patients benefiting from minimally invasive thoracic surgery.
|
|
Acknowledgement
This work was supported, in whole or in part, by Virginia Commonwealth University Grant BIRCWH K12HD055881, and Susan G Komen for the Cure Career Catalyst Research Grant KG090510 (to K. T.).
|
|
References
- Roviaro G, Rebuffat C, Varoli F, Vergani C, Mariani C, Maciocco M. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7.[LinkOut]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5.[LinkOut]
- Walker WS, Codispoti M, Soon SY, Stamenkovic S, Carnochan F, Pugh G. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402.[LinkOut]
- Yim AP, Landreneau RJ, Izzat MB, Fung AL, Wan S. Is video-assisted thoracoscopic lobectomy a unified approach? Ann Thorac Surg 1998;66:1155-8.[LinkOut]
- Alam N, Flores RM. Video-assisted thoracic surgery (VATS) lobectomy: the evidence base. JSLS 2007;11:368-74.[LinkOut]
- Mack MJ, Scruggs GR, Kelly KM, Shennib H, Landreneau RJ. Video-assisted thoracic surgery: has technology found its place? Ann Thorac Surg 1997;64:211-5.[LinkOut]
- Kim RH, Takabe K, Lockhart CG. A hybrid technique: video-assisted thoracoscopic surgery (VATS) pulmonary resections for community-based surgeons. Surg Endosc 2010;24:700-4.[LinkOut]
- Kirby TJ, Mack MJ, Landreneau RJ, Rice TW. Lobectomy--video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg 1995;109:997-1001.[LinkOut]
- Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000;24:27-30.[LinkOut]
- Demmy TL, Curtis JJ. Minimally invasive lobectomy directed toward frail and high-risk patients: a case-control study. Ann Thorac Surg 1999;68:194-200.[LinkOut]
- Loscertales J, Valenzuela FQ, Congregado M, Merchán RJ, Varela GG, Ramírez AT, et al. Video-Assisted Thoracic Surgery Lobectomy: Results in Lung Cancer. J Thorac Dis 2010;2:29-35.[LinkOut]
- Chu D. Video-assisted thoracoscopic surgery (VATS) anatomic lung resection. J Thorac Dis 2010;2:62-3.[LinkOut]
- Cao CQ, Munkholm-Laresn S, Yan TD. True video-assisted thoracic surgery for early-stage non-small cell lung cancer. J Thorac Dis 2009;1:34-8.[LinkOut]
- Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000;24:27-30; discussion -1.[LinkOut]
- McKenna RJ Jr, Wolf RK, Brenner M, Fischel RJ, Wurnig P. Is lobectomy by video-assisted thoracic surgery an adequate cancer operation? Ann Thorac Surg 1998;66:1903-8.[LinkOut]
- Lewis RJ, Caccavale RJ. Video-assisted thoracic surgical non-rib spreading simultaneously stapled lobectomy (VATS(n)SSL). Semin Thorac Cardiovasc Surg 1998;10:332-9.[LinkOut]
- Kaseda S, Aoki T. Video-assisted thoracic surgical lobectomy in conjunction with lymphadenectomy for lung cancer. Nippon Geka Gakkai Zasshi 2002;103:717-21.[LinkOut]
- Villamizar NR, Darrabie MD, Burfeind WR, Petersen RP, Onaitis MW, Toloza E, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25.[LinkOut]
- Flores RM, Park BJ, Dycoco J, Aronova A, Hirth Y, Rizk NP, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2009;138:11-8.[LinkOut]
- Hoksch B, Ablassmaier B, Walter M, Muller JM. Complication rate after thoracoscopic and conventional lobectomy. Zentralbl Chir 2003;128:106-10. German.[LinkOut]
- Roviaro G, Varoli F, Vergani C, Maciocco M, Nucca O, Pagano C. Video-assisted thoracoscopic major pulmonary resections: technical aspects, personal series of 259 patients, and review of the literature. Surg Endosc 2004;18:1551-8.[LinkOut]
- Shaw JP, Dembitzer FR, Wisnivesky JP, Litle VR, Weiser TS, Yun J, et al. Video-assisted thoracoscopic lobectomy: state of the art and future directions. Ann Thorac Surg 2008;85:S705-9.[LinkOut]
- Congregado M, Merchan RJ, Gallardo G, Ayarra J, Loscertales J. Video-assisted thoracic surgery (VATS) lobectomy: 13 years’ experience. Surg Endosc 2008;22:1852-7.[LinkOut]
- Solaini L, Prusciano F, Bagioni P, di Francesco F, Poddie DB. Video-assisted thoracic surgery (VATS) of the lung: analysis of intraoperative and postoperative complications over 15 years and review of the literature. Surg Endosc 2008;22:298-310.[LinkOut]
- Sawada S, Komori E, Yamashita M. Very long-term outcomes of video-assisted thoracoscopic surgery for lung cancer. Surg Endosc 2008;22:2407-11.[LinkOut]
- Wang B, Liu C, Shih C. Short-term results of thoracoscopic lobectomy and segmentectomy for lung cancer in Koo Foundation Sun Yat-Sen Cancer Center. J Thorac Dis 2010;2:64-70.[LinkOut]
- Hazelrigg SR, Cetindag IB, Fullerton J. Acute and chronic pain syndromes after thoracic surgery. Surg Clin North Am 2002;82:849-65.[LinkOut]
Cite this article as: Kim RH, Takabe K, Lockhart CG. Outcomes of a hybrid technique for video-assisted thoracoscopic surgery (VATS) pulmonary resection in a community setting. J Thorac Dis 2010;2(4):210-214. doi: 10.3978/j.issn.2072-1439.2010.11.5
|