Resection of pulmonary nodule in a patient with subglottic stenosis under modified spontaneous ventilation anesthesia
Introduction
Subglottic stenosis is an uncommon structural abnormality that can pose as a difficulty for patients undergoing surgery, and treatment is complex due to the special anatomical location. Pulmonary nodule resection in patients with subglottic stenosis is challenging and has not yet been reported. Here we present a case of pulmonary nodule resection in a patient with subglottic stenosis using uniportal thoracoscopy under spontaneous ventilation anesthesia (SVA). Compared with traditional double lumen endotracheal intubation, we believe this modified technique can significantly reduce airway trauma, and accelerate patient recovery. Patients’ written informed consent for the procedure and subsequent use of data were obtained.
Case presentation
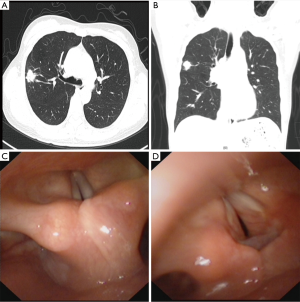
A 45-year-old female patient with a right lung nodule was admitted to our hospital. She had a history of a subtotal thyroidectomy under general anesthesia, which at the time postoperative pathology demonstrated Hashimoto’s thyroiditis. Three years after the resection, she once complained of hoarseness and dyspnea. Positron emission tomography-computed tomography scan showed a lobulated nodule (1.8 cm × 2.0 cm × 1.2 cm) in the posterior segment of the right upper lobe (RUL), SUVmax =3.8 (Figure 1A,B). Electronic laryngoscope demonstrated grade 2 narrowing of subglottic (obstruction had approximately 70% to 90% of the lumen obstructed), according to Cotton’s staging system to subglottic stenosis (1) (Figure 1C,D). Examinations revealed no other abnormalities.
After multidisciplinary consultation (Thoracic surgery, Anesthesiology, Otorhinolaryngology), we believed subglottic stenosis was remote and not required for special management. But it was difficult to perform conventional double lumen tracheal intubation in general anesthesia, which may cause difficulty in extubating the patient. Therefore, we made a backup plan. We would like to perform pulmonary nodule resection under SVA, meanwhile prepare for intubation if necessary. After specific explanation and patient approval, pulmonary nodule resection via uniportal thoracoscopy under SVA was performed.
Anesthesia and operation process
Mask oxygen inhalation was used during anesthesia induction. Thoracic epidural anesthesia (TEA) was performed as previously described (2). A laryngeal mask (LM) airway was used for oxygen inhalation lately, but the patient presented with inspiratory dyspnea. Fiber-optic bronchoscopy demonstrated vocal cords swelling in an olive shape.
We considered double lumen tube (DLT), but found it too large for intubation, and may increase the risk of airway trauma. Therefore, a 6.5 single lumen tube (SLT) (6.0 mm, Well Lead, China) was chosen for intubation of the patient under Glidescope to ensure oxygenation. The target nodule located in RUL, and the opening of right upper lobar bronchus was close to the carina. Therefore could the use of bronchial blockers not provide satisfactory lung isolation for the procedure to be performed. So we decided to perform a modified SVA involving TEA plus intravenous anesthesia with SLT endotracheal intubation without muscle relaxants (2-7).
Lidocaine (2%) was intermittently sprayed into the tube and synchronized intermittent mandatory (SIMV) mode was activated to assist ventilation. Thereafter dyspnea remitted, and blood oxygen saturation remained above 98%.
After 15 minutes of observation, the patient vital signs remained within normal limits and thus we proceeded with the operation. The patient was placed in the left lateral position, a 3 cm incision was made on the right anterior axillary line in the 5th intercostal space. When the operation began, SIMV mode was stopped and transferred to spontaneous ventilation. Intraoperative dexmedetomidine and etomidate was used for sedation and analgesia (3-5).
The surgeons sprayed 2% lidocaine on the lung pleura through surgical field and performed intrathoracic vagal blockade (2). A liner cut stapler was used to perform wedge resection. Intraoperative frozen biopsy confirmed benign granuloma. A chest drainage tube was placed and the incision was sutured.
During the operation, the vital signs were stable. Atrial blood gas analysis showed no hypoxia or hypercapnia. Five minutes after operation the patient was conscious. In order to prevent dyspnea caused by glottic mucosa edema, we inserted a hollow tube core (15 Fr, Well Lead China) from the endotracheal tube before extubation.
To avoid dyspnea following extubation, we inserted a hollow tube core (15 Fr, Well Lead China) from the SLT before extubation. We believe it ensures the safety of the patient during recovery after anesthesia. The patient was observed for 15 minutes; we then removed the tube core and sent her to Intensive care unit (ICU) for recovery.
The drainage tube was removed on the 2nd postoperative day. Postoperative recovery was uneventful and the patient was discharged on the 6th postoperative day. Postoperative pathologic suggested IGg4 associated lung disease, which involving multiple organs or tissues of chronic autoimmune disease. The patient with glottis mucosal swelling may be related to this disease (8). The follow-up time was six months with no complaint of hoarseness and dyspnea.
Comments
As far as we know, resection of pulmonary nodule in patient with subglottic stenosis has not yet been reported. In this paper, we describe a modified method of treating pulmonary disease with subglottic stenosis by using single lumen endotracheal intubation and retaining SVA. Single lung isolation under general anesthesia with a DLT is the standard mode of thoracic surgery (5). However, conditional double lumen endotracheal intubation in patients with subglottic stenosis may stimulate subglottic mucosal edema and thickening which could potentially lead to difficult decannulation. We therefore attempted uniportal thoracoscopic pulmonary nodule resection under SVA, and keeping the patient asleep.
The advantages of this modified method are multiple-fold and include: (I) SLT can play as a stent role which ensures ventilation and reduces the interference of subglottic stenosis, that may cause oedema and closing up of the stenosis and difficult extubation; (II) lung collapse achieved by creation of the surgical pneumothorax can provide satisfactory surgical field which facilitate thoracoscopic operation; (III) TEA with intravenous anesthesia reduces the amount of anesthetics, which reduces anesthesia-associated adverse effects; (IV) combined analgesia by epidural and intravenous has definite effect in the perioperative period, and facilitates postoperative rehabilitation; (V) TEA can block the inhibition of the diaphragm nerve reflex to improve diaphragmatic and respiratory function; and (VI) no postoperative residual neuromuscular blockade, accelerates the recovery of the patient (2-7,9). Meanwhile, in order to prevent dyspnea caused by abnormal circumstances, we inserted a small size tube from the endotracheal tube before extubation to prevent unpredicted accident.
In conclusion, uniportal thoracoscopic pulmonary nodule resection in a patient with subglottic stenosis under SVA is feasible. We believe that this new treatment can reduce the surgical trauma of subglottic stenosis of the patient, and subsequently allows for faster recovery of the patient.
Acknowledgements
We would like to acknowledge Lindsey Hamblin for correcting our English spelling and grammar.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Cotton RT. Pediatric laryngotracheal stenosis. J Pediatr Surg 1984;19:699-704. [Crossref] [PubMed]
- Guo Z, Yin W, Pan H, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis 2016;8:359-68. [Crossref] [PubMed]
- Dong Q, Liang L, Li Y, et al. Anesthesia with nontracheal intubation in thoracic surgery. J Thorac Dis 2012;4:126-30. [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation. J Thorac Dis 2014;6:31-6. [PubMed]
- Liu J, Cui F, He J. Non-intubated video-assisted thoracoscopic surgery anatomical resections: a new perspective for treatment of lung cancer. Ann Transl Med 2015;3:102. [PubMed]
- Pompeo E. Nonintubated video-assisted thoracic surgery under epidural anesthesia-Encouraging early results encourage randomized trials. Chin J Cancer Res 2014;26:364-7. [PubMed]
- El-Tahan MR, Regal M. Target-Controlled Infusion of Remifentanil Without Muscle Relaxants Allows Acceptable Surgical Conditions During Thoracotomy Performed Under Sevoflurane Anesthesia. J Cardiothorac Vasc Anesth 2015;29:1557-66. [Crossref] [PubMed]
- Kitada M, Matuda Y, Hayashi S, et al. IgG4-related lung disease showing high standardized uptake values on FDG-PET: report of two cases. J Cardiothorac Surg 2013;8:160. [Crossref] [PubMed]
- Murphy GS, Szokol JW, Avram MJ, et al. Postoperative residual neuromuscular blockade is associated with impaired clinical recovery. Anesth Analg 2013;117:133-41. [Crossref] [PubMed]


