Targeting CD47: the achievements and concerns of current studies on cancer immunotherapy
Introduction
During cancer development, cancer cells are often able to evade immune-surveillance through mechanisms like the down-regulation of specific tumor antigens and major histocompatibility complex (MHC). Therefore, understanding these mechanisms of escape is critical for developing novel cancer therapy. Cancer immunotherapy aims to re-activate the patients’ immune system for the elimination of cancer cells. It is currently a major focus of oncology research, and the results have shown impressive clinical efficacies.
Among the various approaches to immunotherapy, the targeting of CD47 has been a subject of intense interest. Some of the previous preclinical researches involving anti-CD47 therapy included studies in non-Hodgkin’s lymphoma (1), breast cancer (2), ovarian cancer (2), and others. A more recent study has demonstrated the efficacy of anti-CD47 monoclonal antibodies (mAbs) in eliminating xenograft small cell lung cancer tumors in mice when used in combination with anti-CD56 mAbs (3).
Based on these preclinical studies, anti-CD47 therapy has proceeded to clinical trials. At least three CD47 antagonists (Hu5F9-G4, CC-90002, and TTI-621) (Table 1) are currently in active phase I clinical trials, covering hematological malignancies and solid tumors (4). With the release of their safety profiles (5-7), more attention is now being focused on comparing the side effects (8) and efficacies of these inhibitory reagents. Despite the significant investment and rapid progression in pharmaceutical research and development, the detailed mechanisms of anti-CD47 therapies are still controversial. It is also unclear how well the findings in preclinical models will translate to clinical results.
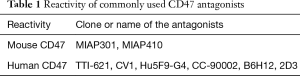
Full table
In this article, we will first discuss the role of antibody-dependent cell-mediated cytotoxicity (ADCC) in determining the clinical strategies of anti-CD47 therapy. Then, we will raise the concern that some of the preclinical xenograft models may potentially overestimate the clinical effectiveness of certain antagonists, and syngeneic models may be a more conservative choice for predicting efficacy. Lastly, we will compare the trial results based on concerns raised from existing studies.
Physiopathological functions of CD47
CD47, also named integrin-associated protein (IAP), is a widely expressed trans-membrane glycoprotein. It provides a “do not eat” signal by binding to the N-terminus of signal regulatory protein alpha (SIRPα) on immune cells and suppresses phagocytosis. CD47 down-regulation is involved in the clearance of red blood cells (RBCs) (9) and platelets (10) by splenic macrophages, which may cause hemolytic anemia and idiopathic thrombocytopenic purpura, respectively. Hematopoietic stem cells transiently up-regulate CD47 expression to escape phagocytosis by macrophages before and during mobilization (11). The pathological role of CD47 is commonly responsible for the escape of malignant cancer cells from immune-surveillance. CD47 overexpression is found to be associated with poor prognosis in leukemia (12), non-Hodgkin’s lymphoma (1), bladder cancer (13), breast cancer, and other cancers (2). Particularly, cancer stem cells are able to resist phagocytosis by overexpressing CD47 (12). These findings have widened the pharmaceutical interest in using CD47 as a potential therapeutic target to eliminate cancer cells.
Fragment crystallizable (Fc) dependency and independency
One major controversy underlying current anti-CD47 therapy development is whether the observed therapeutic effects are due to the specific intrinsic functions of CD47 or the non-specific ADCC. In the latter scenario, the Fc fragment carried by the intact immunoglobulin G (IgG) triggers the responses of macrophages, natural killer (NK) cells, and granulocytes.
This question is of great importance to anti-CD47 drug development, as it can tilt the balance between its cancer-killing effects and its potentially hazardous side effects on other CD47 expressing cells. If ADCC is predominant, tolerable toxicity may be achieved with a compromise in efficacy. However, it would be questionable whether anti-CD47 could provide any additional therapeutic benefit over the existing ADCC-based medications. On the other hand, if the efficacy is specific to CD47 intrinsic functions, it would be reasonable to separate ADCC from CD47 blockade. The ideal strategy would, therefore, be to combine CD47 antagonists that have minimal ADCC (3,14,15) with other therapeutic antibodies that can provide a strong ADCC effect.
To date, studies have demonstrated the presence of both mechanisms. The Fc region of anti-CD47 mAb can trigger ADCC through neutrophils (16) and macrophages. Several studies have also shown the presence of Fc-independent mechanisms. The knockdown of CD47 expression (17) and the use of anti-CD47 F(ab’)2 fragment alone (1) have successfully elicited macrophage phagocytosis. Another evidence for the Fc-independent mechanism comes from the synergistic effect on phagocytosis due to anti-CD47 mAbs in combination with the ADCC from other therapeutic mAbs. Such synergy has been observed in vivo with rituximab (1,6), anti-EGFR mAbs (6,18), and anti-CD56 mAbs (3); and in vitro with trastuzumab (16). Moreover, macrophages that are deficient in Fc receptors can still enable phagocytosis once incubated with intact anti-CD47 mAb (1). A recent original study (3) observed the structural resemblance between CD47-Hu5F9 binding interface and CD47-SIRPα binding interface. This is the first definitive evidence that the mechanism of anti-CD47 mAb Hu5F9 involves the disruption of the CD47 intrinsic functions.
Overestimation of CD47-SIRPα interaction
Animal models are limited in their ability to mimic the complex environment inside the human body. As a result, we feel the need to address some of the limitations that may have affected the interpretations of the above experiments. We raise the concern that CD47-SIRPα interaction may have been overestimated either by SIRPα of high affinity to CD47 in certain mouse models, or by the enhanced CD47 clustering in response to particular anti-CD47 mAb. Thus, these results should be interpreted in reference to species matched animal experiments and in vitro systems.
Superior affinity of Sirpα in NOD mice
A desirable animal model for the investigation of anti-CD47 should faithfully mimic the interaction between human CD47 and human SIRPα, elicit robust responses from both the innate and adaptive immunity, and recapitulate side effects of CD47 blockade on RBCs and platelets. The immunocompromised NSG mice have been widely adopted for xenograft experiments. However, the rationale and potential pitfalls of using NSG mice in CD47 research have not been well discussed; and therefore, whether it is the best choice for the study deserves further consideration.
Concerns have been raised over the suitableness of the SirpαNOD allele in NSG animals to the CD47 study (14,19). The binding affinity between human CD47 and SirpαNOD is about 10 times greater than with human SIRPα (20). Therefore, CD47-SIRPα inhibition could carry more weight in the process of macrophage phagocytosis in NOD-based xenograft models, and thus serves as the dominant factor in relative to ADCC and SIRPα-independent functions of CD47. It is conceivable that the effects of disrupting CD47-Sirpα would be greatly enhanced and more visible in these animals. In this sense, the observed efficacy in the absence of Fc region may not necessarily indicate Fc-independent mechanisms. Instead, it could be merely due to disrupting the stronger CD47-Sirpα interaction that is amplified in the NOD background. This speculation is supported by several non-NOD animal studies (see below). When translating to clinical applications, since the human SIRPα does not interact with CD47 as tightly (20), the anti-tumor effect of CD47-SIRPα inhibition might not be as significant in human patients. As a result, the real-world efficacy of anti-CD47 therapy could potentially be weaker than expected from the NOD-based xenograft models.
The above concern is rather plausible especially in the presence of ADCC. In contrast, in the absence of ADCC, contribution from CD47-SIRPα seems limited in the inhibition of phagocytosis. CV1, a SIRPα variant with high affinity for CD47, competes with endogenous SIRPα for CD47 binding. However, CV1 alone, as an Fc-free antagonist, cannot inhibit cancer growth in vivo (15). TTI-621, a recombinant fusion protein composed of the human SIRPα N-terminus linked to the Fc of IgG1, loses its efficacy when the Fc fragment is replaced with an IgG4 mutant without ADCC capability, despite maintaining its ability to disrupt CD47-SirpαNOD interactions (8). These results indicate that the CD47-SirpαNOD interaction does not predominate in the anti-phagocytic process in the absence of ADCC, and that anti-CD47 therapy is only meaningful in combination with ADCC. Nevertheless, it is possible that the CD47-SIRPα interaction may have differential response to pro-phagocytic signals of different strengths. The synergy between CV1 and other therapeutic mAbs (15) is so dramatic that possibility for overestimation of CD47-SirpαNOD interaction remains in the presence of ADCC. We suggest the researchers consider other animal models that better recapitulate CD47-SIRPα interaction in humans whenever available.
In addition, immunocompromised hosts lack the immune network that effectively responds to Fc fragments. With a weakened adaptive immunity, complement system, and/or NK cells, the ADCC-dependent efficacy and toxicity can be underestimated in immunocompromised xenograft animals.
Syngeneic non-NOD models
The concern over the enhanced affinity of SirpαNOD encouraged the use of non-NOD syngeneic models, in which mouse tumors are established in immunocompetent mice. In general, three merits of using such models are considered (14):
- A complex and robust immune network including all innate and adaptive immunity components;
- Better recapitulation of the in vivo antigen sink, including RBCs and other CD47 expressing cells;
- Bypass of the cross-species difference in the CD47-SIRPα interaction.
While the interspecies affinity between SirpαNOD and human CD47 is too high, the intraspecies affinity between mouse CD47 and mouse Sirpα is often one order of magnitude lower than that in humans, and this problem can be observed in multiple mouse strains (20). Nonetheless, the benefit of this cross-species difference is that it enables a conservative projection of the clinical efficacy.
In contrast to NSG hosts, anti-CD47 therapies using non-NOD genetic backgrounds often show weaker therapeutic effects. Syngeneic C57BL/6 model exhibits only mild and transient tumor inhibition upon multiple doses of anti-mouse CD47 mAb MIAP301 (19). Similarly, syngeneic FVB model also showed insignificant tumor inhibition upon MIAP301 administration (2). A different anti-mouse CD47 mAb MIAP410 did show significant inhibition of breast cancer growth in syngeneic FVB mice (2). However, this effect is likely due to the IgG1 origin of the antibody, which triggers robust and strong innate and adaptive immune responses. The same outcome was not observed when using mouse colon cancer CT26 and mouse melanoma B16 cell lines (21). A separate study using a CD47 antagonist nanobody lacking the Fc segment in combination with anti-programmed death-ligand 1 (PD-L1) mAb demonstrated killing of B16F10 melanoma in the C57BL/6 background, but failed to produce consistent results with CT26 (14). Since the nanobody does not possess Fc, the therapeutic outcome is Fc-independent. Thus, in human patients whose CD47-SIRPα interaction is stronger than that of the syngeneic animals, a better efficacy of targeting CD47 could be expected.
While the MIAP410 administration (2) and the anti-PD-L1 mAb combination therapy (14) mentioned above are of great scientific value, some of the results from other studies may be difficult to interpret. To elicit a robust immune response in immunocompetent animals, the use of appropriate Fc fragment is necessary. One syngeneic study administered an anti-mouse CD47 mAb MIAP301 of rat IgG2a into mouse immune system (19). Without appropriate Fc, the resulted immune response could also be substantially underestimated.
Perspective on other applicable animal models
In the ideal xenograft model, the affinity of SIRPα to CD47 should be lower than the NOD strain but higher than C57BL/6 and 129 strains. BALB/c may possibly be such a candidate (22). It may be necessary to investigate and compare the affinities between human CD47-SIRPα and human CD47-SirpαBALB/c, which would help determine whether BRG (BALB/c-Rag2nullIl2rγnull) animal would be a better substitute for NSG as the xenograft host for the study of human CD47.
To better mitigate the issue in SIRPα affinity observed in mouse models, researchers may consider some of the improved immunocompromised hosts, such as human SIRPα transgenic Rag2nullIl2rγnull (23). The introduction of human SIRPα better represents the role of CD47-SIRPα interaction in the human innate immunity, which allows for more accurate interpretations. The MISTRG host for immune humanization (24), which carries human thrombopoietin (TPO), interleukin-3, and granulocyte macrophage colony-stimulating factor (GM-CSF) for human macrophage reconstitution, is also a candidate for this purpose, but still requires further experimental validations. Xenograft models may be improved by immune humanization, similar to the approaches employed in anti-programmed cell death-1 (PD-1)/PD-L1 mAbs development (25). In addition, such models should require species matched IgG isotypes to exert their merits.
Species-matched phagocytosis assays
In in vitro systems, the cultured macrophages and the cancer cells can both be of human origin. Therefore, in theory, the intensity of the CD47-SIRPα interaction in these systems should resemble clinical scenarios. Several studies have explored the possibilities of testing the F(ab’)2 of anti-CD47 mAb in such systems.
Encouragingly, while the efficacy of the F(ab’)2 domain alone is greatly reduced compared to an intact antibody, it is still able to elicit phagocytosis at a level significantly higher than the control setting (1). In one study, the use of B6H12 Fab fragment produced a phagocytic index of approximately 50% when given alone (15). Despite a separate in vitro study reported that F(ab’)2 fragments did not elicit a phagocytic response in neutrophils (16), this does not exclude the possibility that other innate immune cells may respond to F(ab’)2 without Fc fragments.
Researchers should also take extra consideration when extrapolating the phagocytosis of RBCs onto the phagocytosis of cancer cells, particularly on the effect of F(ab’)2 (21). As noted before, ADCC and intrinsic CD47 function blockade should not be viewed as mutually exclusive mechanisms for anti-CD47 therapies, but two edges of the same sword, which can be specifically potentiated depending on the assay settings. The contribution from the two mechanisms might be very different in two different biological processes. Thus the extrapolation of existing knowledge from RBCs onto cancer cells might lead to additional inaccuracies.
CD47 clustering
In addition to SIRPα polymorphism, the clustering of CD47 can also influence the interaction between CD47 and SIRPα. For example, apoptotic cells are removed by innate immunity via reduced CD47 clustering instead of the down-regulation of CD47 (26).
A less discussed caveat of a widely adopted anti-CD47 non-blocking mAb 2D3 is that it increases CD47 clustering (27). This clone has been widely used as a control in different assay formats (12,15,17,28). The rationale behind its popularity is that its binding epitope is physically close to that of B6H12 and SIRPα (29). However, enhanced clustering and the resulted increase in CD47-SIRPα interaction could suppress the immune responses to this “control” antibody, thus leading to an overestimation of the apparent effects of anti-CD47. Evidence of such overestimation has not yet been observed in NSG xenograft models (1,12,17,28). As elucidated above, in NSG hosts, baseline phagocytosis has been strongly inhibited by SirpαNOD in these studies, therefore potentially masking the additional effects of extra CD47 clustering induced by 2D3. However, the application of 2D3 should be reconsidered when using human SIRPα or humanized xenograft models.
SIRPα-independent functions of CD47
While anti-CD47 mAbs have shown significant anti-cancer efficacies through both Fc-dependent ADCC and Fc-independent mechanisms, the role of SIRPα in this process has been controversial (1,12,15,16,28,30). While the anti-CD47 mAb B6H12 disrupts the interaction between CD47 and SIRPα, it can also affect the binding of CD47 to SIRPγ (31) and thrombospondin1 (TSP1) (32). This implies that anti-CD47 therapy might involve functions of CD47 that are independent from SIRPα, which also provides an alternative explanation to the efficacy of CD47 shRNA (17).
Stimulation of calreticulin (CRT), a pro-phagocytic molecule highly expressed on several cancer cells, might be a SIRPα-independent mechanism in anti-CD47 therapy. The absence of CRT abrogates the therapeutic effect of anti-CD47 mAb (33). Nonetheless, there lacks direct evidence that anti-CD47 could strengthen CRT function. It is possible that CRT is a prerequisite pro-phagocytic signal and does not necessarily receive regulation by CD47. The link between CD47 and CRT is also controversial. One study observed that macrophage phagocytosis is not decreased after blocking CRT on cancer cell, but rather diminished upon CRT blockade in macrophages (34).
In T cell migration, CRT and CD47 are found to bind to the N-terminus and C-terminus of TSP1 respectively (35). Simultaneous binding to TSP1 is required for appropriate signaling to modulate T cell mobility. Whether the physical interactions of CRT and CD47 with TSP1 could contribute to the regulation of phagocytosis deserves further exploration.
Comparison of the trial results and clinical perspectives
One important difference between TTI-621 and Hu5F9-G4 is the incidence of anemia and thrombocytopenia. In TTI-621 trials, 4/5 patients receiving 0.3 mg/kg dosages developed G3 and G4 platelet count events while maintaining stable hemoglobin levels (5). In contrast, out of the 16 patients in Hu5F9-G4 trial, there were 11 incidences of G1 and 5 incidences of G2 anemia, with no reported platelet events (7). These results show that the decoy receptor TTI-621 has a lower impact on RBCs compared to Hu5F9-G4, in spite of a higher general toxicity to other cells due to the strong ADCC from IgG1. It has been suggested that TTI-621 binds minimally to human RBCs (8), due to its specificity towards clustered CD47. Therefore, when human-specific spectrin skeleton restricts the clustering of CD47 on human RBCs, the decoy receptor does not recognize the dispersed CD47 distribution, thus decreasing the risk for anemia side effects.
The existing preclinical models include several types of thoracic cancers. These models suggest potential therapeutic outcomes for anti-CD47 treatments when applied in combination with other antibody treatments, such as rituximab for non-Hodgkin’s lymphoma (1), trastuzumab for breast cancer (16), anti-CD56 mAbs for small cell lung cancer (3), and anti-EGFR mAbs for colorectal and pancreatic cancer (6,18). The synergy of anti-CD47 with EGFR antagonists also implies its application in lung cancer. Moreover, anti-PD-1 mAb has been approved for non-small cell lung cancer, and its combination with CD47 antagonist also can be expected (14). As aforementioned, there exist factors overestimating the efficacy of anti-CD47 in these preclinical models, and the therapeutic effects vary significantly between different cancers. Physicians may not expect the clinical efficacy of these antagonists to be as significant as in some xenograft animals. Patients for anti-CD47 therapy should be cautiously selected based on the expression levels as well as the status of clustering of CD47.
Acknowledgements
The authors sincerely thank Dr. Teng Teng and Dr. Shentong Fang for reviewing the manuscript.
Funding: The present study was supported by the National Natural Science Foundation of China (81502247) and Major Project for Essential Drug Research and Development by the Ministry of Science and Technology (2014ZX09101005-004).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chao MP, Alizadeh AA, Tang C, et al. Anti-CD47 antibody synergizes with rituximab to promote phagocytosis and eradicate non-Hodgkin lymphoma. Cell 2010;142:699-713. [Crossref] [PubMed]
- Willingham SB, Volkmer JP, Gentles AJ, et al. The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci U S A 2012;109:6662-7. [Crossref] [PubMed]
- Weiskopf K, Jahchan NS, Schnorr PJ, et al. CD47-blocking immunotherapies stimulate macrophage-mediated destruction of small-cell lung cancer. J Clin Invest 2016;126:2610-20. [Crossref] [PubMed]
- Liu X, Kwon H, Li Z, et al. Is CD47 an innate immune checkpoint for tumor evasion? J Hematol Oncol 2017;10:12. [Crossref] [PubMed]
- Ansell S, Chen RW, Flinn IW, et al. A Phase 1 Study of TTI-621, a Novel Immune Checkpoint Inhibitor Targeting CD47, in Patients with Relapsed or Refractory Hematologic Malignancies. Blood 2016;128:1812.
- Chao MP, McKenna KM, Cha A, et al. Abstract PR13: The anti-CD47 antibody Hu5F9-G4 is a novel immune checkpoint inhibitor with synergistic efficacy in combination with clinically active cancer targeting antibodies. Cancer Immunol Res 2016;4:Abstract nr PR13.
- Sikic BI, Narayanan S, Colevas AD, et al. A first-in-human, first-in-class phase I trial of the anti-CD47 antibody Hu5F9-G4 in patients with advanced cancers. J Clin Oncol 2016;34:abstr 3019.
- Petrova PS, Viller NN, Wong M, et al. TTI-621 (SIRPαFc): A CD47-Blocking Innate Immune Checkpoint Inhibitor with Broad Antitumor Activity and Minimal Erythrocyte Binding. Clin Cancer Res 2017;23:1068-1079. [PubMed]
- Oldenborg PA, Gresham HD, Chen Y, et al. Lethal autoimmune hemolytic anemia in CD47-deficient nonobese diabetic (NOD) mice. Blood 2002;99:3500-4. [Crossref] [PubMed]
- Olsson M, Bruhns P, Frazier WA, et al. Platelet homeostasis is regulated by platelet expression of CD47 under normal conditions and in passive immune thrombocytopenia. Blood 2005;105:3577-82. [Crossref] [PubMed]
- Jaiswal S, Jamieson CH, Pang WW, et al. CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell 2009;138:271-85. [Crossref] [PubMed]
- Majeti R, Chao MP, Alizadeh AA, et al. CD47 is an adverse prognostic factor and therapeutic antibody target on human acute myeloid leukemia stem cells. Cell 2009;138:286-99. [Crossref] [PubMed]
- Chan KS, Espinosa I, Chao M, et al. Identification, molecular characterization, clinical prognosis, and therapeutic targeting of human bladder tumor-initiating cells. Proc Natl Acad Sci U S A 2009;106:14016-21. [Crossref] [PubMed]
- Sockolosky JT, Dougan M, Ingram JR, et al. Durable antitumor responses to CD47 blockade require adaptive immune stimulation. Proc Natl Acad Sci U S A 2016;113:E2646-54. [Crossref] [PubMed]
- Weiskopf K, Ring AM, Ho CC, et al. Engineered SIRPα variants as immunotherapeutic adjuvants to anticancer antibodies. Science 2013;341:88-91. [Crossref] [PubMed]
- Zhao XW, van Beek EM, Schornagel K, et al. CD47-signal regulatory protein-α (SIRPα) interactions form a barrier for antibody-mediated tumor cell destruction. Proc Natl Acad Sci U S A 2011;108:18342-7. [Crossref] [PubMed]
- Chao MP, Tang C, Pachynski RK, et al. Extranodal dissemination of non-Hodgkin lymphoma requires CD47 and is inhibited by anti-CD47 antibody therapy. Blood 2011;118:4890-901. [Crossref] [PubMed]
- Anti-CD47 targeting therapy for the treatment of colon and pancreas cancers. Available online: https://baylor-ir.tdl.org/baylor-ir/handle/2104/9649
- Liu X, Pu Y, Cron K, et al. CD47 blockade triggers T cell-mediated destruction of immunogenic tumors. Nat Med 2015;21:1209-15. [Crossref] [PubMed]
- Kwong LS, Brown MH, Barclay AN, et al. Signal-regulatory protein α from the NOD mouse binds human CD47 with an exceptionally high affinity-- implications for engraftment of human cells. Immunology 2014;143:61-7. [Crossref] [PubMed]
- Willingham SB, Volkmer JP, Weiskopf K, et al. Targeting CD47 on human solid tumors. Proc Natl Acad Sci U S A 2012;109:E2844-5. [Crossref]
- Iwamoto C, Takenaka K, Urata S, et al. The BALB/c-specific polymorphic SIRPA enhances its affinity for human CD47, inhibiting phagocytosis against human cells to promote xenogeneic engraftment. Exp Hematol 2014;42:163-171.e1. [Crossref] [PubMed]
- Strowig T, Rongvaux A, Rathinam C, et al. Transgenic expression of human signal regulatory protein alpha in Rag2−/−γc−/− mice improves engraftment of human hematopoietic cells in humanized mice. Proc Natl Acad Sci U S A 2011;108:13218-23. [Crossref] [PubMed]
- Rongvaux A, Willinger T, Martinek J, et al. Development and function of human innate immune cells in a humanized mouse model. Nat Biotechnol 2014;32:364-72. [Crossref] [PubMed]
- Stecklum M, Wulf-Goldenberg A, Brzezicha B, et al. Abstract B126: Correlation of tumor growth inhibition by check point inhibitors with PD-L1 expression in preclinical patient derived xenograft (PDX) models. Cancer Immunol Res 2016;4:Abstract nr B126.
- Lv Z, Bian Z, Shi L, et al. Loss of Cell Surface CD47 Clustering Formation and Binding Avidity to SIRPα Facilitate Apoptotic Cell Clearance by Macrophages. J Immunol 2015;195:661-71. [Crossref] [PubMed]
- Subramanian S, Parthasarathy R, Sen S, et al. Species- and cell type-specific interactions between CD47 and human SIRPalpha. Blood 2006;107:2548-56. [Crossref] [PubMed]
- Chao MP, Alizadeh AA, Tang C, et al. Therapeutic antibody targeting of CD47 eliminates human acute lymphoblastic leukemia. Cancer Res 2011;71:1374-84. [Crossref] [PubMed]
- Subramanian S, Boder ET, Discher DE. Phylogenetic divergence of CD47 interactions with human signal regulatory protein alpha reveals locus of species specificity. Implications for the binding site. J Biol Chem 2007;282:1805-18. [Crossref] [PubMed]
- Weiskopf K, Ring AM, Guo N, et al. Direct SIRPa blockade augments macrophage responses to therapeutic anticancer antibodies. Blood 2014;124:2729.
- Stefanidakis M, Newton G, Lee WY, et al. Endothelial CD47 interaction with SIRPgamma is required for human T-cell transendothelial migration under shear flow conditions in vitro. Blood 2008;112:1280-9. [Crossref] [PubMed]
- Bergström SE, Bergdahl E, Sundqvist KG. A cytokine-controlled mechanism for integrated regulation of T-lymphocyte motility, adhesion and activation. Immunology 2013;140:441-55. [Crossref] [PubMed]
- Chao MP, Jaiswal S, Weissman-Tsukamoto R, et al. Calreticulin is the dominant pro-phagocytic signal on multiple human cancers and is counterbalanced by CD47. Sci Transl Med 2010;2:63ra94. [Crossref] [PubMed]
- Feng M, Chen JY, Weissman-Tsukamoto R, et al. Macrophages eat cancer cells using their own calreticulin as a guide: roles of TLR and Btk. Proc Natl Acad Sci U S A 2015;112:2145-50. [Crossref] [PubMed]
- Li SS, Forslöw A, Sundqvist KG. Autocrine regulation of T cell motility by calreticulin-thrombospondin-1 interaction. J Immunol 2005;174:654-61. [Crossref] [PubMed]


