Thymic hyperplasia associated with primary Sjogren’s syndrome cured by thymectomy
Introduction
Primary Sjogren’s syndrome (pSS) is a relatively common autoimmune disease. Its main clinical manifestations are sicca syndrome involving lacrimal gland and salivary glands, besides, for a few patients, the joints and peripheral nervous system are also affected.
Thymic hyperplasia is often accompanied by autoimmune diseases such as systemic lupus erythematosus, myasthenia gravis and rheumatoid arthritis. While the case who suffered from thymic hyperplasia combined with primary Sjogren’s syndrome have rarely been reported (1,2). In our study, we will report a case of thymic hyperplasia associated with pSS cured by thymectomy.
Case presentation
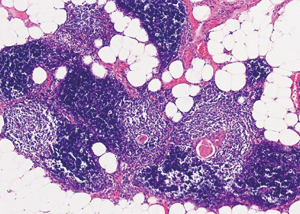
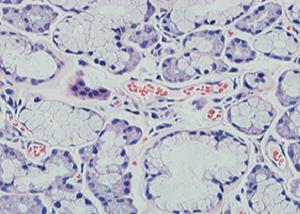
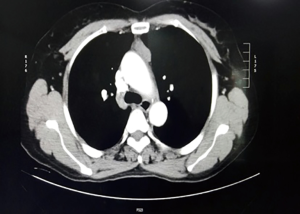
A 55-year-old woman complained chest distress, dryness of the oral cavity and eyes for 3 months. She was previously diagnosed as Sjogren’s syndrome (3), and was admitted to our hospital for further work-up and treatment on May 20, 2015. Laboratory studies revealed elevation of antinuclear antibodies, anti-SSA/Ro antibody, and reduction of CD3, CD4. Other laboratory analysis and immune indices were normal. The decreased secretion of the lacrimal and salivary glands was shown by Schirmer’s, chewing gum, and Saxon tests. The focal lymphocytic sialadenitis was shown by the lip biopsy (Figure 1). The patient had no experience of other autoimmune disease, collagen vascular diseases, acquired immunodeficiency disease, malignant lymphoma, or use of anticholinergic drugs. Chest computed tomography demonstrated anterior mediastinal mass shown as lower density, which measured 4×2.5×2.5 cm (Figure 2). In consideration of these, thymoma, thymic cyst, thymic carcinoma or teratoma was suspected, and a thymectomy was performed. The mass showed no adhesions to the adjacent mediastinal structures on the intraoperative observation. Macroscopically, the resected lesion was 4×2.5×2.5 cm in size, and located in the left part of the thymus. Thymic lymphoid hyperplasia was the pathological diagnosis (Figure 3). The patient was discharged without other therapy on June 3, 2015. After 1-year follow-up period, her sicca syndrome has been resolved and her laboratory examination has improved with regard to antinuclear antibodies, anti-SSA/Ro antibody, CD3 and CD4.
Discussion
The incidence rate (IR) of thymic lymphoid hyperplasia is relatively rare, it is often accompanied by autoimmune diseases such as systemic lupus erythematosus, allergic vasculitis, and Hashimoto thyroiditis. Our case was associated with Sjogren’s syndrome. Different from true thymic hyperplasia, thymic lymphoid hyperplasia is usually characterized by increased number of lymphoid follicles instead of thymic enlargement. Hiroshi Minato reported a case of Sjogren’s syndrome after thymic lymphoid hyperplasia associated with multilocular thymic cysts was diagnosed (4). The case we referred has been diagnosed as Sjogren’s syndrome before admitted in the hospital and her sicca syndrome has improved after the operation without other remedy.
The IR of pSS is 6.92 per 100,000 person-years. The average age is 56 years when they were first diagnosed (5). The clinical characteristic of this disease is functional disorder of exocrine gland, and then resulting in dryness of the oral cavity and eyes, even affect other organs systems, such as respiratory, urinary, and nervous system (6). There has no consensus about the diagnostic criteria of SS until 1993, when the European criteria was validated, and widely adopted (7). In our study, we defined the pSS by American European Consensus Group (AECG) classification criteria (3). Currently the treatment for Sjogren’s syndrome is mainly symptomatic therapies, such as artificial tears, artificial saliva, moisturizing skin lotions, and so on. In addition to this, corticosteroids and immunosuppressor are alternative for the treatment, but they are not applied widely because of their tremendous side effects. To date, the therapeutic strategies for the clinical manifestations have been insufficient because there is no statistically significant recommendable option. Based on these, similar as the function in myasthenia gravis, thymectomy maybe a useful choice for the treatment, especially for the patients with thymic lesions.
Conclusions
When we encounter a case with autoimmune disease such as Sjogren’s syndrome, we should consider the presence of thymic lesions. Although we do not know the mechanism for the association between thymic lesion and Sjogren’s syndrome, we think that it is an attemptable way for thymectomy to improve the sicca symptoms for the case of thymic hyperplasia associated with Sjogren’s syndrome.
Acknowledgements
We will thank Doctor Liu in the pathologic department in the first hospital for his assistance in pathology.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Kobayashi H, Ozeki Y, Aida S. Pulmonary and thymic lymphoid hyperplasia in primary Sjögren's syndrome. Jpn J Radiol 2009;27:107-10. [Crossref] [PubMed]
- Kondo K, Miyoshi T, Sakiyama S, et al. Multilocular thymic cyst associated with Sjögren's syndrome. Ann Thorac Surg 2001;72:1367-9. [Crossref] [PubMed]
- Vitali C, Bombardieri S, Jonsson R, et al. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 2002;61:554-8. [Crossref] [PubMed]
- Minato H, Kinoshita E, Nakada S, et al. Thymic lymphoid hyperplasia with multilocular thymic cysts diagnosed before the Sjögren syndrome diagnosis. Diagn Pathol 2015;10:103. [Crossref] [PubMed]
- Qin B, Wang J, Yang Z, et al. Epidemiology of primary Sjögren's syndrome: a systematic review and meta-analysis. Ann Rheum Dis 2015;74:1983-9. [Crossref] [PubMed]
- Holdgate N, St Clair EW. Recent advances in primary Sjogren’s syndrome. F1000Res 2016;5. pii: F1000 Faculty Rev-1412.
- Vitali C, Bombardieri S, Moutsopoulos HM, et al. Preliminary criteria for the classification of Sjögren's syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheum 1993;36:340-7. [Crossref] [PubMed]