Evolution of transbronchial needle aspiration - a hybrid method
Introduction
As a junior pulmonary fellow, I have been studying transbronchial needle aspiration (TBNA) with Dr. WANG, KP in the interventional pulmonology division of Johns Hopkins for one month. Although with little prior experience, after a systemic training program by Dr. Wang which includes slides presentation, video demonstration and hands on practice on a bronchial tree model, I feel confident and able to puncture the correct lymph nodes of every stations successfully. The goal of this paper is to share my TBNA learning experience and to summarize my understanding of the indication, anatomy, instruments and technique, and to discuss recent improvements and the future of TBNA.
The origin and historical evolution of TBNA
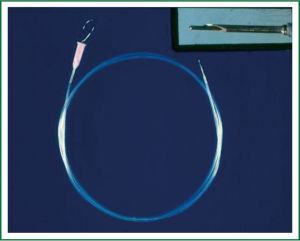
Transbronchial needle aspiration (TBNA) was first reported by Dr. Eduardo Schieppati, in 1949 with little attention (1). In 1978, Wang and colleagues at Johns Hopkins introduced this technique to North America and then the whole world. They described in detail the diagnosis of a paratracheal mass by TBNA biopsy through a rigid bronchoscope using a rigid 25-gauge esophageal variceal needle (2). In 1983, a flexible needle similar to the current EBUS needle (Figure 1) was developed for use with the flexible bronchoscope to perform TBNA (3). Shortly after this, in 1984, the efficacy and utility of TBNA in the diagnosis of peripheral pulmonary nodules was established (4). In 1985, a histology needle for the flexible bronchoscope was demonstrated (5). Wang published the results demonstrating the effectiveness of TBNA in the histological diagnosis of sarcoidosis in 1989 (6).
Indication
TBNA is indicated for biopsy of lesions underneath the mucosal surface or within the needle’s reach outside the lumen of the tracheobronchial tree. TBNA is used primarily for obtaining mediastinal or hilar lymph node tissue for the diagnosis and staging of bronchogenic and other metastatic carcinomas. Other important indications include the diagnosis of granulomatous, inflammatory and infectious diseases located in mediastinum and lungs. TBNA could be used also in the diagnosis of endobronchial lesions, and drainage of cystic lesions adjacent to the tracheobronchial tree.
Anatomy
For beginners, learning lymph node anatomy is not only of the greatest priority, but also the most difficult part. TBNA will not be effective if the needle miss the appropriate puncture site. Usually, CT scan, landmarks in the airway and occasionally fluoroscopy are used to guide selection of biopsy sites. Experienced bronchoscopists can easily recognize the consistent endobronchial location of common mediastinal lymph node chains. In 1994, Wang published a map of the mediastinal and hilar lymph node stations (total 11 stations) with CT and endobronchial correlations for each of the stations (7), which allowed for TBNA biopsy of the mediastinum in areas accessible from the airways (Figure 2).
These 11 nodal stations were selected because they can be sampled easily and safely with the TBNA technique. Also, they are consistently involved with metastatic tumor. In this system, carina, main right/left bronchus, both upper lobes and the bronchus intermedius were used as the important landmarks. The carina is defined on the CT scan by the change of shape of the trachea to triangular or oval shape or the appearance of the carina tip, which divides the trachea bronchus into right and left mainstem bronchi. This area usually is at the same level as the azygos arch. The following is a detailed description of the 11 nodal stations.
Station 1: Anterior carina LNs are defined as lymph nodes in front of the carina. To sample the anterior carina node, the needle is placed between the space of the first tracheal cartilage ring and the first bronchial cartilage ring, anteriorly and slightly toward the right.
Station 2: posterior carina LNs are defined as lymph nodes behind of the carina. The sample site is at the medial posterior wall of the right main bronchus which is directly opposite to the anterior carina LN.
Station 3: right paratracheal LNs are defined as lymph nodes above the azygoes arch and more superior and lateral to the anterior carina LN. The puncture site is located in the second to the fourth tracheal inter cartilagious space above the carina.
Station 4: left paratracheal LN is defined as the lymph node lateral to the left lower trachea. When it is below the aortic arch and above the pulmonary artery, it is also called the AP window lymph node. The AP window lymph nodes include left para-tracheal LNs and sub aortic lymph nodes. It can be LNs lateral to the left main bronchus. Considering the aortic arch and pulmonary artery, the needle must be placed very close to the tracheobronchial angulation as horizontal as possible to the trachea.
Station 5: right main bronchus LNs are defined as lymph nodes inferior and lateral to the anterior carina, the puncture space should be between the first two bronchial cartilage rings anteriorly.
Station 6: left main bronchus LN is defined as anterior to the left main bronchus. The puncture site is anterior to the space between the first two bronchial cartilages.
Station 7: right upper hilar lymph node is defined as in front of and between the right upper lobe and main bronchus. The puncture site for the right upper hilar is at the anterior aspect of the right upper lobe spur.
Station 8: sub carina LN is defined as the lymph node next to the medial wall of the right main bronchus. The puncture site of the sub carina LN is at the medial wall of the right main bronchus, proximal to the right upper lobe orifice.
Station 9: right lower hilar LN is defined as the lymph node at the anterior lateral aspect of the bronchus intermedius. The puncture site is at the right anterior lateral wall of the bronchus intermedius.
Station 10: sub-subcarinal LN is defined as medial to the bronchus intermedius. The puncture site is at the medial posterior wall of the bronchus intermedius below of the RUL bronchus.
Station 11: left hilar LN is defined as the lymph node in between the left upper and lower lobe bronchi. The puncture site is at the mid lateral wall of the left lower lobe bronchus, proximal to the superior segment orifice.
These nodal stations are not isolated from each other, but have regional relationships among themselves. They can be combined into 4 groups: right mediastinal LNs include1, 3, and 5; left mediastinal LNs include 4 and 6; central mediastinal LNs include 2, 8, and 10; hilar LNs include right side 7 and 9, as well as 11 in the left side. (Figures 3,4,5).



The following case will help to understand not only the LN anatomy (especially station 1, 3, 5), but also the sampling rules for staging of right lung cancer (Figure 6). This case was diagnosed as Non Small Cell Lung Cancer with TBNA biopsy positive at all stations including 4 (A-P window), 8 (subcarina), 3 (right paratracheal), 1 (anterior carina) and 5 (right main bronchus). It’s also worth noting that although the A-P window was hardly visible (Figure 4B,C) and a small sub-carina LN (Figure 4D), which still could be involved by cancer.

Originally, WANG LNs map was to guide TBNA biopsy but it is closely correlated with the current American Joint Committee On Cancer (AJCC) staging system (Figure 7, Table 1).

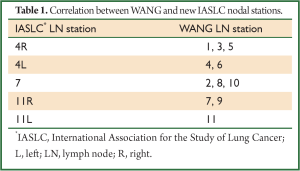
Full table
Technique
Before the procedure, the operator should review the radiology images to locate the lung nodules, masses and mediastinal lymph nodes involvement, using the WANG LN map to help select the proper LNs sites for needle puncture.
We would like to highlight the most common mistakes that the beginners tend to make resulting in a failed ineffective TBNA. (I) The needle did not penetrate the bronchial wall completely; (II) Inadequate angulation of the needle; (III) Lymph node missed despite adequate penetration and angulations.
Before the needle is inserted into the scope, the needle tip must be inside the metal hub. When the metal hub is visualized, the needle is advanced and locked. The whole catheter should be withdrawn to a point where only the distal tip of the needle is visible. Then the scope is advanced to the target area. After this, there are 4 methods described of needle insertion through the bronchial wall. First, Jabbing method: after the scope is fixed at the nose or the mouth by assistant, the needle is thrust through the inter cartilaginous space with a quick, firm jab. Second, Pushing method (piggy back method): after the needle tip cantacts the mucosa at the puncture site, the catheter is advanced until the hub is visible. Then, the catheter is fixed in relation to the scope at the proximal insertion port using the left hand fingers, and the scope is pushed forward at the distal end close to the nose by the right hand. The bronchoscope and catheter are actually pushed forward as a single unit until the entire needle penetrates the tracheobronchial wall. Often the jabbing and pushing technique are applied sequentially. Thirdly, occasionally, with the needle retracted, the distal end of the catheter (the metal hub) can be placed directly in contact with the mucosa and held firmly; then the needle is pushed in and locked. Usually the needle will penetrate through the tracheobronchial wall. If not, follow through with the jabbing or pushing technique. This was called the Hub against the wall method. All of these techniques can be used singly or in combination to insert the needle through the tracheobronchial wall. Occasionally, the cough of the patients may facilitate the penetration of the needle, which was referred as the Cough method.
The present status of conventional TBNA
Although TBNA has been around for 30 years, it is still underutilized (8). The recent development of EBUS-TBNA renewed interest and confidence in conventional TBNA (9,10). In a short 5 years it has proven to be a more attractive and reliable method than standard TBNA. Obvious reasons are with ultra sound (US) guides, the puncture site can be identified first and the puncturing of the needle into the lesson can be seen and confirmed by US. This allows the lesion to be sampled more successfully and bleeding complications can be avoided in contrast to conventional TBNA (C-TBNA).
EBUS-TBNA
The EBUS Scope has a side exit of 35-45 degree making the angulations of the needle toward bronchial wall easier and can allow afford the use of a stiffer needle which is easier to control and manipulate. The length of the needle and ability to advance and withdraw the needle inside the lesion repeatedly under US visualization is effective in obtaining an adequate sample, and sending the bloody clot specimen for histology has enhanced the diagnosis.
Inadvertent vessels puncture happens frequently with both technique (C-TBNA and EBUS-TBNA). It may even be more in EBUS-TBNA, which has never been proven to have any significant consequences. Successful puncture of the lesion can also be aided by using the WANG lymph node map without US. The success of TBNA depends on selection of the right puncture site under bronchoscope view.
The technique of puncture through the air way into the LN is the same with both C-TBNA and EBUS-TBNA. Confirming that C-TBNA has the lesion is judged by experience and by observing the angle and depths of the needle or by a more certain end point like rapid on-site evaluation (ROSE) instead of US.
One question is whether EBUS-TBNA has a higher yield than C TBNA and why. In EBUS TBNA, the yield will be high and there might be less variation among the experts because they all use US confirmation that the needle is in the lesion. In conventional TBNA there is no similar end point. Another important factor is that conventional TBNA training is not as vigorous as EBUS TBNA. For the beginnerthe needle may never puncture through the wall and the operator may not know it because they let the catheter of needle extended to far out the tip of the scope, or the angle and depth of the penetration are inadequate or the target is missed even with good angle and depth. With adequate training all of these mistakes can be avoided. But what constitutes good training in C-TBNA? It is unlikely one will or can start doing E-TBNA without training but most C-TBNA is performed without any hands-on training. Knowledge of anatomy, technique, and preparation of specimen and interpretations of the cytology and histology of specimens all play important roles. But the technique' skill is the most important factor.
Slide presentations, video demonstration, and hands on instruction, followed by practice are all important elements for adequate trainings. It may take several hours or days depending on the basic skills of the bronchoscopist. It will be of interest to know, given equal effort of training or leaning for each technique, which one is easier to learn and perform. Arguing which technique is better and which one should be used depends on several factors. In my experience if one is well trained in both techniques the differences will be trivial. What to use depends on one,s experise, and the availability and affordability of an EBUS scope.
The future of TBNA
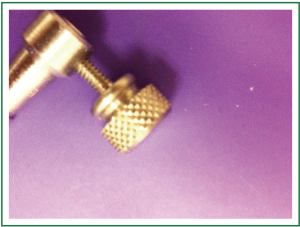
The development of a scope which has both the ability and ease of use of TBNA as a standard bronchoscope and also has the capability of US is needed (11). In the interim, we propose a hybrid C-TBNA technique, which is much more dependable and easier to do by adding a “fixer” to hold the catheter onto the scope while using only the pushing technique (Figure 8). This will eliminate the common mistakes of C-TBNA, such as protruding the catheter too far out during jabbing technique or forgetting to fix or ineffective fixation of the catheter to the scope during use of the pushing technique. Using an adapter to fix the needle catheter to the scope and using the pushing technique, will cause less confusion, but it will ensure the penetration and adequate angle and depth of the needle. Moving the needle back and forth inside the lesion is accomplished by pulling the scope back and forth using the pushing technique to core the tissue (Videos 1,2).
Ideally, TBNA should use both the endo view landmarks and the US landmarks as a guide to sample the LNs. This hybrid method of using a fixer with C-TBNA inspired by EBUS-TBNA will make conventional TBNA more reliable and dependent in the future.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Schieppati E. Mediastinal puncture thru the tracheal carina. Rev Asoc Med Argent. 1949;63:497-9. [PubMed]
- Wang KP, Terry P, Marsh B. Bronchoscopic needle aspiration biopsy of paratracheal tumors. Am Rev Respir Dis 1978;118:17-21. [PubMed]
- Wang KP, Terry PB. Transbronchial needle aspiration in the diagnosis and staging of bronchogenic carcinoma. Am Rev Respir Dis 1983;127:344-7. [PubMed]
- Wang KP, Haponik EF, Britt EJ, et al. Transbronchial needle aspiration of peripheral pulmonary nodules. Chest 1984;86:819-23. [PubMed]
- Wang KP. Flexible transbronchial needle aspiration biopsy for histologic specimens. Chest 1985;88:860-3. [PubMed]
- Wang KP, Fuenning C, Johns CJ, et al. Flexible transbronchial needle aspiration for the diagnosis of sarcoidosis. Ann Otol Rhinol Laryngol 1989;98:298-300. [PubMed]
- Wang KP. Staging of bronchogenic carcinoma by bronchoscopy. Chest 1994;106:588-93. [PubMed]
- Prakash UB, Offord KP, Stubbs SE. Bronchoscopy in North America: the ACCP survey. Chest 1991;100:1668-75. [PubMed]
- Herth FJ, Becker HD, Ernst A. Ultrasound-guided transbronchial needle aspiration: an experience in 242 patients. Chest 2003;123:604-7. [PubMed]
- Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004;126:122-8. [PubMed]
- Xiang Y, Zhang F, Akulian J, et al. EBUS-TBNA by a new Fuji EBUS scope (with video). J Thorac Dis 2013;5:36-9. [PubMed]