Primary tracheal schwannoma treated by surgical resection: a case report
Introduction
Primary tracheal tumors are uncommon, and account for only 1% of all tumors (1). Most of these tumors are squamous cell carcinoma (malignant) and adenoid cystic carcinoma (intermediate malignant) (2). As one of the extremely rare benign primary tracheal tumors, primary neurogenic tracheal tumors, which are divided into two categories: schwannoma and neurofibroma (1), account for less than 0.5% of primary tracheal tumors (3). The rarity and non-specific symptoms of these benign primary tracheal tumors always leaded to misdiagnosis and delayed treatment, and also undefined the optimal treatment. Here we reported a case of primary tracheal schwannoma in proximal trachea treated by surgical resection.
Case presentation
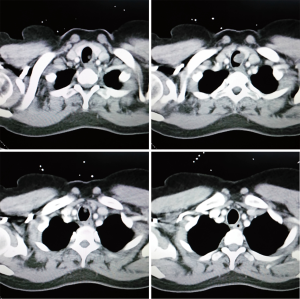
A 45-year-old woman had a history of progressive shortness of breath and dry cough for several years. The symptoms exacerbated two weeks before her admission. She was a non-smoker with no other pulmonary diseases. During the course of disease, she had been misdiagnosed and treated as asthma or bronchitis for several times with normal chest X-rays. In this admission, some light wheezes were auscultated from cervical part of trachea. The respiratory function (FEV1 =2.14), other physical examinations and biochemical tests were all normal. Enhanced CT scan revealed an intra-luminal tracheal mass invaded the left side of tracheal wall without enhancement (Figure 1), no enlarged lymph nodes were detected. A bronchoscope was performed for location of the mass, the result showed that the superior margin of the wide-pedicle mass was on the level of 4th trachea cartilage ring with intact capsule, the mass occupied about 2/3 transverse section of the lumen, and two cartilage rings was involved.
The patient underwent surgical treatment. A smaller size of tracheal cannula was used for intubation. The patient was positioned as thyroid surgical posture, a transverse incision was made 3 cm above suprasternal fossa. As full traction of thyroid, the trachea was exposed sufficiently with no extra-luminal invasion. After confirmation of the 4th trachea cartilage ring, the anterior wall of trachea was transversely cut at the level of upper edge of 4th cartilage ring to expose the superior margin of the tumor. The tumor was involved the left side of tracheal wall, the pedicle was about 1.0 cm in diameter. Subsequently, another transverse incision was made at the level of upper edge of 6th cartilage ring to identify the inferior margin of the tumor. The tumor was excised along the pedicle without cutting the posterior wall of trachea. The tumor was 1.5 cm in diameter with smooth and intact capsule, the margin was negative. At last, the trachea was repaired by manual interrupted sutures.
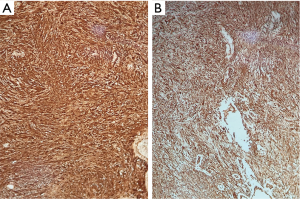
The pathological result demonstrated two areas of the tumor: Antoni type A and B, which means areas of high and low cellularity respectively (Figure 2). Immunohistochemical result revealed positivity for S-100 protein and Vimentin (Figure 3). The diagnosis of schwannoma was confirmed.

Discussion
Primary neurogenic tracheal tumors (neurofibroma and schwannoma) can occur in any age. Neurofibroma has been reported only in male patients, while schwannoma has a predilection for female patients (1). Schwannoma in trachea was first reported by Straus in 1951 (4), the tumor arises from Schwann cells of intra-luminal never sheath, and mostly occurred in the distal of trachea (5), the tumor in this case was in the proximal of trachea. Schwannoma in trachea is so rare that only 23 cases have been reported from 1951 to 2003 (1).
Because of the flexibility of trachea, patients with tumors in trachea usually have no symptoms in the early stage of disease. Only when the trachea is occupied over 50%, the patients will present some non-specific symptoms like shortness of breath and dry cough, or repeated inspiratory dyspnea in serious cases (6). These patients are prone to be misdiagnosed and treated as some respiratory diseases, so CT scan, MRI or bronchoscope are necessary for patients with above symptoms after a long time of treatment. Chest X-ray is not efficient enough to detect a mass in trachea because of the superimposition of vertebra and mediastinum, this might also contribute to delayed diagnosis.
Treatment of primary tracheal schwannoma now includes surgery and bronchoscopic resection. Bronchoscope is important in the diagnosis of primary tracheal tumors, it can facilitate the location of tumor and give instructive information for both intubation and surgery. However, it is concerned that bronchoscopic resection was associated with high rate of residual tumor, a rate of 46.2% was reported by Kasahara (7). Some other studies revealed a recurrence rate of about 50% after bronchoscopic treatment (8,9), so we consider surgery as the first choice of treatment of primary tracheal schwannoma, surgery can provide radical resection for both extra-luminal and intra-luminal tumors as no recurrence case has been reported after surgical treatment. The most important step of the surgical treatment is end-to-end tracheal anastomosis, which follows the strict hemostasis. As schwannoma rarely has malignant present, a wedge resection or segmental resection will be enough for complete remove of tumor (8-10). For tumors in distal respiratory tract, such as carina or bronchus, reconstruction of airway (sleeve resection, reconstruction of carina and bronchus, lobectomy or pneumonectomy) will be performed according to the location and size of tumors.
Above all, primary tracheal schwannoma is a kind of extremely uncommon benign tumors with non-specific symptoms, which result to high risk of delayed diagnosis. For patients with repeated respiratory symptoms, chest CT or MRI scan play an important role in the diagnosis of tracheal tumors. Surgery is superior to bronchoscopic treatment in the term of recurrence rate from current scattered case reports.
Acknowledgements
We are grateful to Dr. Wen-Qing Feng (Ruijin Hospital, Shanghai Jiaotong University School of Medicine) for contacting support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Righini CA, Lequeux T, Laverierre MH, et al. Primary tracheal schwannoma: one case report and a literature review. Eur Arch Otorhinolaryngol 2005;262:157-60. [Crossref] [PubMed]
- Grillo HC, Mathisen DJ. Primary tracheal tumors: treatment and results. Ann Thorac Surg 1990;49:69-77. [Crossref] [PubMed]
- Hamdan AL, Moukarbel RV, Tawil A, et al. Tracheal schwannoma: a misleading entity. Middle East J Anaesthesiol 2010;20:611-3. [PubMed]
- Straus GD, Guckien JL. Schwannoma of the tracheobronchial tree. A case report. Ann Otol Rhinol Laryngol 1951;60:242-6. [Crossref] [PubMed]
- Mathisen DJ. Tracheal tumors. Chest Surg Clin N Am 1996;6:875-98. [PubMed]
- Erol MM, Uzun H, Tekinbas C, et al. A case of intratracheal schwannoma presenting at the emergency department with a diagnosis of asthmatic attack. J Emerg Med 2010;39:589-91. [Crossref] [PubMed]
- Kasahara K, Fukuoka K, Konishi M, et al. Two cases of endobronchial neurilemmoma and review of the literature in Japan. Intern Med 2003;42:1215-8. [Crossref] [PubMed]
- Dorfman J, Jamison BM, Morin JE. Primary tracheal schwannoma. Ann Thorac Surg 2000;69:280-1. [Crossref] [PubMed]
- Horovitz AG, Khalil KG, Verani RR, et al. Primary intratracheal neurilemoma. J Thorac Cardiovasc Surg 1983;85:313-7. [PubMed]
- Ma CK, Raju U, Fine G, et al. Primary tracheal neurilemoma: report of a case with ultrastructural examination. Arch Pathol Lab Med 1981;105:187-9. [PubMed]