Systemic inflammatory response syndrome, sequential organ failure assessment, and quick sequential organ failure assessment: more pieces needed in the sepsis puzzle
Sepsis remains the most common cause of death in critically ill patients in non-coronary intensive care units (ICUs) (1), while its reported incidence has been steadily increasing during the past three decades (2). Furthermore, many survivors of sepsis would still suffer from long-term physical, psychological, and cognitive disorders (3,4).
While recognizing the limitations of previous definitions of sepsis based on systemic inflammatory response syndrome (SIRS), an international task force presented a newly revised sepsis definition, i.e., sepsis-3. Sepsis has now been defined as a dysregulated host response to infection leading to life-threatening organ dysfunction, which can be identified as an acute increase in total sequential organ failure assessment (SOFA) score ≥2 (5). In addition, a quick SOFA score (qSOFA) has been proposed as a screening tool in the non-ICU setting to identify patients with suspected infection who are likely to develop sepsis (5). However, an accompanying editorial advocated prospective, real-world validation of qSOFA before routine implementation in clinical practice (6).
Based on a prospectively collected, observational database of 8,871 patients with presumed or confirmed infection presenting to the emergency department of Royal Brisbane and Women’s Hospital, Brisbane, Australia, Williams and coworkers tried to describe the prognostic and diagnostic performance of SIRS and qSOFA (7).
One major finding of the study was that SIRS was associated with organ dysfunction (defined by sepsis-2 or sepsis-3 criteria) and mortality, which was not unexpected. Although inconsistent with previous studies (5), it is intuitive that abnormalities in physiological parameters, especially vital signs as in SIRS (temperature, heart rate, and respiratory rate), are more common in patients with organ dysfunction. For example, we often teach our medical students or junior physicians that tachypnea is usually a sensitive, although nonspecific, surrogate marker of the severity of critically illness. Moreover, it is of note that the authors did not specify when exactly the criteria for SIRS and/or acute organ dysfunction were fulfilled (7). It is self-explanatory that critically ill patients who are already in the stage of organ dysfunction are more likely to have abnormal vital signs recorded in the nursing chart. In the meanwhile, it would also be very interesting to find that abnormal vital signs are of prognostic value for organ dysfunction during the disease progress. In addition, the authors reported that SIRS and qSOFA showed similar discrimination for organ dysfunction, as suggested by area under the receiver operating characteristic curve (AUROC) (0.72 vs. 0.73). However, for fair comparison of performance, AUROC could be inaccurate when the two ROC curves were crossing each other (8).
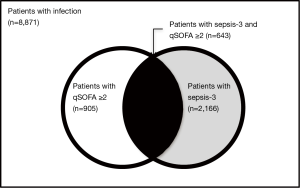
Another major finding was the low sensitivity of qSOFA score in patients with sepsis-3. Among the 8,871 patients with potential infection who were enrolled in the study, 2,166 patients (24.4%) met sepsis-3 criteria. The authors reported that although qSOFA score ≥2 was highly specific for sepsis-3 (96.1%), sensitivity was very poor (29.7%) (7). It is very important to bear in mind that qSOFA score has been developed as an effective way of raising suspicion of sepsis in general wards (9). Such a low sensitivity indicates that more than 70% of patients with sepsis-3 will be missed if we rely solely on the qSOFA score to identify these high-risk patients. Likewise, in a prospective cohort study in 30 emergency departments in 4 countries that enrolled 879 patients with suspected infection during 4-week period, use of qSOFA score would miss at least 26.6% patients with sepsis-3 (10). As a result, it is interesting to know whether this group of patients, i.e., patients fulfilling sepsis-3 but not qSOFA criteria, has a similar outcome as those patients meeting both sepsis-3 and qSOFA criteria (Figure 1). On the other hand, 262 patients out of 905 patients (29.0%) meeting qSOFA criteria did not have sepsis-3 (7). This group of patients will be misdiagnosed as sepsis and treated as such if not followed up by assessment of organ dysfunction. However, whether this group of patients, i.e., patients fulfilling qSOFA but not sepsis-3 criteria, has a better clinical outcome than those with “real” sepsis still awaits prospective validation (Figure 1).
Last, but not the least, according to definition (5), sepsis-3 denotes a clinical syndrome less severe than severe sepsis, and therefore should bear a lower mortality rate. After publication of sepsis-3 definition, many sepsis trials in the future will employ the new sepsis-3 definition instead of severe sepsis as inclusion criteria. Theoretically, this will result in enrollment of less critically ill patients with sepsis in clinical trials. From previous studies of sepsis, we understand that the less severe the enrolled patients are, the less likely the study exerts a positive result. For example, Eichacker and colleagues demonstrated that the efficacy of anti-inflammatory agents during sepsis was dependent on the risk of death, suggesting that anti-inflammatory agents had greater treatment effects in animal models compared with clinical trials because preclinical studies were done at significantly higher risks of death (11). If this were the case, enrollment of septic patients according to the recent sepsis-3 criteria might lead to even more negative clinical trials. As an example, a prospective, multicenter, placebo-controlled, randomized clinical trial found that use of hydrocortisone did not reduce the risk of septic shock among adults with severe sepsis not in septic shock (12). Contrary to the above deductions, Williams and coworkers reported that 30-day mortality associated with organ dysfunction based on sepsis-2 (severe sepsis) and sepsis-3 was similar (12.5% vs. 11.4%, difference 1.0%, 95% confidence interval −1.1% to 3.2%) (7). Whether this represents the reality or just a random finding merits further investigation due to its potential clinical significance.
In conclusion, new sepsis-3 criteria, especially qSOFA score, need to be validated in prospective cohort studies in different clinical settings, before it can be introduced into clinical practice. It is also important to understand the clinical significance of different patient groups according to the sepsis-3 criteria, including patients fulfilling both sepsis-3 and qSOFA criteria, patients fulfilling sepsis-3 but not qSOFA criteria, patients fulfilling qSOFA but not sepsis-3 criteria, and patients fulfilling neither criteria.
Acknowledgements
Funding: This study was funded, in part, by the Capital Clinical Application Research grant (Z1311017002213112) from the Science and Technology Commission of Beijing, and Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (CIFMS) 2016-I2M-1-014.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644-55. [Crossref] [PubMed]
- Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003;348:1546-54. [Crossref] [PubMed]
- Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010;304:1787-94. [Crossref] [PubMed]
- Cuthbertson BH, Elders A, Hall S, et al. Mortality and quality of life in the five years after severe sepsis. Crit Care 2013;17:R70. [Crossref] [PubMed]
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016;315:801-10. [Crossref] [PubMed]
- Abraham E. New definitions for sepsis and septic shock: continuing evolution but with much still to be done. JAMA 2016;315:757-9. [Crossref] [PubMed]
- Williams JM, Greenslade JH, McKenzie JV, et al. SIRS, qSOFA and organ dysfunction: insights from a prospective database of emergency department patients with infection. Chest 2017;151:586-96. [Crossref] [PubMed]
- Saito T, Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 2015;10:e0118432. [Crossref] [PubMed]
- Vincent JL, Martin GS, Levy MM. qSOFA does not replace SIRS in the definition of sepsis. Crit Care 2016;20:210. [Crossref] [PubMed]
- Freund Y, Lemachatti N, Krastinova E, et al. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA 2017;317:301-8. [Crossref] [PubMed]
- Eichacker PQ, Parent C, Kalil A, et al. Risk and the efficacy of anti-inflammatory agents: retrospective and confirmatory studies of sepsis. Am J Respir Crit Care Med 2002;166:1197-205. [Crossref] [PubMed]
- Keh D, Trips E, Marx G, et al. Effect of hydrocortisone on development of shock among patients with severe sepsis: the HYPRESS randomized clinical trial. JAMA 2016;316:1775-85. [Crossref] [PubMed]


