Higher coronary artery calcification score is associated with adverse prognosis in patients with stable angina pectoris
Introduction
Coronary artery calcification (CAC) is defined as a lesion of at least 130 Hounsfield units (HU) resulting from a plaque with an area of three contiguous pixels (at least 1.00 mm2). The CAC score is calculated using automatic analysis software, and this score favourably and quantitatively correlates with the area of atherosclerotic plaques (1,2). A CAC indicates the presence of atherosclerotic lesions, and CAC and atherosclerotic lesions are generally positively correlated (3). Moreover, a recent study showed CAC is more likely to cause stable angina pectoris (SAP) than unstable angina pectoris (4), and the CAC score directly correlates with the incidence of major adverse cardiac events (MACE) of patients with coronary artery disease (CAD) after coronary stenting (5). Recent studies have suggested that the CAC score may predict prognosis, including the rate of death and MI, in patients with CAD, but the value of the CAC score for evaluating the prognosis of patients with SAP is unknown (6,7). In the present study, we evaluated the prognostic value of CAC scores in patients with SAP.
Methods
Study population
The study population consisted of 106 consecutive patients with SAP aged 44 to 90 years (mean-age: 70.26±8.89 years), and 74 percent of the subjects were male; all patients under went multi-slice computer tomography (MSCT), and their CAC scores were evaluated. Patients were recruited from the Emergency and Cardiology Departments of Wuxi No. 2 Hospital of Nanjing Medical University and divided into a lower CAC score group (CAC score, ≤300, n=66) and a higher CAC score group (CAC score, >300, n=40). We obtained the clinical characteristics of these patients from their medical records, including previous history (hypertension, diabetes mellitus, hyperlipidaemia and smoking) and laboratory characteristics. The inclusion criteria were defined based on the definition of SAP from the 2013 ESC guidelines on the management of stable CAD (8). However, patients with acute coronary syndrome, previous myocardial infarction, a history of PCI or coronary artery bypass grafting (CABG), end-stage liver disease and renal disease were excluded from the study.
The research protocol was approved by the Ethics Committee of Wuxi No. 2 Hospital. All subjects signed an informed consent form before participating in this study.
Laboratory characteristics
The blood samples were obtained after fasting for a minimum of 8 h. At our hospital, haematology samples were assessed using a Beckman-Coulter LH750 system (Beckman Coulter, Inc. CA, USA), and the level of creatinine (Cr), lipids [total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C)] were assessed using an Olympus 5421 instrument.
MSCT and CAC scores
All MSCT examinations were performed using a 640-row scanner (TOSHIBA, Tokyo, Japan), and the following scanning parameters were used for the unenhanced calcium scoring scan: 120 kV tube voltage, 450 mAs tube current, 0.35 s rotation time and 0.5 mm slice thickness. CAC measurements were performed with the CaScoring software by two experienced readers blinded to the patient information, and the calcification area of each coronary artery was marked. The CAC score was defined by Agatston et al., and the software automatically obtained the integral and total values of the calcification of the coronary artery and its main branches. The degree of calcification was stratified based on the CAC score: the absence of calcified plaque received a score of 0, minimal plaques received scores of 1 to 10, mild plaques received scores of 11 to 100, moderate plaques received scores of 101 to 400, and severe plaque received scores >400 (2).
Recently, many studies have indicated that CAC scores >300 represent a strong predictor of MACE and provide predictive information for prognosis in patients with SAP (9,10). Therefore, in our study, the samples were divided into two groups according to their CAC scores: a lower CAC score group (CAC scores ≤300) and a higher CAC score group (CAC scores >300).
Coronary angiography and percutaneous coronary intervention (PCI)
Selective coronary angiography and PCI were performed at our catheterization laboratory via the radial or femoral artery by experienced cardiologists who were blinded to the clinical data and CAC score; the subjects were randomised and selected from quantitative coronary angiography results; CAD was defined as lesions with stenosis diameters exceeding 75% of the diameter of one of the major epicardial coronary arteries or its branches or a ≥50% narrowing of the left main coronary artery (11). All lesions with stenosis diameters exceeding 75% of a ≥2 mm coronary artery or a more than 50% narrowing of the left main coronary artery were subjected to PCI. Successful PCI was defined as a residual stenosis ≤20%.
Follow-up and MACE
All participants were followed-up for MACE consisting of a combined end point of death, non-fatal myocardial infarction, target lesion revascularisation (PCI or CABG) and rehospitalisation for cardiac ischaemia events (typical ischaemia chest pain, a positive stress test result or coronary angiography indicating ischaemia); the event-free survival time, which represented the time from hospital discharge to the occurrence of the MACE, was recorded.
Statistical analyses
Continuous variables are expressed as the mean ± standard deviation (SD) values or medians [interquartile range (IQR)], whereas categorical variables are expressed as percentages. Independent Student’s t-test and Mann-Whitney U test were used to compare two groups, and a one-way analysis of variance (ANOVA) and Kruskal-Wallis H test were used to compare multiple groups. The chi-squared test was used to assess qualitative data. Kaplan-Meier survival curves were used to calculate the cumulative event rates, and a Cox regression analysis was employed to analyse the relationship between risk factors and MACE. The log (CAC score) is expressed per 1 SD (SD =772.5 Agatston units) so the effect estimates could be compared. All statistical analyses were performed using the SPSS 17.0 software (IBM Corporation, New York, NY, USA). P<0.05 was considered to indicate a significant difference.
Results
Clinical characteristics of the study subjects
The CAC scores ranged from 6–300 in the lower CAC group and 305–5,183 in the higher CAC group. As shown in Table 1, the baseline characteristics did not significantly differ between the groups except for the age, Cr level, and rates of MACE and PCI. Compared with the lower CAC score group, the higher CAC score group was significantly older (72.83±9.7 vs. 68.65±7.99 years), had a higher Cr (84.95±23.28 vs. 73.44±18.52 mol/L), had higher CAC scores [609 (IQR: 429–1,275) and 116 (IQR: 50–205)], and had higher rates of PCI (43 vs. 23) and MACE (48 vs. 23); P<0.05 for all.
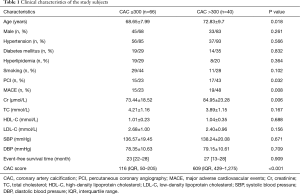
Full table
Relationship between CAC scores and clinical characteristics
The results in Table 1 show that the age, Cr levels, incidence of MACE and incidence of vascular disease were significantly associated with the CAC score; generally, patients with MACE had higher CAC scores than did patients without MACE [161 (IQR, 64–402) and 148 (IQR, 296–680); P<0.001; respectively], and the prevalence of coronary vessel disease directly correlated with the CAC score [238 (IQR, 117–294), 264 (IQR, 134–304) and 1,664 (IQR, 232–3,096), P=0.005]. Moreover, a higher than median age correlated with a higher CAC score [160 (IQR, 57–389) and 130 (IQR, 300–631), respectively; P=0.022], and subjects with a higher than median Cr level also had higher CAC scores [140 (IQR, 64–393) and 144 (IQR, 305–653), respectively; P=0.031]. The results are shown in Figure 1A-D.
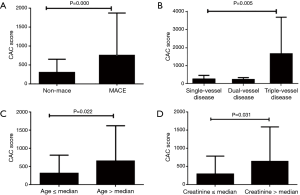
Relationship between CAC scores and clinical characteristics. (A) CAC scores were higher in patients with MACEs than patients who did not experience MACEs; (B) CAC scores were significantly higher in patients with triple-vessel disease than in patients with single- and dual-vessel disease; (C,D) significantly higher CAC scores were observed in patients with higher than median ages and Cr levels. CAC, coronary artery calcification; MACE, major adverse cardiac event; Cr, creatinine.
Medication and PCI plus medical therapy
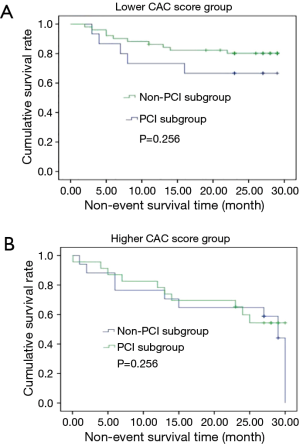
Of all patients, only 32 patients accepted PCI, whereas the remaining patients under went optimal medical therapy. In both groups, the patients were divided into the PCI sub-group (n=15 for patients with lower CAC scores and n=17 for patients with higher CAC scores), which included patients who underwent PCI plus medical therapy, and the non-PCI sub-group (n=51 for patients with lower CAC scores and n=23 for patients with higher CAC scores), which included patients who only received optimal medical therapy. Table 2 shows that the medical therapy was similar in both groups and that the percentages of PCI and multi-vessel disease were higher in the higher CAC score group than the lower CAC score group. Furthermore, a Kaplan-Meier analysis suggested that the rates of MACE did not differ by treatment strategy in both the high CAC score and low CAC score groups (Figure 2A,B).
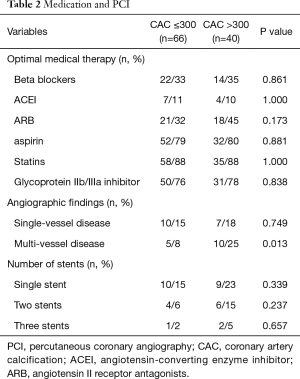
Full table
Relationship between risk factor and MACE
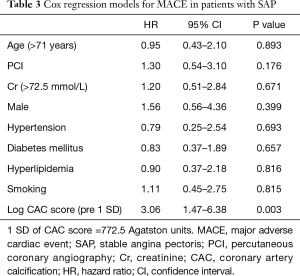
A total of 35 patients suffered a MACE after a median of 24.50 months (range, 0.07–30.00 months) of follow-up (Table 2). A Kaplan-Meier analysis suggested that a strong association between higher CAC scores and MACE in patients with SAP (P=0.033) (Figure 3). Moreover, a Cox regression analysis adjusted for clinical characteristics showed that high CAC scores adversely affected the survival of patients with SAP [hazard ratio (HR), 3.06; 95% confidence interval (CI), 1.47–6.38; P=0.003] (Table 3).

Full table
Discussion
In this study, we investigated the relationship between the CAC scores and the clinical characteristics and prognosis of patients with SAP. We found the following: (I) that there was a positive association between CAC scores and age, Cr; (II) that compared with patients with lower CAC scores, the rates of PCI plus medical therapy, MACE and multi-vessel disease were significantly higher in patients with higher CAC scores; (III) that a Kaplan-Meier analysis suggested that there was no difference in the rates of MACE with treatment strategy of PCI plus medical therapy compared with optimal medical therapy alone, regardless of higher or lower CAC scores; and (IV) that the Kaplan-Meier and Cox regression analyses showed that the CAC scores were risk factors for non-event survival time (HR, 3.06; 95% CI, 1.47–6.38; P=0.003).
Previous studies have shown that CAC scores are closely related to the progression of coronary atherosclerotic plaques and that they independently predicted CAD events and all-cause mortality because they may increase the likelihood of plaque rupture (12-14). Our study, which showed that the rate of MACE in patients with SAP directly correlated with the CAC score, corroborated these previous findings. Further, we identified a positive relationship between the CAC scores and age, the Cr level, and atherosclerotic lesions, similar to the findings from recent studies (7,14). Many researchers have reported that the CAC scores are reported to increase with age. A significantly higher Cr in higher CAC score may be related to dysregulated calcium and phosphorus metabolism and the deposition of high phosphorus levels in the blood vessel wall after renal dysfunction. High serum phosphorus levels can promote the transformation of vascular smooth muscle cells into osteoblasts to increase bone calcium mobilization. Consequently, intercellular and intracellular calcium concentrations are increased, resulting in calcium phosphorus deposition in the atherosclerotic plaque and arterial muscle layer, which promotes CAC (15). Moreover, coronary angiography results from 32 patients showed that the rate of multi-vessel disease directly correlated with the CAC score, whereas single-vessel disease did not correlate with the CAC score.
Several large population registries and clinical trials confirming the role of CAC scores in the detection of risk among intermediate Framingham risk patients have been published (9,16-18). Calcium deposits indicate the existence of atherosclerotic lesions, and in general, the more severe the calcium deposition is, the more extensive the atherosclerotic lesions are. Traditionally, CAC is considered an unfavourable phenomenon because it relates to disease severity and adverse prognosis, but several clinical and biomechanical studies have indicated that calcium deposits tend to reduce the likelihood of plaque rupture, indicating that CAC is favourable for prognosis (3). Shah and his colleagues found that the extent of CAC is an independent estimator of long-term prognosis among symptomatic patients with luminal stenosis and that the extent may further define risk and guide preventative strategies in patients without obstructive CAD (19). This study identified a direct correlation between the CAC scores and MACE, particularly the rate of rehospitalisation for cardiac ischaemic events. Moreover, a Kaplan-Meier analysis suggested that MACE were more common in patients with higher CAC scores than in patients with lower CAC scores, and a Cox regression analysis showed that the CAC score (per-SD) was a risk factor for the non-event survival time (HR =3.06). Thus, we are more inclined to support CAC as an indicator of poor prognosis. Accordingly, patients with SAP and high CAC scores should receive additional treatment interventions to improve their prognosis.
In this study, the 17 patients with high CAC scores received a more positive treatment for therapy plus PCI, but we did not find a relationship between the different treatments (medicine therapy and medicine therapy plus PCI) and MACE, regardless of a lower or higher CAC score in patients with SAP. The COURAGE clinical trial also did not identify a difference in survival between patients with SAP initially treated with PCI plus medical therapy or medical therapy alone during an extended follow-up (20). Even among high-risk subgroups of patients, no subgroup that derived a survival benefit could be identified.
Generally, PCI is more difficult for patients with CAC stenosis. Specifically, the balloon and stent may not permit sufficient expansion and complete apposition, but balloon dilatation or stent implantation may increase the risk of calcified plaque rupture, which may stimulate the formation of thrombosis or endothelial cells and, consequently, cause the blood vessel to narrow quickly again (21). Therefore, the optimization of the PCI strategy is very important to avoid unnecessary PCI, especially for calcified lesions. FFR (fractional flow reserve) is the gold standard for evaluating the risk of myocardial ischaemic due to a coronary artery plaque, and it is helpful to make decisions regarding SAP treatment. In patients with multi-vessel disease, the SYNTAX score provides a basis for revascularization (22,23).
This study has several limitations. It is a single-centre study with a relatively small number of enrolled patients; therefore, patient selection bias could not be completely avoided in our study. Furthermore, some patients in this study were followed for several months. Further studies with larger sample sizes and long-term follow-up are needed to rigorously evaluate the prognostic value of the CAC score for patients with SAP.
In conclusion, our study demonstrated that a higher CAC score (>300) is associated with a higher rate of MACE and that the CAC score (per SD) was significantly associated with clinical events in patients with SAP.
Acknowledgements
Funding: This study was financed by Clinical technology Foundation of Jiangsu Province (BL2012042).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee of Wuxi No. 2 Hospital and written informed consent was obtained from all patients.
References
- Hecht HS. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging 2015;8:579-96. [Crossref] [PubMed]
- Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827-32. [Crossref] [PubMed]
- Peix A, Batista E, Cabrera LO, et al. Gated-SPECT myocardial perfusion imaging and coronary calcium score for evaluation of patients with acute chest pain and a normal or nondiagnostic electrocardiogram. Coron Artery Dis 2012;23:438-44. [Crossref] [PubMed]
- Yoon YE, Chang SA, Choi SI, et al. The absence of coronary artery calcification does not rule out the presence of significant coronary artery disease in Asian patients with acute chest pain. Int J Cardiovasc Imaging 2012;28:389-98. [Crossref] [PubMed]
- Mosseri M, Satler LF, Pichard AD, et al. Impact of vessel calcification on outcomes after coronary stenting. Cardiovasc Revasc Med 2005;6:147-53. [Crossref] [PubMed]
- Gosselin G, Teo KK, Tanguay JF, et al. Effectiveness of percutaneous coronary intervention in patients with silent myocardial ischemia (post hoc analysis of the COURAGE trial). Am J Cardiol 2012;109:954-9. [Crossref] [PubMed]
- Wang FF, Han JL, He R, et al. Prognostic value of coronary artery calcium score in patients with stable angina pectoris after percutaneous coronary intervention. J Geriatr Cardiol 2014;11:113-9. [PubMed]
- Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [Crossref] [PubMed]
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336-45. [Crossref] [PubMed]
- Shaw LJ, Raggi P, Callister TQ, et al. Prognostic value of coronary artery calcium screening in asymptomatic smokers and non-smokers. Eur Heart J 2006;27:968-75. [Crossref] [PubMed]
- Sala V, Bergerone S, Gatti S, et al. MicroRNAs in myocardial ischemia: identifying new targets and tools for treating heart disease. New frontiers for miR-medicine. Cell Mol Life Sci 2014;71:1439-52. [Crossref] [PubMed]
- Motoyama S, Sarai M, Narula J, et al. Coronary CT angiography and high-risk plaque morphology. Cardiovasc Interv Ther 2013;28:1-8. [Crossref] [PubMed]
- Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007;49:1860-70. [Crossref] [PubMed]
- Al Rifai M, McEvoy JW, Nasir K, et al. Traditional cardiovascular disease risk factors associated with one-year all-cause mortality among those with coronary artery calcium scores >/=400. Atherosclerosis 2015;241:495-7. [Crossref] [PubMed]
- Liabeuf S, Desjardius L, Momar D, et al. The addition of vascular calcification scores to traditional risk factors improves cardiovascular risk assessment in patients with chronic kidney disease. PLoS One 2015;10:e0131707. [Crossref] [PubMed]
- Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol 2011;57:1622-32. [Crossref] [PubMed]
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010;122:e584-636. [Crossref] [PubMed]
- Erbel R, Mohlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010;56:1397-406. [Crossref] [PubMed]
- Shah S, Bellam N, Leipsic J, et al. Prognostic significance of calcified plaque among symptomatic patients with nonobstructive coronary artery disease. J Nucl Cardiol 2014;21:453-66. [Crossref] [PubMed]
- Sedlis SP, Hartigan PM, Teo KK, et al. Effect of PCI on Long-Term Survival in Patients with Stable Ischemic Heart Disease. N Engl J Med 2015;373:1937-46. [Crossref] [PubMed]
- Généreux P, Madhavan MV, Mintz GS, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) and ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) TRIALS. J Am Coll Cardiol 2014;63:1845-54. [Crossref] [PubMed]
- Task Force Members. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [Crossref] [PubMed]
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014;64:1929-49. [Crossref] [PubMed]


