Application of bronchoscope for the placement of nasoenteric feeding tube in patients with esophagectomy: a novel technique
Introduction
Enteral nutrition is indicated for patients who are unable to take foods orally and have normal intestinal function (1,2), like those with esophagectomy complicated by anastomotic leakage or gastroparesis. It provides essential energy support as parenteral nutrition while maintains the functional intestinal barrier as well. In addition, it also contributes to a significant reduction of infection incidence and organ failure rate, as well as shortened hospital stay, and reduced medical costs (3,4).
The most common method of enteral nutrition is placing the nasoenteric feeding tube (NET) to duodenum or beyond the ligament of Treitz into the proximal jejunum. It is more reliable than intragastric feedings in critically ill patients (5,6), especially in those with anastomotic leakage and gastroparesis. This very method can reduce regurgitation, stimulate the anastomosis, and speed up the anastomotic inflammation repair, though some data are insufficient to show a significant decrease in aspiration or pneumonia with small-bowel feeds (7,8).
There are various approaches of NET placement, including blind passage, fluoroscopically assisted, endoscopic, ultrasound assisted, and electromagnetic assisted procedures or direct surgical guidance (9). However, to date, the clinicians are not satisfied with above methods (10). Though utilizing trans-nasal gastroscopy is the most popular method (11), which is considered to be more tolerable and quicker than others, a lot of local hospitals in China don’t have this endoscopic device.
Bronchoscope has most of the advantages of transnasal endoscopy, and is more popular in common hospitals, which make it useful for NET placement. The aim of this study was to evaluate the feasibility and availability of the technique of placing NET through the bronchoscope in patients with esophagectomy.
Methods
Patients
From January 2013 to January 2016, 48 consecutive patients placed with NET using bronchoscope in Henan Cancer hospital were included in our review. Informed consents were obtained from patients or their family members. The study was approved by the Ethics Committee of Affiliated Cancer Hospital of Zhengzhou University (No. 2016103). All subjects were ≥18 years of age. Clinical informations such as age, gender, and background disease were collected. The success rate, procedure duration, and complications were recorded for each patient.
Technique for placement
All endoscopic procedures and tube placement were performed by experienced endoscopists and assisted by experienced nurses. A 130-cm long polyurethane naso-enteral feeding tube with a front-end opening (Flocare, Nutricia, Netherlands) was used in each case. Patients were fasting for 8 hours before the procedure. Topical Xylocaine was sprayed into the nose and retro-pharynx in conscious patients. One tip of the oxygen tube which was cut into wedges was inserted in the biopsy channel served as air supply device, the other end was connected with 1 mL/min oxygen flow approximately (Figure 1). The tip of the bronchoscope with an outer diameter of 4.9 mm (Olympus BP-260) was then passed under direct vision into one of the nasal passages as far as possible. Usually the endoscope can arrive at the second portion of the duodenum. After removing the oxygen tube, a 260-cm long guide wire with a soft tip (zebra guide-wire, JHY-GW-88-260-C1, Changzhou, China) was inserted via the biopsy forcep channel as far as possible until resistance was felt. Then the endoscope was slowly withdrawn while the wire was simultaneously threaded forward at the same speed, so that the wire can stay in a fixed position in the intestine. Before exiting the stomach, the path made by the wire was tested and adjusted to ensure that there was no coils or loops within the gastric body. After an open-ended feeding tube which was lubricated and filled with water passed over the guide wire into the duodenum or jejunum, the wire was removed. Saline solution instillation is used to rinse the lens to keep the visual field clear, as far as possible avoiding suction so as not to block the slender suction channel.

Assessment
For most of the procedures, if the tube was placed smoothly, and there was no resistance when injecting saline into the tube, the procedure was considered as successful. Meanwhile, air injection with auscultation (12) and the aspiration of bile were applied to confirm whether the feeding tubes were located well in small bowels. In order to reduce the patient’s discomfort, only when necessary, the bronchoscope though the adjacent naris was reintroduced into the proximal stomach to check whether the tube remained straight along and through the pylorus.
Follow-up
The assessment methods of the procedures were subjective, for confirming whether the placement is successful or not, all patients had clinical follow-up daily for one week after the procedure. The most concerning point was whether the food can be injected through tube smoothly. For patients with gastric decompression, the decompression tube was also checked for food remains to make sure that the NET was placed deep enough.
Results
Patient characteristics (Table 1)
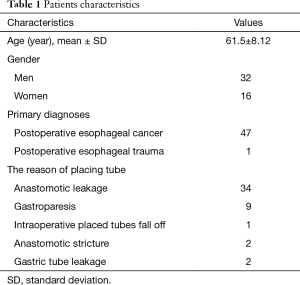
Full table
Among these 48 patients, 32 were male and 16 were female. The mean age was 61.5 years (range, 28–77 years). Primary diagnoses were postoperative esophageal cancer (47/48), postoperative esophageal trauma (1/48), of which 34 had anastomotic leakage, 9 had gastroparesis, 1 had the intraoperative placed nutritional tube fall off, 2 had anastomotic stricture as cancer recurrent, and 2 had gastric tube leakage.
Patient outcomes
NET was successfully placed in all (the technique success rate was 100%) patients. 93.8% (45/48) of the procedures were performed at the endoscopic center, 6.3% (3/48) were beside using the fiber-bronchoscope (Olympus BP-P60) for the placement. During the follow-up of 7 days, the tube feeding for all patients went well, no foods were found in the gastric decompression tubes. There were no adverse events related to the tube placement, such as epistaxis or perforation. The average time for placement was 257 s (range, 150–750 s).
Discussion
How to place the NET quickly, safely and patient-friendly remains an important technique for doctors. There are various approaches to NET placement. However, to date, the clinicians were not satisfied with those methods for some reasons as indicated below.
Blind insertion is the original and most simple technique for nasoenteral intubation. Although serious attention was paid on right lateral positioning, gastric insufflation, tube tip angulation, and clockwise rotation during insertion, the success rate was still low while complications occurred frequently. A study by de Aguilar-Nascimento and Kudsk (13) demonstrated that of 932 blind postpyloric tube placement attempts, 433 (46%) failed and 20 (1.6%) were airway misplacements. In addition, such tube placements require experience and an average of 28–40 min to perform (12). It is not suitable for patients with gastric emptying disorder or anatomical changes, so it is not widely accepted.
Failure of bedside NET placement is an indication for the use of fluoroscopy or endoscope. Many studies reported that fluoroscopic guidance in the placement of Naso-intestinal feeding tubes had a success rate of >84% (14,15), achieving jejunal positioning in 53%, requires on average 22 min of fluoroscopy room time (16). However, this procedure is not only expensive, but also exposes patients and doctors to varying doses of radiation.
Endoscopically assisted intubation allows direct vision and is, therefore, a more practical approach. Depending on experience, the success rate of endoscopic NET placement has been described to range from 86% to 97% (9). There are two methods in using of traditional transoral gastroscope: one is directly pulling-pushing, which makes the gastroenterologists frustrated in their efforts because of retrograde migration on withdrawal of the endoscope. Another is by guide wire which takes much less time than the above. But both of the procedures have to change the tube from mouth to nose in the end, which aggravate the patient’s discomfort and prolong the operation time.
Transnasal gastroscopy with an outer diameter of 5.1–5.9 mm has been developed and used frequently for more than 10 years, which has been reported to be safer and more tolerable than traditional transoral gastroscopy (17,18). Compared with using traditional transoral gastroscope, nasoendoscopical placement method does not have to change the tube from mouth to nose in the end of the procedure, which shows advantage as a more successful technique for tube placement than others (19,20). Qin et al. (11) compared fluoroscopic, endoscopic and guide wire assistance with ultraslim gastroscopy for placement of nasojejunal feeding tubes. The success rate for guide wire assistance with transnasal gastroscopic placement was 100%, the average time was 11.1±2.2 min. It was significantly faster (P<0.05) than any other approaches. It was also feasible in patients with upper gastrointestinal diseases, especially in those with changed anatomy (21). But 2–5% of patients may present epistaxis after transnasal gastroscopic placement (22,23). However, lots of hospitals don’t have this endoscope system, which limits the promotion of this technology.
Bronchoscope, which is the basic respiratory endoscopic device, not only has most of the advantages of transnasal gastroscopy, but also is available in common hospitals in China. We used oxygen instillation as air supply plant, which broke its application limitation in digestive tract. Alternatively we have applied bronchoscope for NET placement with a satisfying result.
Our average time for successful placement was 257 s is obviously shorter than other methods. The case which had the longest operation time both had anastomotic mediastinal leakage and tracheal leakage, its fistula was as huge as the stomach cavity and covered with too much necrotic material, that made us spend too much time to find the correct direction to the stomach cavity.
For patients in intensive care unit, the fiberbronchoscope was applied because of the feasibility to be carried to perform the procedure at the bedside without the movement of the patient.
The bronchoscope with an outer diameter of 4.9 mm is thinner than transnasal endoscope, no complication of epistaxis has been found in this study. As the experience of these endoscopists with bronchoscopy is ranged from 7 to 20 years, this outcome was acceptable. Meanwhile, all of the patients under local anesthesia tolerated well, and it solved the problem that some of the critically ill patients are not suitable for general anesthesia gastroscopy. The patients with tracheal fistula commonly have severe pneumonia, which indicates high risk for the outpatients to have general anesthesia.
This technology is limited to patients with upper gastrointestinal surgery because the total length of bronchoscope is only 60 cm. Entering into the pylorus is one technical difficulty as most of the opening direction of the pylorus had changed by the operation, which was also the main issue affecting entry speed. Another point is that the bronchoscope is a two-way endoscope, which is different from the four-way gastroscope, so that the digestive endoscopic physicians need time to adapt to it.
In conclusion, our experience showed that the technique of placing NET with the bronchoscope is quick, effective, safe and tolerable for patients with esophagectomy, which is also suitable for patients in intensive care unit.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of Affiliated Cancer Hospital of Zhengzhou University (No. 2016103). Written informed consent was obtained from the patients or their family members for publication of this manuscript and any accompanying images.
References
- Phillips MS, Ponsky JL. Overview of enteral and parenteral feeding access techniques: principles and practice. Surg Clin North Am 2011;91:897-911. ix. [Crossref] [PubMed]
- DeWitt RC, Kudsk KA. Enteral nutrition. Gastroenterol Clin North Am 1998;27:371-86. [Crossref] [PubMed]
- McClave SA, Chang WK, Dhaliwal R, et al. Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral Nutr 2006;30:143-56. [Crossref] [PubMed]
- Eckerwall GE, Axelsson JB, Andersson RG. Early nasogastric feeding in predicted severe acute pancreatitis: A clinical, randomized study. Ann Surg 2006;244:959-65; discussion 965-7. [Crossref] [PubMed]
- Davies AR, Froomes PR, French CJ, et al. Randomized comparison of nasojejunal and nasogastric feeding in critically ill patients. Crit Care Med 2002;30:586-90. [Crossref] [PubMed]
- Hsu CW, Sun SF, Lin SL, et al. Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, randomized, clinical study. Crit Care Med 2009;37:1866-72. [Crossref] [PubMed]
- Marik PE, Zaloga GP. Gastric versus post-pyloric feeding: a systematic review. Crit Care 2003;7:R46-51. [Crossref] [PubMed]
- Ho KM, Dobb GJ, Webb SA. A comparison of early gastric and post-pyloric feeding in critically ill patients: a meta-analysis. Intensive Care Med 2006;32:639-49. [Crossref] [PubMed]
- ASGE Technology Committee. Enteral nutrition access devices. Gastrointest Endosc 2010;72:236-48. [Crossref] [PubMed]
- Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol 2014;20:8505-24. [Crossref] [PubMed]
- Qin H, Lu XY, Zhao Q, et al. Evaluation of a new method for placing nasojejunal feeding tubes. World J Gastroenterol 2012;18:5295-9. [PubMed]
- Zaloga GP. Bedside method for placing small bowel feeding tubes in critically ill patients. A prospective study. Chest 1991;100:1643-6. [Crossref] [PubMed]
- de Aguilar-Nascimento JE, Kudsk KA. Clinical costs of feeding tube placement. JPEN J Parenter Enteral Nutr 2007;31:269-73. [Crossref] [PubMed]
- Stănescu D, Mihalache D, Nistor A, et al. Importance of enteral nutrition support in necrotic hemorrhagic pancreatitis. Rev Med Chir Soc Med Nat Iasi 2010;114:91-4. [PubMed]
- Zhihui T, Wenkui Y, Weiqin L, et al. A randomised clinical trial of transnasal endoscopy versus fluoroscopy for the placement of nasojejunal feeding tubes in patients with severe acute pancreatitis. Postgrad Med J 2009;85:59-63. [Crossref] [PubMed]
- Ott DJ, Mattox HE, Gelfand DW, et al. Enteral feeding tubes: placement by using fluoroscopy and endoscopy. AJR Am J Roentgenol 1991;157:769-71. [Crossref] [PubMed]
- Murata A, Akahoshi K, Sumida Y, et al. Prospective randomized trial of transnasal versus peroral endoscopy using an ultrathin videoendoscope in unsedated patients. J Gastroenterol Hepatol 2007;22:482-5. [Crossref] [PubMed]
- Yagi J, Adachi K, Arima N, et al. A prospective randomized comparative study on the safety and tolerability of transnasal esophagogastroduodenoscopy. Endoscopy 2005;37:1226-31. [Crossref] [PubMed]
- Wiegand N, Bauerfeind P, Delco F, et al. Endoscopic position control of nasoenteral feeding tubes by transnasal re-endoscopy: a prospective study in intensive care patients. Am J Gastroenterol 2009;104:1271-6. [Crossref] [PubMed]
- Black H, Yoneda K, Millar J, et al. Endoscopic placement of a novel feeding tube. Chest 2010;137:1028-32. [Crossref] [PubMed]
- Zhang L, Huang YH, Yao W, et al. Transnasal esophagogastroduodenoscopy for placement of nasoenteric feeding tubes in patients with severe upper gastrointestinal diseases. J Dig Dis 2012;13:310-5. [Crossref] [PubMed]
- Damore LJ 2nd, Andrus CH, Herrmann VM, et al. Prospective evaluation of a new through-the-scope nasoduodenal enteral feeding tube. Surg Endosc 1997;11:460-3. [Crossref] [PubMed]
- Patrick PG, Marulendra S, Kirby DF, et al. Endoscopic nasogastric-jejunal feeding tube placement in critically ill patients. Gastrointest Endosc 1997;45:72-6. [Crossref] [PubMed]


