Chondromatous hamartoma of cervical esophagus: a case report and literature review
Introduction
Hamartomas are congenital tumor-like malformations that contain a range of heterogeneous structures (1). Esophageal hamartomas are rare and account for approximately 6% of large resected hypopharyngeal and esophageal polyps (2). Esophageal chondromatous hamartomas, which are histologically composed of nodules of proliferating hyaline cartilage and spindle cells, are very rare (3). Only several studies have reported that esophageal hamartomas were chondromatous or contained cartilaginous (4-9) or bony tissue (10,11). We herein present a very rare case of an elderly women with a chondromatous hamartoma in the cervical esophagus.
A literature review was conducted using the PubMed database (up to August 2016). The search terms “esophageal hamartoma” (71 studies) and “chondromatous hamartoma” (102 studies) were used in the search process. The references in the relevant articles and reviews were also scanned for potentially eligible studies.
Case presentation
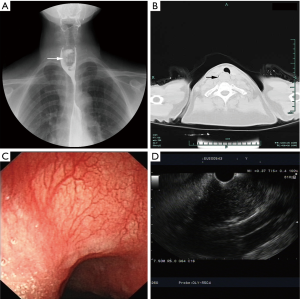
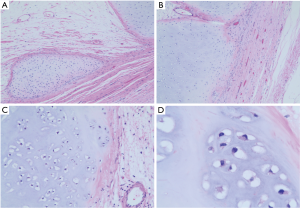
A 64-year-old woman who had a progressive foreign body sensation in the laryngopharynx for 3 years was admitted to our department. She denied dysphagia, nausea and vomiting, anorexia, weight loss, belching and acid reflux, chest pain, and hemoptysis. The patient had a history of hypertension, and she was receiving antihypertensive treatment. An echocardiogram indicated mild regurgitation in the aortic, mitral, and tricuspid valves, left ventricular diastolic dysfunction, and arrhythmia. Tumor markers and other blood tests showed no abnormalities. The patient had no other significant medical background or family history. A barium test revealed a stricture in the upper esophagus for approximately 2.5 vertebral bodies (Figure 1A). Computed tomography (CT) and enhanced CT scans suggested a 2.5-cm soft-tissue mass in the upper esophagus with inhomogeneous mild enhancement and no obvious lymph node enlargement (Figure 1B). The patient underwent endoscopic ultrasonography (EUS), which revealed a giant bulging lesions in the upper esophagus with smooth surface mucosa. The lesion presented with inhomogeneous low-echo areas and multiple high-echo points (Figure 1C,D). EUS-guided fine-needle aspiration (EUS-FNA) was conducted and the pathology report suggested that the lesion consisted of small pieces of cartilaginous tissue. The multidisciplinary team (MDT) devised a further treatment plan, and the patient underwent trans-cervical esophagectomy after comprehensive evaluation (Figure 2A). The patient was placed in a supine position, and general endotracheal anesthesia was induced without complications. The neck was then prepared and draped in the usual sterile fashion. A 15-cm U-shaped incision was made, and the platysma was incised to free the upper esophagus. A longitudinal myotomy was performed, and an intraluminal hard mass was exposed without breaking through the mucosa. A 4.5 cm × 2 cm × 2 cm intraluminal pedicled mass was resected (Figure 2B). The incision was sutured layer by layer with 4-0 non-invasive sutures and a negative-pressure drainage ball was placed. An intraoperative biopsy revealed it a cervical esophageal chondromatous hamartoma composed of cartilage cells (Figure 3). The patient was stable after surgery, had no obvious complications and was discharged 12 days later. She was regularly followed up for 4 months and had no recurrence of the foreign body sensation.

Discussion
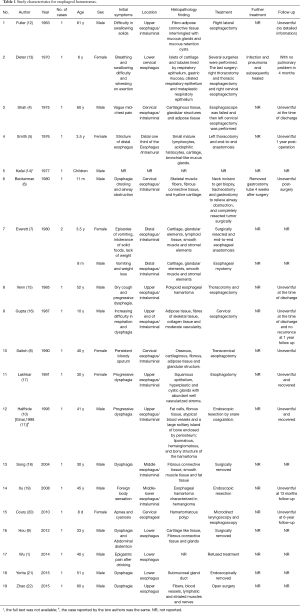
Esophageal hamartoma, which was first described in 1963, is rare (12). To the best of our knowledge, twenty studies with twenty esophageal hamartoma cases (1,4-22) have been reported and eight of these studies described nine cases (4-11) of esophageal chondromatous hamartomas or that contained cartilaginous or bony tissue. Four cases (4,6,8,10,11) were cervical or upper esophagus hamartomas [Halfhide et al. (10) and Ginai et al. (11) reported the same case], and five cases (5,7,9,13) were in distal or lower esophagus [one (9) was in Chinese, Table 1]. Several other studies (23-32) also reported congenital esophageal stenosis caused by tracheobronchial remnants. Generally, most chondromatous hamartomas are located in the lung parenchyma (33), and although this type of tumor is very rare in the esophagus, it is the most common benign lung tumor and third most common pulmonary nodule (34). Esophageal chondromatous hamartomas are very rare in terms of both their anatomical location and their pathological components. In this case, the clinical manifestation and auxiliary examination were not specific, and EUS-FNA played an important role in preoperative diagnosis of the hamartoma. Xu et al. (19) reported that EUS was superior to other imaging techniques, including barium esophagogram, contrast-enhanced CT image and conventional gastroscopy, in the diagnosis and treatment of hamartoma. Indeed, EUS can provide helpful diagnostic accuracy and comprehensive pre-operative assessment of submucosal tumors of the esophagus, including more detailed information about the tumor size, layer of origin, morphologic features, and even histopathological components (35). Thus, clinicians could design further treatment plans for patients with submucosal tumors of esophagus based on the EUS-FNA results.
Full table
The distinctive histologic feature of a chondromatous hamartoma is the hyaline cartilage, which is located in cartilage lacunae and surrounded by a thin fibrous perichondrium. However, highly differentiated chondrosarcoma, which featured with lobulated tumor cells with less atypia, should be taken in to consideration for different diagnosis. In our case study, the mass was covered with an integrated capsule and was composed of cartilage cells that were well differentiated, and our hospital’s pathology team had taken chondromatous hamartoma into prior consideration.
There are no standard treatment instructions for esophageal hamartoma. Most of the previously reported patients underwent surgical treatment, including esophagectomy and thoracotomy, while one underwent endoscopic resection by snare coagulation (10), two underwent routine endoscopic resection (19,20) and one refused operation (1). Ginai et al. (11) suggested that the resection method depends on the polyp’s volume and site of origin. When the pedicle is thin and the polyp is relatively small, endoscopic ligation is preferred. If there is an increased risk of bleeding, cervical esophagectomy should be performed. However, Xu et al. (19) suggested that gastroscopic resection is more feasible and the selection of different treatment methods should be based on the depth of tumor invasion. In our case, the patient was carefully evaluated and transferred to our department from the department of gastroenterology, and it was discussed during the MDT consultation before surgery that the tumor might have malignant potential. For conservative considerations and to avoid perforation and bleeding from an endoscopic resection, we performed transcervical esophagectomy. According to the limited report information, no further post-surgical treatment was given for these esophageal hamartoma cases, and all patients were discharged uneventfully and recovered with no recurrence.
Hamartomas are uncommon congenital abnormalities that are usually asymptomatic and grow slowly. In this case, the patient complained of a progressive foreign-body sensation in the laryngopharynx for 3 years. However, it can be speculated that the hamartoma might have existed for many years and grown slowly until it was large enough to cause symptoms. Previous studies suggested that esophageal hamartoma was benign, however, obstruction and pulmonary complications can cause fatal events. Thus, aggressive surgical treatment should be recommended because it can significantly improve the patients’ status and is nearly curative (5).
In conclusion, we report a very rare chondromatous hamartoma of the cervical esophagus. Pre-operative EUS-FNA can aid in diagnosis and surgical treatment should be recommended for cervical esophageal hamartomas.
Acknowledgements
Funding: This work was funded by Major science and technology projects of Zhejiang province (2014C03032) and General research program of medical and health in Zhejiang Province (2015KYB142).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Wu WM, Wang XD, Sun G, et al. Adult asymptomatic hamartoma in the distal esophagus: a rare case. Intern Med 2014;53:1945-8. [Crossref] [PubMed]
- Caceres M, Steeb G, Wilks SM, et al. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg 2006;81:393-6. Review. [Crossref] [PubMed]
- Amstalden EM, Carvalho RB, Pacheco EM, et al. Chondromatous hamartoma of the chest wall: description of 3 new cases and literature review. Int J Surg Pathol 2006;14:119-26. [Crossref] [PubMed]
- Shah B, Unger L, Heimlich HJ. Hamartomatous polyp of the esophagus. Arch Surg 1975;110:326-8. [Crossref] [PubMed]
- Smith CW, Murray GF, Wilcox BR. Intramural esophageal hamartoma. An unusual cause of progressive stricture in a child. J Thorac Cardiovasc Surg 1976;72:315-8. [PubMed]
- Beckerman RC, Taussig LM, Froede RC, et al. Fibromuscular hamartoma of the esophagus in an infant. Am J Dis Child 1980;134:153-5. [PubMed]
- Everett C, Volberg F, Ulshen M, et al. Intramural esophageal hamartoma: a report of two cases and review of the literature. Gastrointest Radiol 1980;5:317-9. [Crossref] [PubMed]
- Saitoh Y, Inomata Y, Tadaki N, et al. Pedunculated intraluminal osteochrondromatous hamartoma of the esophagus. J Otolaryngol 1990;19:339-42. [PubMed]
- Hou SP, Zhang QQ, Wang LN, et al. Chondroma-like hamartoma of esophagus: report of a case. Zhonghua Bing Li Xue Za Zhi 2012;41:274-5. [PubMed]
- Halfhide BC, Ginai AZ, Spoelstra HA, et al. Case report: a hamartoma presenting as a giant oesophageal polyp. Br J Radiol 1995;68:85-8. [Crossref] [PubMed]
- Ginai AZ, Halfhide BC, Dees J, et al. Giant esophageal polyp: a clinical and radiological entity with variable histology. Eur Radiol 1998;8:264-9. [Crossref] [PubMed]
- Fuller AP. Pedunculated hamartoma of the oesophagus. J Laryngol Otol 1963;77:706-13. [Crossref] [PubMed]
- Dieter RA Jr, Riker WL, Holinger P. Pedunculated esophageal hamartoma in a child. A case report. J Thorac Cardiovasc Surg 1970;59:851-4. [PubMed]
- Kafai F, Mirbod P. Hamartoma of the oesophagus. Br J Clin Pract 1977;31:154-6, 165. [PubMed]
- Venn GE, DaCosta P, Goldstraw P. Giant oesophageal hamartoma. Thorax 1985;40:684-5. [Crossref] [PubMed]
- Gupta AK, Goyal VP, Hemani DD, et al. Pedunculated intraluminal oesophageal hamartoma. J Laryngol Otol 1987;101:851-4. [Crossref] [PubMed]
- Lakhkar BN, Ghosh MK, Shenoy PD, et al. Hamartoma--a benign intraluminal tumor of the oesophagus (a case report). J Postgrad Med 1991;37:235-7, 236A-236B.
- Song X, Wang W, Tong S, et al. Giant hamartoma polyp of esophagus. Chin J Dig 2004;24:744.
- Xu GQ, Hu FL, Chen LH, et al. The value of endoscopic ultrasonography on diagnosis and treatment of esophageal hamartoma. J Zhejiang Univ Sci B 2008;9:662-6. [Crossref] [PubMed]
- Coury J, Steinfeld J, Zwillenberg D, et al. Esophageal hamartoma as an unusual cause of neonatal apnea and bradycardia. Ear Nose Throat J 2010;89:E7-E11. [PubMed]
- Yorita K, Miike T, Sakaguchi K, et al. Corrigendum: A Novel Case of an Unusual Esophageal Submucosal Tumor: An Esophageal Submucosal Gland Duct Hamartoma. Am J Gastroenterol 2015;110:1634. [Crossref] [PubMed]
- Zhao XJ, Xie H, Yu DL, et al. Esophageal stricture caused by a mediastinal hamartoma invading the esophageal wall. Endoscopy 2015;47 Suppl 1 UCTN:E151-2.
- Frey EK, Duschl L. Der Kardiospasmus. Springer Berlin Heidelberg; 1936. Available online: https://link.springer.com/chapter/10.1007/978-3-642-91091-3_12
- Case records of the Massachusetts General Hospital; case 42411. N Engl J Med 1956;255:707-10. [PubMed]
- Kumar R. A case of congenital oesophageal stricture due to a cartilaginous ring. Br J Surg. 1962;49:533-4. [Crossref] [PubMed]
- Paulino F, Roselli A, Aprigliano F. Congenital esophageal stricture due to tracheobraonchial remnants. Surgery 1963;53:547-50. [PubMed]
- Ishida M, Tsuchida Y, Saito S, et al. Congenital esophageal stenosis due to tracheobronchial remnants. J Pediatr Surg 1969;4:339-45. [Crossref] [PubMed]
- Fonkalsrud EW. Esophageal stenosis due to tracheobronchial remnants. Am J Surg 1972;124:101-3. [Crossref] [PubMed]
- Goldman RL, Ban JL. Chondroepithelial choristoma (tracheobronchial rest) of the esophagus associated with esophageal atresia. Report of an unusual case. J Thorac Cardiovasc Surg 1972;63:318-21. [PubMed]
- Deiraniya AK. Congenital oesophageal stenosis due to tracheobronchial remnants. Thorax 1974;29:720-5. [Crossref] [PubMed]
- Ohkawa H, Takahashi H, Hoshino Y, et al. Lower esophageal stenosis in association with tracheobronchial remnants. J Pediatr Surg 1975;10:453-7. [Crossref] [PubMed]
- Rose JS, Kassner EG, Jurgens KH, et al. Congenital oesophageal strictures due to cartilaginous rings. Br J Radiol 1975;48:16-8. [Crossref] [PubMed]
- Gholoum S, Fraser R, Ferri LE. Posterior mediastinal chondromatous hamartoma. Ann Thorac Surg 2007;83:1528-30. [Crossref] [PubMed]
- Seda G, Amundson D, Lin MY. Predominant cartilaginous hamartoma: an unusual variant of chondromatous hamartoma. South Med J 2010;103:169-71. [Crossref] [PubMed]
- He G, Wang J, Chen B, et al. Feasibility of endoscopic submucosal dissection for upper gastrointestinal submucosal tumors treatment and value of endoscopic ultrasonography in pre-operation assess and post-operation follow-up: a prospective study of 224 cases in a single medical center. Surg Endosc 2016;30:4206-13. [Crossref] [PubMed]


