Regional dietary characteristics and bronchial foreign body: a repeated misdiagnosis caused by a red pepper
Case presentation
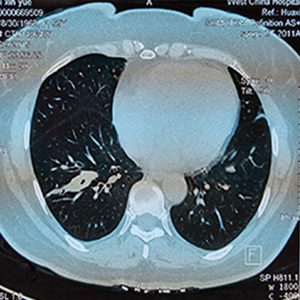
A 52-year-old woman presented to West China Hospital, Sichuan University, China, with a history of recurrent cough and hemosputum for more than 3 years, and aggravated in recent 2 months. Before admission, thoracic CT scan twice and flexible fiberoptic bronchoscopy 5 times all diagnosed as chronic pulmonary inflammation in lower lobe of right lung, besides, the biopsy twice also showed bronchial granulation nodule formation. For further treatments, with the suspicion of lung cancer, VATS resection of lower lobe of right lung was conducted. However, when we checked the resected specimen, a red pepper was belatedly found inserted in the basal segment bronchial. Tumor was excluded by postoperative pathological analysis. After 3 days’ postoperative respiratory managements, she was discharged successfully.
Discussion
Generally, vegetative foreign bodies were the most common foreign body aspirated (84.7%) (1); and most of them can be primarily suspected by a definite history of aspiration, and further confirmed by chest X-ray, CT-scan or bronchoscopy (2). However, in some cases, especially to those with a denied history of aspiration, and no evidence of thoracic CT scan or fiberoptic bronchoscopy, the correct diagnosis is usually challenging (3). The suspected diagnoses are commonly as pulmonary infection, tuberculosis or tumors (4), while bronchial foreign body may be often ignored, which may seriously affect the optimal treatments.
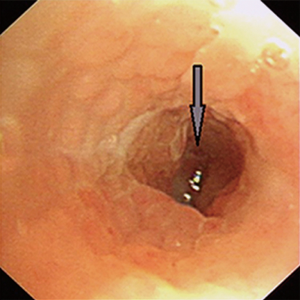
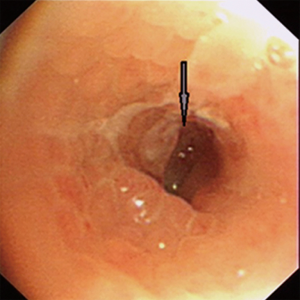
Although aspiration of a foreign body into trachea and bronchus can occur in all age groups, infants and little children suffer most commonly. Most adult patients with a foreign body in the bronchial tree have an early history suggestive of aspiration. As such, occult foreign body aspiration in adults is rare. In our case, the patient couldn’t recall any episode of choking and aspiration, which may partly led to difficulties of diagnosis. As bronchoscopy is the “golden standard” for the definitive diagnosis of an aspirated vegetable foreign body (2) and most aspirated foreign bodies can easily be confirmed by bronchoscopy and biopsy, during bronchoscopy, a foreign body can be directly visualized, or granulation tissue, endobronchial stenosis, or edema, all features of tissue reaction to an aspirated foreign body, may be present. However the initial biopsy did not find satisfying evidences in this case and aspiration of a foreign body was excluded by the bronchoscopy staff once and repeatedly, which finally led to the treatment of lung lobe resection. In Figure 1, the picture of the first time flexible fiberoptic bronchoscopy presented that the basal segment bronchial wall of right lower lobe was red, much similar to blood clot, without bronchial obstruction (as confirmed in Figure 2). Adjacent mucosal swelling and granulation nodule was observed in Figures 2,3 which provided a suspicion of tumors and finally led to a lung resection. But when we dissected the resected specimen, we realized that the bloody area was actually a tubular pepper adhering to the bronchial wall (Figure 4), and could be entirely removed. Postoperative speculation was considered that with the long-term stimulation continuously released from the pepper, adjacent mucosal swelling and granulation nodule were progressively formed and suspected as tumors (Figures 2,3).
Types of bronchial foreign bodies are variegated, depending on patient age and cultural background including religious beliefs as well as alimentary habits or regional dietary characteristics. Ali et al., concluded that Fishermen are more prone to experience a live-fish aspiration while substandard conditions may expose individuals to leech and roundworm infestations (5); Wang et al., reported a rare case of undetected Chinese medicine “coptis chinensis” aspiration for 10 long years, which is an extremely bitter Chinese herbal medicine used as an antipyretic and antibacterial agent since ancient time (6); in a study from Croatia, animal bone and cherry stone aspiration was common due to dietary habits (7). Correct visualization and precise instruments are essential to the success of bronchoscopy, and seasonal correlation factors (8) should also be under consideration. In this case, a well understanding of local diet characteristics should be highly noted that people from southwest china were famous for the dietary habit of spicy food, especially chafing dish, and a high degree of clinical suspicion that red pepper may be a bronchial foreign body though it’s sometimes difficult to identify with blood clot and the tubular characteristic may have little affection on ventilation.
Acknowledgements
Funding: This study was supported by the Foundation of Science and Technology Support Plan, Department of Sichuan Province (2015SZ0158).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Park AH, Tunkel DE, Park E, et al. Management of complicated airway foreign body aspiration using extracorporeal membrane oxygenation (ECMO). Int J Pediatr Otorhinolaryngol 2014;78:2319-21. [Crossref] [PubMed]
- Behera G, Tripathy N, Maru YK, et al. Role of virtual bronchoscopy in children with a vegetable foreign body in the tracheobronchial tree. J Laryngol Otol 2014;128:1078-83. [Crossref] [PubMed]
- Hegde SV, Hui PK, Lee EY. Tracheobronchial foreign bodies in children: imaging assessment. Semin Ultrasound CT MR 2015;36:8-20. [Crossref] [PubMed]
- Kargl S, Frechinger B, Pumberger W. Haemoptysis in a teenager: late diagnosis of unnoticed foreign body aspiration. BMJ Case Rep 2014;2014. doi: 10.1136/bcr-2014-207310. [Crossref]
- Ali SR, Mehta AC. Alive in the Airways: Live Endobronchial Foreign Bodies. Chest 151:481-91. [Crossref] [PubMed]
- Wang L, Pudasaini B, Wang XF. Diagnose of occult bronchial foreign body: A rare case report of undetected Chinese medicine aspiration for 10 long years. Medicine (Baltimore) 2016;95:e4076. [Crossref] [PubMed]
- Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. [Crossref] [PubMed]
- Xiaowei S, Jianji Z, Li Z, et al. Seasonal correlation and causal analysis of the incidence of bronchial foreign bodies in children. Int J Pediatr Otorhinolaryngol 2014;78:1567-70. [Crossref] [PubMed]



