Personalized alternative therapy of intractable bronchiectasis-induced hemoptysis in a patient: syndrome differentiation and treatment according to individual physique category
Case presentation
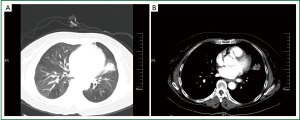
A 53-year-old female presented with recurrent expectoration and hemoptysis over the past forty years and worsening of these symptoms during the past one month or so. The patient reported that her hemoptysis had first appeared at the age of 8 and initially manifested by coughing up small amounts of blood-streaked sputum that could cease on itself. Thereafter, her condition had been relapsing frequently in spring and autumn months, usually induced by common cold, exertion or even an abrupt change in body posture from bending forward to the upright position. She had not been on any regular therapy despite the deteriorating hemoptysis over time. In February 2012, following a seasonal flu, the patient experienced several attacks of productive cough with large quantities of bloody sputum (100-200 mL at each episode). She was consequently hospitalized in a local medical center. A high resolution CT of her chest (10 Feb 2012) revealed multiple lesions of bronchiectasis complicated with infection in both lungs. Patches of infiltrates were seen in the upper (lingula) and lower lobes of the left lung, which was consistent with alveolar hematocele (Figure 1A,B). A fiberoptic bronchoscopy (11 Feb 2012) visually confirmed lesions of bronchiectasis and hemorrhage in the airways of her right upper, left upper and bilateral lower lobes. Since the patient continued to have onsets of significant hemoptysis (50-100 mL) despite conservative medications, she underwent contrast angiography of bronchial arteries and non-bronchial systemic arteries (NBSA) with embolization of disordered vessels. The procedure was uneventful and did improve her symptoms during the rest of hospital stay. However, her condition recurred and even worsened after she was discharged home. She was then referred to our Clinic of Traditional Chinese Medicine (TCM) for alternative therapy, at nearly 3 months after the arterial embolization (11 May 2012).
On first inspection, the patient appeared dull and lethargic with a puffy physique and lusterless facial complexion, showed aversion to wind or cool temperature, and spoke in an upset, worried voice. She reported constipation, sleep disturbances and preference of hot to cold beverages. Her tongue body was pale and fat with whitish wet coatings; her pulses felt deep, long and soft. On routine physical checkup, her temperature was 37.0 degree Celsius, pulse 80 beats/min, respiratory rate 20 times/minute and blood pressure 145/85 mmHg. The contour of her chest was normal with equal expansion and good movement. Breath sounds were attenuated on the left side, and a few moist rales were heard near the bases of both lungs. Her heart percussed normal in size. Cardiac rhythm was regular at 90 per minute. No murmurs. Abdomen was flat and soft. No tenderness, and no palpable masses. Past history unremarkable.
Based on TCM principles of symptom differentiation, the patient was identified to have suffered severe debilitation by substantial deficiency of primordial Qi owing to her long-standing morbidity. Therewith the weakened, stagnated Qi circulation gave rise to retention of body fluid in all meridians and collaterals, particularly, in the pulmonary meridian which is the major regulatory channel of body fluids. In turn, severe fluid retention in the pulmonary meridian impeded the normal return of blood, which was then held back out of the meridian, and may be expelled from the body along with sputum production. Accordingly, alternative treatment for this patient was targeted at warming Yang to induce diuresis, and ultimately, to direct the aberrant blood flow back to the pulmonary meridian. The formula contained 9 commonly used herbs: Radix Aconiti Lateralis Preparata (pre-decocted one hour) 35.7%, Ramulus Cinnamomi 7.9%, Rhizoma Atractylodis Macrocephalae 7.9%, Poria 7.9%, Radix Astragali 15.9%, Radix Angelicae Sinensis 7.9%, Herba Asari 4.8%, baked ginger 7.9% and prepared Radix Glycyrrhiza 4.0%. Decoction of the formula was designed to be taken once daily for a total of 7 days. During the course of herbal treatment, the patient was allowed to continue the medications which she had been using during the past months. Addition of any newly prescribed drugs should be subjected to agreement of the alternative therapist.
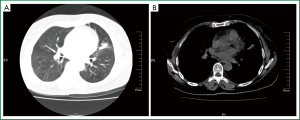
During her second clinic visit on 17 May 2012, the patient reported reduction in her hemoptysis and improvement in the general well-being. The hemoptysis completely resolved after one more course of 7-day herbal therapy with the same formula. Thereafter, the patient was on a 2-month maintenance TCM therapy which targeted at warming Yang, invigorating spleen, and inducing diuresis. As a result, she experienced significant relief in symptoms and better quality of life. Follow-up CT of her chest at two months later (10 July 2012) showed diminishing patchy consolidation in the lingual lobe, and reduced patchy opacities in basal segments of the left lower lung, as compared with pre-treatment (Figure 2A,B). During the treatment course, no newly prescribed drugs were needed.
Discussion
Hemoptysis accounts for about 9-15% of all symptoms in respiratory clinics (1). Among patients presenting with massive hemoptysis, the onset is usually acute and sudden, and associated with asphyxia and hemorrhagic shock that may contribute to a high mortality rate. Bronchiectasis, the most common cause of hemoptysis, is a respiratory disorder characterized by localized, irreversible dilation of part of the bronchial tree caused by destruction of the airway smooth muscles and elastic tissues. Bronchiectasis can develop at any age, but often starts during childhood and becomes symptomatic later in life. The severity and clinical picture of bronchiectasis, as in this case manifested by cough, sputum and hemoptysis, rest largely on the presence and size of complicating infection (2). Although treatment of hemoptysis may include antimicrobials, hemostatics or coagulants, the outcome of conservative therapies appears unsatisfactory, and surgical procedures remain so far the mainstay for management. Unfortunately, a variety of factors, such as the size of lesions and individual physique in a patient, may affect the indication and widespread use of surgical operations. Over the recent years, promising outcomes have been shown by interventional embolization (3-5), but much remains to be evaluated in future studies. Like the patient in this case report, hemoptysis relapsed frequently despite a standard session of interventional embolization.
Personalized alternative treatment according to individual physique category featured the general practice of traditional Chinese medicine. In our case of intractable bronchietasis-induced hemoptysis, the patient showed apparent debilitation and asthenia from her long-standing morbidity that dated back to her childhood. Physically, the patient was dull and lethargic with a puffy body-building and lusterless facial complexion. She showed aversion to wind or cool temperature even on a hot summer day. Coupled with her report about sleep disturbances and preference of hot to cold beverages, her pale and fat tongue body with whitish wet coatings, her deep long and soft pulses, a judgment of physique category as Yang-deficiency in this patient should be proper (6). In a status of Yang deficiency, stagnated Qi circulation in this case subsequently resulted in body fluid retention in the pulmonary meridian. In turn, normal blood return was impeded and held extra-meridianally, mixed with sputum and then coughed up. From the perspective of traditional Chinese medicine, this may explain for the hemoptysis in the patient.
According to the theory of traditional Chinese medicine, in management of hemorrhagic disorders, hemostasis therapy simply may not suffice; rather, the treatment needs to be guided by syndrome differentiation according to the individual physique category. In light of physical characteristics of this patient, central to the treatment was warming Yang and replenishing Qi, which was aimed to induce diuresis and relieve fluid retention. Along with these changes, the system of meridians would finally resume patency. Thereby the aberrant blood flow may be normally directed back to the pulmonary meridian, resulting in cessation of the hemoptysis. The delicate combination of herbs for this patient (Radix Aconiti Lateralis Preparata, Ramulus Cinnamomi, Rhizoma Atractylodis Macrocephalae, Poria, Radix Astragali, Radix Angelicae Sinensis, Herba Asari, baked ginger, and prepared Radix Glycyrrhiza) was shown to well contribute to these goals of treatment. The therapeutic efficacy was encouraging, as reflected by the remarkable resolution of patchy opacities on follow-up CT.
In summary, personalized syndrome differentiation and treatment based on individual physique category can have important implications in alternative therapy for intractable bronchiectasis-induced hemoptysis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Shao XH. eds. Current emergence medicine. Beijing: The Joint Publishing House of Union Medical University and Peking Medical University, 1997:419-21.
- Kutlay H, Cangir AK, Enön S, et al. Surgical treatment in bronchiectasis: analysis of 166 patients. Eur J Cardiothorac Surg 2002;21:634-7. [PubMed]
- Li FB, Yang RM, Zhang MQ, et al. The clinical application of interventional therapy in severe hemoptysis. J Interventional Radiol 2005;14:130-1.
- Yang QH, Lu WF, Xu SC, et al. Treatment of bronchiectasis complicating with acute hemoptysis using transdermal embolisation. J Med Imaging 2002;12:432-34.
- Fan Y, Yin BQ, Han BS, et al. Bronchial arterial embolisation for hemoptysis in patients with pulmonary tuberculosis and bronchiectasis. J Intervent Med 2005;14:582-4.
- Wang Q. eds. Discovery of nine types of physique in Chinese. Beijing: Science Publishing House, 2011:112-6.