A comparison of longitudinal and transverse approaches to ultrasound-guided axillary vein cannulation by experienced operators
Introduction
Central vein cannulation is very important in critical care unit. A variety of situations need central venous access include the need to administer medications and to monitor hemodynamic status. In many cases, such as obesity, thoracic deformity, and emergency status, the landmark method is a challenge and has a high incidence of complications (1,2). In the central line placement with the application of ultrasound, the puncture under direct vision, can significantly reduce complications, including pneumothorax, arterial injury and nerve damage, significantly improve patient safety (3-5). In previous studies, ultrasound method had a superior advantage in the jugular vein and femoral vein cannula compared to the landmark method (6,7). However, each venipuncture method has its own limitations. The internal jugular vein is difficult to insert in patients with tracheotomy. Moreover, due to tracheotomy, patients have a high infection rate. The femoral method is the easiest and most time saving, can be used for emergency rescue. However, due to the anatomical location of the factors, patients are particularly vulnerable to infection (8-10). The subclavian method has many advantages, including ease of care, low infection rate, especially for patients with severe. Because of the clavicle effect, subclavian vein cannot be seen easily, so most operators still use the landmark method. However, landmark method has many drawbacks, including pneumothorax, arterial injury, hematoma (11). The complications of pneumothorax and arterial injury are very common and serious and endanger the lives of patients. Ultrasound-guided cannulation is a novel option to the axillary veins (12). The aim of this study is to find out which transducer orientation, longitudinal or transverse, is better for imaging the axillary vein with ultrasound.
Methods
Clinical materials
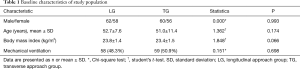
The study was approved by Zhongshan Hospital of Fudan University and written informed consent was obtained from all patients. A total of 236 patients were enrolled in this study between May 2013 and November 2015. All patients were hospitalized in Zhongshan Hospital of Fudan University. Among all the patients, 120 patients were in the longitudinal group and 116 were in the transverse group. The clinical characteristics include gender, age distribution and body mass index were similar between the two groups. The two groups have no significant difference. Baseline characteristics of the research population are presented in Table 1.
Full table
Ultrasound equipment
A ultrasound machine (Philips, CX50) equipped with a high-resolution 7.5-MHz linear array transducer was used. Deep venous catheters package (16 G × 20 cm) are produced by the United States ARROW company. The needle’s diameter is 18 G and length is 6.5 cm. The guide wire’s diameter is 0.8 mm and length is 60 cm.
Real-time ultrasound to guide vein cannulation
Real-time ultrasound guidance allows the needle to be seen during puncture of the vessel and wire passage. It can decrease the complications and increase the success of cannulation by experienced operators. Real-time ultrasound guidance of axillary vein insertion includes several crucial steps (Figure 1).
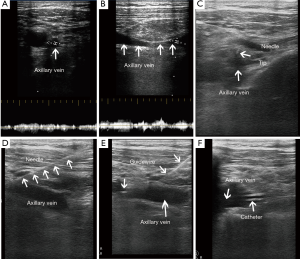
- Apply ultrasound gel to the head of the probe. Place the probe into the sterile covering or sleeve. Apply additional sterile conductive medium between the wrapped probe and the surface of the skin. First, we should find the view of axillary vein, axillary artery, subclavian vein, first rib and adjacent structures. In anatomic terms, the axillary vein is formed from the basilic and the brachial veins continues medially until it reaches the first rib when it becomes the subclavian vein. Scanning of the axillary vessels including artery and vein. Second, we should identify the axillary vein and artery using compression method or pulse-waved Doppler method.
- Center the target vein on the ultrasound screen (transverse view), or obtain a longitudinal view using care to distinguish veins from arteries. Anesthetize the puncture site (e.g., 1% lidocaine). Ultrasound guidance during local anesthesia administration helps prevent inadvertent puncture of the artery or vein, or excessive administration that might distort the anatomy.
- Visualization of the axillary artery to exclude the presence of the needle over the axillary artery. Puncture the vein under the real-time ultrasound guidance using the longitudinal view or the transverse view. When you use the transverse view and visualization of the needle tip is difficult, can make the needle jiggled up and down within the tissues. You should maintain negative pressure on the syringe, push the needle slowly toward the vein until a free flow of blood return occurs. When the tip of the needle cannot be seen, you can measure the depth of the vessel on the ultrasound monitor. This method help you guide the depth of needle and decrease the complications. The needle can be seen to penetrate the vein when you use the longitudinal method (Figure 2).
- Once the vein has been accessed, remove the transducer and place the catheter using Seldinger techniques. Insertion of the guidewire with confirmation of the presence of the guidewire in the axillary vein.
- Exclusion of the presence of the guide wire in the artery and in the jugular vein. Insertion of the catheter into the axillary vein. Confirmation of the presence of the catheter in the axillary vein. Exclusion of the presence of the inserted catheter in the jugular vein.

Statistical analysis
Statistical analysis was performed using SPSS software, version 20.0 (SPSS Inc., Chicago, IL, USA). Data were expressed as mean ± standard deviation (SD). Student’s t-test for independent means, χ2 analysis, or Fisher’s exact test where appropriate were used to evaluate association among the different variables. A P value (two sided in all tests) of <0.05 was considered significant.
Results
Clinical characteristics
A total of 236 patients were enrolled in this study between May 2013 and November 2015. Baseline characteristics of the study population are presented in Table 1. There were no significant differences in age, gender, body mass index (BMI), and mechanical ventilation rate between longitudinal group and the transverse group.
The overall success rates of the longitudinal group and the transverse group were both 100%. No vein punctures failed in 236 patients by experienced operators. The rate of one-attempt success in the longitudinal approach group is higher than the transverse approach group (91.7% vs. 82.8%, P=0.040). The transverse approach group had shorter operation time than the longitudinal group (184.7±8.1 vs. 287.5±19.6 seconds, P=0.000). The two groups had lower postoperative complications. Arterial puncture occurred in 1 of 120 longitudinal and 2 of 116 transverse attempts and this difference was no significant (P=0.541). Two patients who had artery injury were obese to see the axillary artery and vein under ultrasound guidance. One patient got artery injury because of thoracic deformity. Moreover, the axillary artery and vein were very narrow and crossed together. No pneumothorax occurred in the two groups. The results of comparison of longitudinal and transverse approaches are presented in Table 2.

Full table
Discussion
In this study, the proportion with one-attempt success was higher with the longitudinal method than with the transverse approach. The transverse approach was associated with fewer operation time. The longitudinal method had a lower incidence of arterial puncture compared with the transverse method. However, the difference is no significance. For experienced operators, the overall success of axillary vein cannulation is high. The two groups had no failure in overall insertion of catheter under ultrasound guidance. Placement of catheter with direct observation via ultrasound imaging is very safe. The complication of artery puncture was very low in the two groups. No pneumothorax occurred in the longitudinal group and the transverse group. Most of results are in agreement with a previous study.
Over the past years, ultrasound guidance for central venous catheter has evolved from use of Doppler ultrasound alone to use of high frequency linear transducers (3,13,14). The high frequency linear transducers have detailed visualization of vessels. The internal jugular vein and common carotid artery can be easily recognized confirmed with the ultrasound (6). Previous studies have demonstrated that use of real-time ultrasound guidance for central venous catheter insertion can increase success rates and decrease mechanical complications (9,11,15-18). Use of real-time ultrasound guidance for cannulation of central venous catheters has become the standard of care and is recommended by many guidelines. Use of real-time ultrasound guidance for central venous catheter insertion is now routine in our department.
In some studies, ultrasound method had a superior advantage in the jugular vein and femoral vein cannula (10,19). Because of the presence of overlying bony structures, CVC insertions preclude use of ultrasound at the subclavian vein (20). Recent research has turned its attention to real-time ultrasound guidance for the subclavian vein cannulation again (14). In fact, it is technically referring to ultrasound-guided axillary vein access because the venous insertion site is lateral to the first rib. The jugular vein is unavailable in a number of clinical scenarios such as in patients with neck infections, masses, burns, or trauma. The femoral vein method has higher rate of infection. The axillary vein is a good alternative to the jugular vein and femoral vein (8). It yielded the lowest infection rate and could be cared easily. Axillary vein can be well visualized using ultrasound at the lateral position on the chest wall.
Ultrasound guidance of axillary vein cannulation is now documented in the medical literature although many clinicians remain unaware that ultrasound can be integrated into this approach (4,5,12,14,21). Several studies document utility of ultrasound guidance for axillary vein cannulation with a decreased complication rate. Despite the development in the ultrasound guidance of axillary vein cannulation, most of the guidelines do not recommend the axillary method as routine (3,22). A larger study is required to assess the potential of this technique.
In one previous study, a longitudinal orientation of the ultrasound probe was superior to the transverse orientation for visualizing the axially vein (23). All of the results trended in favor of the longitudinal approach. The longitudinal approach was superior in terms of successful placement on the first try without redirection of the needle. The study is the comparison of longitudinal and transverse approaches to ultrasound-guided axillary vein cannulation by the use of a phantom. Although the phantom is similar to the body, there are differences between the model and the human body. These results were obtained from the inexperienced operators. No study evaluating the preferred approach to the ultrasound-guided axillary vein cannulation by experienced operators in patients was found in our literature review. The aim of our study was to identify which method, longitudinal or transverse, is better for imaging the axillary vein with ultrasound.
Subclavian vein cannulation is associated with failure and complications because of injury to the nearby lung and artery (4,16,17,21). Its position, the clavicle and the first rib makes sonographic imaging difficult. The anatomy of subclavian vein makes it difficult to align the needle as well as image the entire needle. The axillary vein lies outside of the thoracic cage and can be easily imaged both in the longitudinal approach and the transverse method (7,24). We can see the entire needle, guidewire, dilator, and catheter in real-time in longitudinal view. So the longitudinal approach may be better than the transverse method. Our experience is that, for the skilled, the two methods are similar. In a transverse approach, the introducer needle crosses the plane of the ultrasound beam, and only the needle tip is seen. The shaft of the needle is not tracked. It is imperative to identify and track the needle tip. Advance the needle a few millimeters at a time while continuing to track the needle tip by subtly tilting the transducer back and forth.
In a longitudinal approach, the plane of the beam is parallel to the vessel, and the needle tip and shaft can be seen (7). Care must be taken to prevent the transducer from sliding over the artery. Limited data exist comparing the longitudinal versus transverse approach for CVC insertion (15,23,25), but most experts of ultrasound-guided procedures recommend learning the transverse approach first. The hand-eye coordination needed to perform a transverse approach is acquired easier than that of the longitudinal method.
The axillary vein is formed by the anastomosis of the brachial and basilic veins. Start by scanning along the inferior margin of the mid-clavicle with the transducer in a sagittal plane and slide the transducer laterally (15,26). Select the site where the axillary vein is most superficial and where the vein can be clearly distinguished from the artery. Avoid selecting a site too distal because of increased risk of complications. Choose the best insertion site of the target vein where vital structures surrounding the vein, specially artery and pleura, can be visualized.
We strongly recommend the use of color flow and/or pulsed-wave Doppler ultra-sound to confirm correct differentiation of axillary or subclavian artery and vein. We have a very important experience is that move only one hand at a time. When you change direction of the needle, keep the hand holding the transducer still. If the ultrasound transducer is moved to adjust the image, keep the hand advancing the needle still. Note the depth of the anterior venous wall in relation to the skin. If the needle has been advanced to the expected depth and a flash of venous blood has not been seen, find and confirm location of your needle tip. Do not insert the needle beyond the anticipated depth of the anterior wall without obtaining the red blood. Regardless of the approach used, it is most important to ensure proper placement of the needle tip, followed by the guidewire, in the lumen of the axillary.
The study has limitations. First, this study is a retrospective study. A larger prospective, randomized study is required to assess the difference of the two techniques. Second, the study was completed at a single center and the operators were experienced, therefore, the conclusion may not apply to other settings.
In conclusion, the ultrasound-guided axillary vein cannulation by experienced operators is very safe in the longitudinal approach and the transverse method. The rate of complications was very low in both groups of patients. The axillary vein can be successfully cannulated by experienced operators with good success. The longitudinal approach is associated with greater one-attempt success. The transverse method has shorter operation time.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Zhongshan Hospital of Fudan University and written informed consent was obtained from all patients.
References
- Dietrich CF, Horn R, Morf S, et al. Ultrasound-guided central vascular interventions, comments on the European Federation of Societies for Ultrasound in Medicine and Biology guidelines on interventional ultrasound. J Thorac Dis 2016;8:E851-E868. [Crossref] [PubMed]
- Liu P, Zhou YF, Yang P, et al. Optimized Axillary Vein Technique versus Subclavian Vein Technique in Cardiovascular Implantable Electronic Device Implantation: A Randomized Controlled Study. Chin Med J (Engl) 2016;129:2647-51. [Crossref] [PubMed]
- Gawda R, Czarnik T, Łysenko L. Infraclavicular access to the axillary vein - new possibilities for the catheterization of the central veins in the intensive care unit. Anaesthesiol Intensive Ther 2016;48:360-6. [Crossref] [PubMed]
- Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med 2011;39:1607-12. [Crossref] [PubMed]
- Czarnik T, Gawda R, Nowotarski J. Real-time, ultrasound-guided infraclavicular axillary vein cannulation for renal replacement therapy in the critical care unit—A prospective intervention study. J Crit Care 2015;30:624-8. [Crossref] [PubMed]
- Batllori M, Urra M, Uriarte E, et al. Randomized comparison of three transducer orientation approaches for ultrasound guided internal jugular venous cannulation. Br J Anaesth 2016;116:370-6. [Crossref] [PubMed]
- Vogel JA, Haukoos JS, Erickson CL, et al. Is long-axis view superior to short-axis view in ultrasound-guided central venous catheterization? Crit Care Med 2015;43:832-9. [Crossref] [PubMed]
- O'Leary R, Bodenham A. Future directions for ultrasound-guided central venous access. Eur J Anaesthesiol 2011;28:327-8. [Crossref] [PubMed]
- Werner HC, Vieira RL, Rempell RG, et al. An Educational Intervention to Improve Ultrasound Competency in Ultrasound-Guided Central Venous Access. Pediatr Emerg Care 2016;32:1-5. [Crossref] [PubMed]
- Wadman MC, Lomneth CS, Hoffman LH, et al. Assessment of a new model for femoral ultrasound-guided central venous access procedural training: a pilot study. Acad Emerg Med 2010;17:88-92. [Crossref] [PubMed]
- Stefanidis K, Fragou M, Pentilas N, et al. Optimization of Cannula Visibility during Ultrasound-Guided Subclavian Vein Catheterization, via a Longitudinal Approach, by Implementing Echogenic Technology. Crit Care Res Pract 2012;2012:617149. [PubMed]
- Czarnik T, Gawda R, Nowotarski J. Real-time ultrasound-guided infraclavicular axillary vein cannulation: A prospective study in mechanically ventilated critically ill patients. J Crit Care 2016;33:32-7. [Crossref] [PubMed]
- Lin CP, Wang YC, Lin FS, et al. Ultrasound-assisted percutaneous catheterization of the axillary vein for totally implantable venous access device. Eur J Surg Oncol 2011;37:448-51. [Crossref] [PubMed]
- Bodenham A, Lamperti M. Ultrasound guided infraclavicular axillary vein cannulation, coming of age. Br J Anaesth 2016;116:325-7. [Crossref] [PubMed]
- Roger C, Sadek M, Bastide S, et al. Comparison of the visualisation of the subclavian and axillary veins: An ultrasound study in healthy volunteers. Anaesth Crit Care Pain Med 2017;36:65-8. [Crossref] [PubMed]
- Esmaiel A, Hassan J, Blenkhorn F, et al. The Use of Ultrasound to Improve Axillary Vein Access and Minimize Complications during Pacemaker Implantation. Pacing Clin Electrophysiol 2016;39:478-82. [Crossref] [PubMed]
- Gualtieri E, Deppe SA, Sipperly ME, et al. Subclavian venous catheterization: greater success rate for less experienced operators using ultrasound guidance. Crit Care Med 1995;23:692-7. [Crossref] [PubMed]
- Mitre CI, Golea A, Acalovschi I, et al. Ultrasound-guided external jugular vein cannulation for central venous access by inexperienced trainees. Eur J Anaesthesiol 2010;27:300-3. [Crossref] [PubMed]
- Schmidt GA, Maizel J, Slama M. Ultrasound-guided central venous access: what's new? Intensive Care Med 2015;41:705-7. [Crossref] [PubMed]
- Brass P, Hellmich M, Kolodziej L, et al. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev 2015;1:CD011447. [PubMed]
- Bentley SK, Seethala R, Weingart SD. Ultrasound-guided axillary vein approach to the subclavian vein for central venous access. Ann Emerg Med 2008;52:475. [Crossref] [PubMed]
- Brass P, Hellmich M, Kolodziej L, et al. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev 2015;1:CD006962. [PubMed]
- Sommerkamp SK, Romaniuk VM, Witting MD, et al. A comparison of longitudinal and transverse approaches to ultrasound-guided axillary vein cannulation. Am J Emerg Med 2013;31:478-81. [Crossref] [PubMed]
- Pittiruti M, Biasucci DG, La Greca A, et al. How to make the axillary vein larger? Effect of 90° abduction of the arm to facilitate ultrasound-guided axillary vein puncture. J Crit Care 2016;33:38-41. [Crossref] [PubMed]
- Shrestha GS, Gurung A, Koirala S. Comparison between long- and short-axis techniques for ultrasound-guided cannulation of internal jugular vein. Ann Card Anaesth 2016;19:288-92. [Crossref] [PubMed]
- Buzançais G, Roger C, Bastide S, et al. Comparison of two ultrasound guided approaches for axillary vein catheterization: a randomized controlled non-inferiority trial. Br J Anaesth 2016;116:215-22. [Crossref] [PubMed]


