Tuberculosis control programs and challenges in developed cities with intermediate disease burden: China experience
Tuberculosis (TB) remains one of the world’s deadliest infectious disease (1). Historically, it not only posed threats in developing countries, but also affected population in the developed world. From a global perspective, more guidance and focus were prioritized in low-income countries and rural areas due to their high TB burdens. Recently, the World Health Organization (WHO) proposed the End TB Strategy targets (90% reduction in TB incidence and 95% reduction in TB deaths by 2035) and the action framework in low-incidence countries (1,2). However, how to strive for TB elimination in urban areas with intermediate disease burden is still not well understood.
China had made great efforts and achievements in TB control. The TB notification rates, in most developed cities like Hong Kong Special Administrative Region (Hong Kong) and Shanghai, decreased sharply in last few decades and became stable within the intermediate level. Despite the different organizational health structures and TB control schemes, Hong Kong and Shanghai represent two of the most successful TB control models in China. A comparative viewpoint of context and public health system in TB control would enable us to identify the diverse programs, experiences and challenges. Hopefully it can raise more discussions, provide insights for each other, and also for other cities which will eventually evolve into economically “rich” and endemically “intermediate” ones.
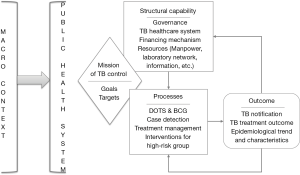
Applying a structure-process-outcome model, a conceptual framework is adopted to facilitate the understanding in a comprehensive way (see in Figure 1) (3). From macro context perspective, despite the stable political, better social-economic and population health status in Hong Kong and Shanghai, the large population size (7.2 and 24.2 million in 2013), high density of population and per capita living space, urbanization, increasing number of the elderly (aged 65 years and older, accounted for 14% and 18% in 2013), mobile residents, people living with high-risk factors for TB (such as HIV, diabetes and lung cancer), pose new challenges for the TB control programs (4,5).
The overall goal of a TB control program is to reduce TB morbidity and mortality by breaking the chain of transmission. In Shanghai, strategic targets within TB program were formulated and updated every five or ten years. TB is a notifiable disease in Hong Kong since 1939 by Quarantine and Prevention of Disease Ordinance and Occupational Safety and Health Ordinance (6). In Shanghai, TB report is statutory since 1959 in line with the Law on the Prevention and Treatment of Infectious Diseases (7). However, no exclusive TB laws or regulations exist for more strict policy such as compulsory isolation or treatment.
Integrated healthcare systems are fundamental for TB control programs in two cities but organized in different ways (6,7). It poses a challenge for Hong Kong which has a mixed public-private provider and financing system. The majority of TB patients are managed in 17 Hong Kong public chest clinics which provide primary ambulatory care. The chest clinics are also responsible for TB surveillance, treatment, defaulter and contact tracing, health education, Bacille Calmette-Guerin (BCG) vaccination and research. Public outpatient clinics and private practitioners can also provide clinical services and/or refer them to chest clinics. In secondary care, TB patients are treated for multi-drug resistance TB (MDR-TB) or complications in public and private clinics and hospitals. In shanghai, TB designated hospitals (TB hospital), community healthcare services and Centers for Disease Control and Prevention (CDCs) are effectively integrated. Thirty-three TB hospitals are responsible for clinical diagnosis, treatment and management of TB patients. Sections of the hospitals are designed of hospitalization for MDR-TB, complications and inpatient care. All 247 community health centers and 13 township clinics take charge of referral of TB suspects or patients to nearest TB hospitals, close contact and default tracing, health education and directly observed therapy (DOT). CDCs are responsible for program management, surveillance, laboratory quality assurance, technical assistance, health promotion, training, research, monitoring and evaluation.
Undoubtedly, effective healthcare systems only work within sustainable financing mechanisms which provide universal access to high-quality healthcare services. To avoid financially catastrophic cost due to TB, patients in Hong Kong chest clinics and Shanghai TB hospitals are provided with free TB clinical services (6,7). Additional supplements or incentives are provided for vulnerable population like older and poor people by giving medical voucher, transportation subsidies or living allowances. The rates of healthcare workers (TB programmatic, clinical and laboratory staff), to 100,000 citizens ranged from 1.78 to 3.13 in two cities (7,8). Well-equipped laboratories and networks are built with capability to bacteriologically confirm TB and MDR-TB cases (6,7). Comparing web-based electronic TB information management system in Shanghai, TB information can be reported and collected by on-line system, fax, post and other channels in Hong Kong (6,7).
In most developed cities in China, BCG program for newborn babies and DOTS (Directly Observed Treatment, Short-Course) strategy have been well implemented with high coverage (6,7). In addition to optimize actions along the patient-initiated pathway within the effective healthcare systems, systematic screening which is predominantly provider-initiated in high-risk groups for TB is highly recommended as the key intervention towards TB elimination (9). In Hong Kong, close contact of infectious TB patient, patient with HIV infection, silicosis and other immunocompromised conditions, such as receiving anti-tumor necrosis factor therapies, are recommended for both latent and active TB screening with appropriate treatment (6). In Shanghai, integrated into health examination, the elderly and people with diabetes are recommended for screening active TB every year or every two years in partial districts (7). The school students and staff, healthcare and mineral workers, and prisoners are also the high-risk group for regular active TB screening (7).
As an effective way of improving medication adherence, DOT has proved to be increasingly difficult in urban areas probably due to privacy concerns, longer working hours, geographical inconvenience, low TB awareness and human rights claims. In Hong Kong, DOT is given in chest clinics and extended beyond working hours. For patients who have ambulatory difficulties, the therapy can be delivered by community nurses in their homes or nursing stuff in elderly institutions (6). In Shanghai, DOT is mainly administered by nurses in community health centers. Electronic reminders to improve medication adherence and health education, such as mobile text messaging and medication monitor boxes, have been integrated within management programs in pilot studies.
The overall downward trends of TB notification and mortality are observed in the past half-century (6-8). In Hong Kong, the TB notification rates decreased sharply from a peak of 697/100,000 in 1952 to 101/100,000 in 1995, and thereafter plateaus around 65/100,000 and to 2013. In Shanghai, the rates decreased rapidly before 2000s and then ran a fluctuating course around 30/100,000. TB mortality rates in both places decreased to less than 4/100,000 since 2007. The changing TB epidemiology may account for epidemiological characteristics (7,8). In Hong Kong, the elderly patients accounted for 15.3% of TB notification in 1985, increasing to 39% in 2004 and since, leveled off (6). Patients who were born outside Hong Kong accounted for more than 60% (10). In Shanghai, the elderly patients accounted for 16% and ranked as the highest notification rate, while internal migrants accounted for more than half of TB patients in 2013 (7). The treatment completion rates were both lower than 85% mainly due to the unfavorable treatment outcome respectively in the elderly and internal migrants (7,8).
In summary, under the integrated TB healthcare systems adapted to specific macro context in two cities, the affordable, accessible, available and acceptable TB services and control measures were designed to strive for the strategic targets of control programs. Despite the declined disease burden and good health infrastructure, TB control in Chinese developed cities will remain a major challenge in the following years. The decline of TB incidence may take longer time given the rapid pace of population ageing and large amount of internal migrants. Towards the End TB Strategy targets, effective interventions to rapidly reduce TB reservoir and prevent progression from latent TB infection are highly needed, as very high disease rates were observed during the past decades. The two cities could learn from each other in terms of specific measures and experience. Systematic screening for latent and active TB infection in high-risk groups, rapid diagnostics and effective therapy, innovation of DOT approach in urban residents warrant more research and evaluation to bridge the research and policy gaps. In addition, the joint efforts and engagements in a supportive social network are necessary in response to the social-economic determinants. The enhanced surveillance should be ready to accurately monitor TB epidemiology under the demographic changes happening in the developed cities.
Acknowledgements
Funding: This work was supported by the Health and Medical Research Fund [Number: CU-15-C12], Food and Health Bureau, Hong Kong Special Administrative Region, China.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- World Health Organization. Global Tuberculosis Report 2015. Geneva: World Health Organization; 2015.
- World Health Organization. Towards tuberculosis elimination: an action framework for low-incidence countries. Geneva: World Health Organization; 2014.
- Handler A, Issel M, Turnock B. A conceptual framework to measure performance of the public health system. Am J Public Health 2001;91:1235-9. [Crossref] [PubMed]
- Shanghai Municipal Bureau of Statistic. Shanghai statistical yearbook-2014. Shanghai: China Statistics Press. 2014.
- Census and Statistics Department, Government of the Hong Kong Special Administrative Region. Hong Kong Annual Digest of Statistics-2014. Hong Kong: Census and Statistics Department, Government of the Hong Kong Special Administrative Region; 2014. Available online: http://www.statistics.gov.hk/pub/B10100032014AN14B0100.pdf
- Department of Health, Government of the Hong Kong Special Administrative Region. Tuberculosis manual. Hong Kong: Department of Health, Government of the Hong Kong Special Administrative Region; 2006. Available online: http://www.info.gov.hk/tb_chest/doc/Tuberculosis_Manual2006.pdf
- Shanghai CDC, Final evaluation report of national TB programme 2011-2015. Shanghai: Shanghai CDC; 2015.
- Department of Health, Government of the Hong Kong Special Administrative Region. Annual Report 2013. Hong Kong: Department of Health, Government of the Hong Kong Special Administrative Region; 2014.
- World Health Organization. Systematic screening for active tuberculosis: principles and recommendations. Geneva: World Health Organization; 2013.
- Leung CC, Chan CK, Chang KC, et al. Immigrants and tuberculosis in Hong Kong. Hong Kong Med J 2015;21:318-26. [PubMed]


