Temperament and character profiles of male COPD patients
Introduction
Chronic obstructive pulmonary disease (COPD) is an inflammatory disorder of respiratory system and is characterized by persistent airflow obstruction that is generally irreversible (1). It is currently accepted to be as one of the major causes of chronic morbidity and mortality (2). COPD patients are exposed to severe physical limitations, such as impaired performance of daily living activities and due to dependent on long-term oxygen therapy for survival (3,4). Because of these limitations COPD patients have substantial psychosocial trouble (5,6). Anxiety and depression are accepted to be main co-morbidities in COPD patients (7) and both are associated with a poor prognosis (8,9).
Psychological characteristics are generally ignored in medical and treatment guidelines. There is growing findings that psychological or emotional distresses have effect on the quality of life in patients with COPD. As a comorbities anxiety and depression have been included in to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline criteria in 2011. It is also possible that other psychological variables, such as personality traits, may influence the progression of the illness, as well as treatment achievement and rehabilitation. There seems to be an existing impression among health professionals that COPD patients are exhausting to work with, as well as they are being generally non adherent to treatment plans (10,11).
Cloninger et al. investigate and distinguish personality into the temperament and character dimensions by the temperament and character inventory (TCI), which is known to be useful in clinical practice (12). Temperament is described as genetically homogenous and independently inherited and includes four dimensions. Moreover, character is described as demonstrating individual differences in self-concepts about values in relation to social experiences and consists of three dimensions. Temperament is accepted to be stable during the lifelong, but character can be affected by the environment. It is thought that genetic factors have effects of 10-15%, and living environmental factors have effects of 30-35% on character dimensions (13,14). Temperament dimensions are thought to be genetically independent qualities and are 40-60% inheritable and stable throughout life (12,14,15).
The aim of our study was first to investigate personality by Cloninger’s temperament and character model in patients with COPD and compared with healthy controls. COPD patients have higher rates of anxiety and depressive disorders (6,16), compared to normal persons. Anxiety and depression have well-known associations with various temperament and character traits (15,17). Also we aimed to investigate correlations between temperament and character dimensions and clinical factors such as severity of the disease, smoking, alcohol abuse, and psychological problems like depression and anxiety in patients with COPD.
Methods
The study was approved by the Ethics Committee of Kahramanmaras Sutcuimam University, School of Medicine and conducted according to the ethical standards of the Helsinki Declaration of 2000.
The COPD group consisted of the patients diagnosed and treated at the Department of Pulmonary Disease Clinic in Kahramanmaras University Hospital. The control group was chosen among the patients without any chronic illness, admitted to outpatient clinic of the Family Medicine and Pulmonary Disease Clinic between October 2010 and December 2010. In order to form a homogenous group, only male participants were included. They gave informed consent after receiving an explanation of the study. The questionnaires were completed alone or with the help of relatives in cases where the participant had inadequate education or was unable to understand the questions. The questionnaires were distributed to 277 patients; only 115 patients completed and brought them (return rate: 41.5%). A total of 9 patients were excluded because of incomplete registrations and age accordance (5 control patient excluded because of being lower than 43 years-old) and as a result, remaining 106 male patients were included to the study.
Thirty-nine male COPD patients diagnosed according to the GOLD criteria (18) and 67 age- and gender-matched healthy control group patients were enrolled into the study. Patients with current suicidal thoughts, serious physical conditions (diabetes mellitus, congestive heart failure, debilitating neurological and rheumatologic condition, etc.) and used psychotropic agents within the last six months were excluded from the study.
A spirometry device (ZAN 500 Plethysmograph) was used to diagnose COPD; the presence of a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) <70% confirms the presence of COPD. According to GOLD criteria, the severity of COPD was classified by FEV1 value into four Grades (Mild, FEV1 ≥80% predicted; Moderate, 50%≤ FEV1 <80% predicted; Severe, 30%≤ FEV1 <50% predicted; and Very Severe, FEV1 <30% predicted) (18,19). Blood oxygen saturation was measured from finger pulse oximeters.
Socio-demographic data forms containing age, BMI, education, gender, marital status, residing place, smoking history, alcohol abuse, presence of other medical disorders, smokeless tobacco history and duration and type of drugs being used were completed by the patients.
Temperament and Character Inventory consists of 240 questions, which are answered as true or false. It has been commonly used in different areas of psychological and psychiatric researches and practices recently. It was developed by Cloninger et al., and validity and reliability studies of the Turkish version have been performed (20,21). Cloninger’s model examines the character dimension by 3 scales: Self-directedness (SD, total of 44 items), Cooperativeness (C, total of 42 items), and Self-transcendence (ST, total of 33 items). These scales are investigated by 5 subscales for SD as Responsibility (SD, 8 items), Purposefulness (SD2, 8 items), Resourcefulness (SD3, 5 items), Self-acceptance (SD4, 11 items), and Congruence (SD5, 12 items); 5 subscales for C as Social acceptance (C1, 8 items), Empathy (C2, 7 items), Helpfulness (C3, 8 items), Compassion (C4, 10 items), and Integrated conscience (C5, 9 items); 3 subscales for ST as Self-forgetfulness (ST1, 11 items), Trans-identification (ST2, 9 items), and Spiritual acceptance (ST3, 13 itens). Also examines the temperament dimension by 4 scales: Novelty seeking (NS, total of 40 items), Harm avoidance (HA, total of 35 items), Reward dependence (RD, total of 38 items), and Persistence (P, 8 items). These scales are studied by, 4 subscales for NS as Exploratory (NS1, 11 items), Impulsiveness (NS2, 10 items), Extravagance (NS3, 9 items), and Disorderliness (NS4, 10 items); also 4 subscales for HA as Anticipatory worry or Pessimism (HA1, 11 items), Fear of uncertainty (HA2, 7 items), Shyness (HA3, 8 items), and Fatigability (HA4, 9 items); 3 subscales for RD as Sentimentality (RD1, 10 items), Attachment (RD3, 8 items), and Dependence (RD4, 6 items); no subscale for P (12,15,22).
Anxiety and depressive symptoms were assessed by using the confirmed Turkish version of the Hospital Anxiety and Depression Scale (HADS), which has been revealed to be a reliable instrument for the screening of anxiety and depression. It includes two parts, seven questions evaluating anxiety and another seven questions evaluating depressive symptoms. To measure HADS anxiety (HADS-A), a score of 11 or more was considered as indicative of anxiety and a HADS depression (HADS-D) score of eight or more was considered as indicative of depression (23,24).
The degree of dyspnoea was evaluated by using the Modified Medical Research Council (MMRC) dyspnoea scale. Scores range from 0 (‘‘I only get breathless with strenuous exercise’’) to 4 (‘‘I am too breathless to leave the house’’ or ‘‘I am breathless when dressing or undressing’’) (25).
Statistical analyses were carried out using the statistical package of SPSS 15.0 for Windows (SPSS, Inc., Chicago, IL, USA). Patients and controls were compared in terms of socio-demographic data by the Chi-squared test (if required, Fisher’s exact test was used) and the Student-t test. Correlation analysis was performed by Pearson’s for parametric variables and Spearman’s correlation analysis for non-parametric variables. In these analyses, the significance level was assumed to be P<0.05. Saturation was examined by one-way ANOVA and was followed by Tukey’s test posthoc.
Results
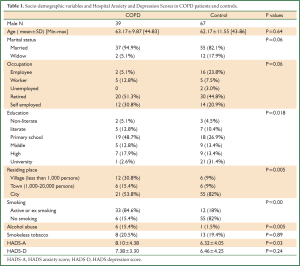
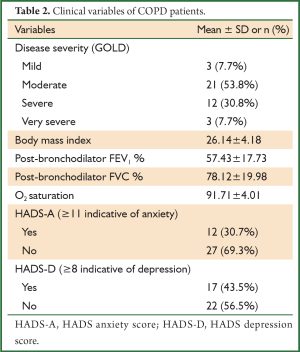
There were no significant differences between the COPD patients and the controls in term of demographic characteristics except in education, residing place, presence of smoking history and alcohol (Table 1). In our study, the prevalence of depression in COPD patients was 43.5%, in controls was 35.8%. The HADS-D score of COPD patients was not significantly higher than those of controls (P>0.05). We determined a positive correlation between depression and age of both COPD and control groups (P=0.03, r=0.21). The HADS-A score of COPD was significantly higher than those of controls (P=0.03) (Table 1). Also in our study, the prevalence of anxiety in COPD patients was 30.7%, in controls was 16.4%. The clinical variables of COPD patients are shown in Table 2.
Full Table
Full Table
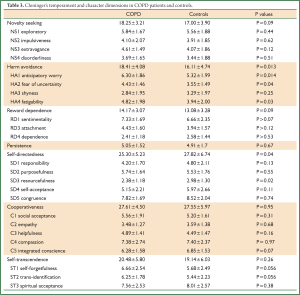
We found that in COPD patients, the Harm avoidance score was significantly higher and Self-directedness score was significantly lower than in controls (P=0.01, P=0.04 respectively). Anticipatory worry (HA1), Fear of uncertainty (HA2) and Fatigability (HA4) subscores were significantly higher and Resourcefulness (SD3) subscore was significantly lower in COPD patients (P=0.01, P=0.04, P=0.03, P=0.02, respectively) (Table 3). TCI dimensions were not correlated with the severity of COPD (P>0.05).
Full Table
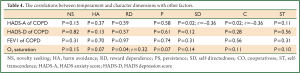
In COPD patients, HADS-A was negatively correlated with the Self-directedness and Cooperativeness scores (P=0.02 and P=0.02; r=–0.36, r=–0.36 respectively). In COPD patients HADS-D and age were not correlated to any of temperament and character dimensions (Table 4). In controls, age was negatively correlated with the Self-directedness and Cooperativeness scores and positively correlated with Harm avoidance score (P=0.02 and P=0.01, P=0.007; r=–0.27, r=–0.29, r=0.32, respectively).
Full Table
Discussion
Our study is the first one using the well-validated TCI personality questionnaire to compare personality characteristics of COPD patients to those of healthy controls. Temperament and character dimensions of personality are affected by genetic and environmental factors (26). COPD is evaluated by GOLD criteria and is known to be affected by genetic, socioeconomic and environment factors too. Although psychological processes other than anxiety and depression are generally not taken into account in medical and treatment guidelines and also researches indicate a high prevalence of psychological disorders in this population (10,11). In our study, we found that COPD patients had significantly higher mean score of Harm avoidance and significantly lower score of Self-directedness traits than healthy controls.
A meta-analysis from England identified a prevalence of major depression in patients with moderate-to-severe COPD in an out-patient setting of 40% (27). In a study of Turkey, the prevalence of depression in COPD male patients was 29.6% (28). Some studies reported a significant increase in the prevalence of depression, but others reported no significant differences between COPD patients and controls (29). In our study, the prevalence of depression was 43.5%, and these results are similar to other studies. In our healthy control group, the prevalence of depression was 35.8%. According to HADS-D score in our study, COPD patients were more depressive than controls but the difference was not significant. In a study, older alcohol user men were related to higher levels of depressive symptoms and higher levels of anxiety (30). In our study alcohol consumption was significantly more common in COPD group which they had not been using psychotropic drugs. In both groups of our study, we determined a positive correlation between age and depression. So the increased depression scores in both groups may be due to elderly age of our participants.
The symptom of dyspnoea, which is a major complaint of COPD patients, is accepted to be a potent stimulus for anxiety (31). Inability to perform daily activities or expected social roles may also lead them to feel anxious. Cigarette smoking, which is the primary cause of COPD, has also been strongly linked to anxiety symptoms. In the USA, unadjusted prevalence of anxiety was higher among those with COPD (15%) than in controls (6%) (8). In our country, Celik et al. found the prevalence of anxiety to be about 44% in COPD patients (32). In our study, the incidence of anxiety in COPD group was 30.7%, and in control group was 16.4%. These results are similar to those of other studies.
Only a few studies investigated the role of personality in COPD. In one study, COPD patients were found to be more neurotic than healthy controls (33). Other two prospective studies suggest that personality factors, such as neuroticism and pessimism, might play a role in the prevalence and course of disease (34,35). But the definite conclusions about the role of personality could not be drawn based on the previous reviewed studies. Temperament dimensions are known as differences between individuals’ automatic responses to danger, novelty and different reward types and are closely related to four basic emotions: harm avoidance to fear, Novelty seeking to anger, Reward dependence to attachment and Persistence to ambition (12,13,36). In a study, 25% of COPD patients had at least one fall event during walking in a year and 29% of COPD patients had increased fear of falling (16). In another study, COPD patients also had greater dyspnea-related fear (37). We found COPD patients to have higher Harm avoidance score and also have higher Anticipatory worry, Fear of uncertainty, Fatigability subscores than controls. The other name of Anticipatory worry is pessimism and our result was support other previous studies investigated personality by other than TCI in COPD (10,36). Higher Harm avoidance scores were detected with previous studies carried out on patients with asthma, fibromyalgia and other disorders (15,38). Due to chronic nature of these disorders, high harm avoidance score may be related to chronic disorders. Temperament Dimensions are also correlated with neurotransmitters: novelty seeking with low dopamine level, Harm avoidance with high serotonin and Reward dependence with low noradrenalin (13,39). Plasma serotonin levels are found to be higher in stable COPD patients than control subjects and the serotonin levels are not correlated with the severity of the disease. They also demonstrated a positive correlation between plasma serotonin levels and age in the COPD patients, but not in the control subjects (19,40). The Harm avoidance score is also positively related to the serotonin level and in COPD patients, the serotonin level is found to be increased (13,19). Silvertooth et al. (41) noted that citalopram, a selective serotonin reuptake inhibitor, did not change symptoms of anxiety or depression or self-reported physical function in COPD. These results suggest that in COPD patients, medication other than selective serotonin reuptake inhibitors may be more effective for anxiety or depression treatment. Extensive studies are needed to clarify this subject.
COPD patients experience a progressive reduction of functions and seem to be particularly susceptible to panic attacks. The respiratory complaint in patients with COPD may have effect on the development of panic attacks and anxiety (42). Our results presenting Anticipatory worry, Fear of uncertainty, and Fatigability subscores were higher in COPD and our results supported the Rose et al. study (42).
In our study, COPD patients were found to have lower Self-directedness score and Resourcefulness subscore. Individuals who are low in Self-directedness are described as immature, weak, fragile, blaming, destructive, ineffective, irresponsible, and poorly integrated and so they need others to make decision (36). They seem to be lacking an internal directorial attitude and handling with disability (14,43,44) Self-directedness is closely related to the perception of self-efficacy. Self-efficacy is defined as the personal conviction that one can successfully demonstrate problem-solving behaviour in a certain situation (45). In our COPD patients, Self-directedness score was significantly lower and anxiety was negatively correlated to Self-directedness score. Lower Self-directedness may be a result of chronic illness as mentioned in a study (45). As we know, this character score can be influenced by environment and so psychotherapy may be tried to improve this personality trait. We did not determine any correlation between the severity of COPD and TCI scores. Ashutosh et al. noted also no significant correlation between the Multifactorial Method for Personality Investigations scores and severity and all parameter of COPD like FEV1, FVC and FEV1/FVC (46).
There are some limitations in our study. The major one is that our sample size was small, and it may not be representative for all COPD patients. Further studies are required to confirm these results. We can describe no conclusions about cause-and-effect relationships because of the data’s cross-sectional nature. Finally, we used self-report scales to evaluate psychiatric symptoms, but it might be more reliable to use structured scales evaluated by psychiatrists.
Conclusions
The main clinical implication of our study is that in terms of temperament and character dimensions, male COPD patients have higher score of Harm avoidance and subscores of Anticipatory worry, Fear of uncertainty, and Fatigability and also have lower score of Self-directedness and subscore of Resourcefulness. Clinicians and psychiatrists should keep in mind the COPD patients’ personality traits while dealing with their treatment, but, in general, personality traits in COPD patients have been neglected. An understanding of the personality traits of patients may enable clinicians and psychiatrists to reduce these findings and improve quality of life among patients with COPD.
Acknowledgements
Disclosure: The abstract was submitted at 34. Turkish Respiratory Society Congress 6-10 October 2012 Çeşme, Turkey and won best poster award. The authors declare no conflict of interest.
References
- Celli BR. Update on the management of COPD. Chest 2008;133:1451-62. [PubMed]
- Raherison C, Girodet PO. Epidemiology of COPD. Eur Respir Rev 2009;18:213-21. [PubMed]
- Niewoehner DE. Clinical practice. Outpatient management of severe COPD. N Engl J Med 2010;362:1407-16. [PubMed]
- Katz PP, Gregorich S, Eisner M, et al. Disability in valued life activities among individuals with COPD and other respiratory conditions. J Cardiopulm Rehabil Prev 2010;30:126-36. [PubMed]
- Albuquerque SC, Carvalho ER, Lopes RS, et al. Ego defense mechanisms in COPD: impact on health-related quality of life and dyspnoea severity. Qual Life Res 2011;20:1401-10. [PubMed]
- Putman-Casdorph H, McCrone S. Chronic obstructive pulmonary disease, anxiety, and depression: state of the science. Heart Lung 2009;38:34-47. [PubMed]
- Hanania NA, Müllerova H, Locantore NW, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med 2011;183:604-11. [PubMed]
- Eisner MD, Blanc PD, Yelin EH, et al. Influence of anxiety on health outcomes in COPD. Thorax 2010;65:229-34. [PubMed]
- Ng TP, Niti M, Tan WC, et al. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med 2007;167:60-7. [PubMed]
- Hynninen KM, Breitve MH, Wiborg AB, et al. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res 2005;59:429-43. [PubMed]
- Rodríguez-Roisin R, Agustí A. The GOLD initiative 2011: a change of paradigm? Arch Bronconeumol 2012;48:286-9. [PubMed]
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry 1993;50:975-90. [PubMed]
- Cloninger CR. A systematic method for clinical description and classification of personality variants. A proposal. Arch Gen Psychiatry 1987;44:573-88. [PubMed]
- Cloninger CR, Przybeck TR, Svrakic DM, et al. The Temperament and Character Inventory (TCI): A guide to its development and use. St. Louis, MO: Center for Psychobiology and Personality, Washington University, 1994.
- Gulec MY, Gulec H, Oztuna F, et al. Cloninger’s temperament and character dimension of personality in patients with asthma. Int J Psychiatry Med 2010;40:273-87. [PubMed]
- Hellström K, Vahlberg B, Urell C, et al. Fear of falling, fall-related self-efficacy, anxiety and depression in individuals with chronic obstructive pulmonary disease. Clin Rehabil 2009;23:1136-44. [PubMed]
- Lu X, Chen Z, Cui X, et al. Effects of temperament and character profiles on state and trait depression and anxiety: a prospective study of a Japanese youth population. Depress Res Treat 2012;2012:604684.
- Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532-55. [PubMed]
- Lau WK, Chan-Yeung MM, Yip BH, et al. The role of circulating serotonin in the development of chronic obstructive pulmonary disease. PLoS One 2012;7:e31617. [PubMed]
- Kose S, Sayar K, Kalelioglu U, et al. Normative data and factorial structure of the Turkish version of the Temperament and Character Inventory. Compr Psychiatry 2009;50:361-8. [PubMed]
- Arkar H, Sorias O, Tunca Z, et al. Factorial structure, validity, and reliability of the Turkish temperament and character inventory. Turk Psikiyatri Derg 2005;16:190-204. [PubMed]
- Köse S, Sayar K. Ak İ ve ark. Turkish version of TCI: reliability, validity and factor structure. Bull Clin Psychopharmacol 2004;14:107-31.
- Aydemir O, Guvenir T, Kuey L, et al. Validity and Reliability of Turkish Version of Hospital Anxiety and Depression Scale. Turk Psikiyatri Derg 1997;8:280-7.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [PubMed]
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999;54:581-6. [PubMed]
- Gillespie NA, Cloninger CR, Heath AC, et al. The genetic and environmental relationship between Cloninger’s dimensions of temperament and character. Pers Individ Diff 2003;35:1931-46.
- Yohannes AM, Connolly MJ. Do antidepressants work in patients with chronic obstructive pulmonary disease with comorbid depression? Expert Rev Respir Med 2011;5:727-9. [PubMed]
- Kömürcüoğlu B, Balıoğlu M, Öztuna I, et al. KOAH’lı erkek olgularda depresyon (Depression among male COPD patients). Toraks Dergisi 2000;3:31-4.
- van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax 1999;54:688-92. [PubMed]
- Aartsen MJ, Comijs HC. Alcohol consumption and depressive symptoms among older adults: results of the Longitudinal Aging Study Amsterdam. Tijdschr Gerontol Geriatr 2012;43:127-36. [PubMed]
- Hill K, Geist R, Goldstein RS, et al. Anxiety and depression in end-stage COPD. Eur Respir J 2008;31:667-77. [PubMed]
- Çelik P, Esen A. Akın M ve ark. Kronik obstrüktif akciğer hastalığı olgularında depresyon. Solunum Hastalıkları 1998;9:25-32.
- Rutter BM. Some psychological concomitants of chronic bronchitis. Psychol Med 1977;7:459-64. [PubMed]
- Harthill ME. Psychosocial factors in pulmonary function and disease: a prospective investigation. Diss Abstr Int 1998;59:0903.
- Kubzansky LD, Wright RJ, Cohen S, et al. Breathing easy: a prospective study of optimism and pulmonary function in the normative aging study. Ann Behav Med 2002;24:345-53. [PubMed]
- Köse S. A Psychobiological Model Of Temperament And Character: TCI. Yeni Symposium 2003;41:86-97.
- Janssens T, De Peuter S, Stans L, et al. Dyspnea perception in COPD: association between anxiety, dyspnea-related fear, and dyspnea in a pulmonary rehabilitation program. Chest 2011;140:618-25. [PubMed]
- Gencay-Can A, Can SS. Temperament and character profile of patients with fibromyalgia. Rheumatol Int 2012;32:3957-61. [PubMed]
- Cloninger CR. A unified biosocial theory of personality and its role in the development of anxiety states. Psychiatr Dev 1986;4:167-226. [PubMed]
- Lee JJ, Chang CK, Liu IM, et al. Changes in endogenous monoamines in aged rats. Clin Exp Pharmacol Physiol 2001;28:285-9. [PubMed]
- Silvertooth EJ, Doraiswamy PM, Clary GL, et al. Citalopram and quality of life in lung transplant recipients. Psychosomatics 2004;45:271-2. [PubMed]
- Rose C, Wallace L, Dickson R, et al. The most effective psychologically-based treatments to reduce anxiety and panic in patients with chronic obstructive pulmonary disease (COPD): a systematic review. Patient Educ Couns 2002;47:311-8. [PubMed]
- Cloninger CR. A systematic method for clinical description and classification of personality variants. A proposal. Arch Gen Psychiatry 1987;44:573-88. [PubMed]
- Conrad R, Schilling G, Bausch C, et al. Temperament and character personality profiles and personality disorders in chronic pain patients. Pain 2007;133:197-209. [PubMed]
- Orhan FO, Ozer A, Sayarlioglu H, et al. Temperament and character profiles of end stage renal disease patients undergoing hemodialysis and peritoneal dialysis. Bull Clin Psychopharmacol 2011;21:201-9.
- Ashutosh K, Haldipur C, Boucher ML. Clinical and personality profiles and survival in patients with COPD. Chest 1997;111:95-8. [PubMed]


