Esophagogastric junction outflow obstruction-related functional chest pain treated using robotic-assisted thoracoscopic esophageal myotomy
Introduction
Esophagogastric junction (EGJ) outflow obstruction is characterized by elevated relaxation pressure in combination with intact or weak peristalsis and can be diagnosed using high-resolution manometry (HRM) (1,2). The integrated relaxation pressure (IRP) is associated with LES relaxation, crural diaphragm contraction and intrabolus pressure (2). Symptoms of EGJ outflow obstruction include dysphagia and atypical chest pain. The etiology remains uncertain and there is a lack of consensus regarding treatment. The disease can be classified as primary or secondary EGJ outflow obstruction. Secondary EGJ outflow obstruction is caused by a mechanical obstruction such as lack of EGJ relaxation, hiatal hernia, esophageal malignancy, esophageal stricture, external compression, mitochondrial myopathy, gastric band, or iatrogenic. Patients without mechanical obstruction are considered to have primary EGJ outflow obstruction. The prevalence of EGJ outflow obstruction is low (0.016) (3), and EGJ outflow obstruction is usually treated as gastroesophageal reflux disease. Reducing the cost of these treatments and making them accessible across the world will help reduce the burden due to refractory EGJ outflow obstruction. Herein, we present a case with chest pain that was diagnosed as EGJ outflow obstruction using HRM and treated using robotic-assisted esophageal myotomy.
Case presentation
A 43-year-old man with a history of headache and mitral valve disorder suffered from intermittent non-cardiac chest pain for about 20 years. The chest pain gradually worsened, and the patient experienced severe dysphagia. He underwent series of examinations to rule out the possibility of a cardiovascular disorder. He visited a local GI clinic where panendoscopy revealed gastroesophageal reflux. The Eckardt score was 9. The pain was poorly controlled with symptoms worsening despite more than 5 years of treatment with proton-pump inhibitors and hyoscine-N-butylbromide under the guidance of the local clinic.
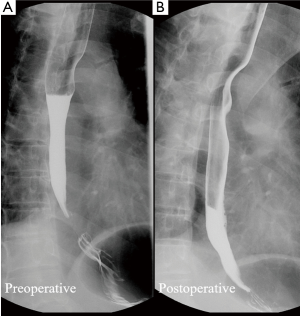
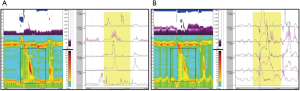
The patient underwent HRM and esophagraphy at the Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan and there was no acid reflux and chest pain during the examination. The esophagraphy reveal peristalsis passes normally through the entire esophagus (Figure 1A). The Chicago Calculation data for swallows (liquid) revealed an abnormal IRP. The median IRP was 15 mmHg (Figure 2A). The distal latency in 5 out of 10 swallows (5 mL each) was normal (>4.5 s), and for 6 out of 10 swallows, the contractile front velocity was normal (<9 cm/s). In addition, the median and maximum distal contractile integrals were 1,445 mmHg/s/cm (<5,000 mmHg/s/cm) and 2,725 mmHg/s/cm (<8,000 mmHg/s/cm), respectively. The amplitude of proximal esophagus (25.0 cm) was 49 mmHg; The amplitude of middle esophagus (30 and 35 cm) were 104 and 119 mmHg, respectively; The amplitude of distal esophagus (40 cm) was 102 mmHg. The HRM finds with elevated median IRP (>15 mmHg) and normal distal latency. The esophagraphy reveal peristalsis passes normally through the entire esophagus.
The patient was diagnosed as having EGJ outflow obstruction based on the Chicago Classification of esophageal motility disorders, v3.0 (4). However, the chest pain was not provoked during the HRM, thus the possibility of diffuse esophageal spasm (DES) was considered. We tried a calcium channel blocker and nitrite for pain control. The chest pain improved, but a side effect of severe headache occurred. After discussion, Because of worsening symptoms, the patient decided to undergo surgery and refused any additional attempt at endoscopic treatment.
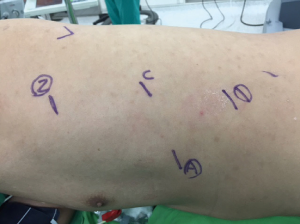
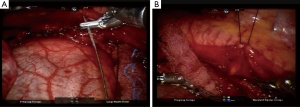
Robotic-assisted esophageal myotomy and Belsey-Mark IV fundoplication were performed with the patient in the right lateral semi-prone position and the thoracic cavity inflated with CO2 (Figure 3). Using the HRM findings that amplitude of middle esophagus (30 and 35 cm) were 104 and 119 mmHg, respectively, a long myotomy from the proximal (the aortic arch) to the distal (1.5 cm below the EGJ) level of the esophagus was performed and the vagus nerve was preserved. We used straight needle suture-gained traction of the posterior mediastinal pleura to expose the esophagus from the posterior mediastinum (Figure 4A,B). The esophagus is then encircled with a Penrose drain which aids in traction. A long myotomy was performed with da Vinci Maryland bipolar forceps. There was no perforation of the mucosa as confirmed by an intraoperative water test. The Robotic Belsey-Mark IV fundoplication for gastroesophageal reflux was performed. Total operation time was 3 hours 48 minutes. Post-operative esophagography showed no perforation. Chest pain related to the EGJ outflow obstruction was considerably improved after surgery. The patient was discharged 7 days after surgery. A postoperative 1 month HRM showed that the IRP was normal for all swallows (median, 8 mmHg). The distal latency in 3 out of 10 swallows (5 mL each) was normal (>4.5 s) and for 3 out of 10 swallows, the contractile front velocity was normal (<9 cm/s). In addition, the median and maximum distal contractile integrals were 460 mmHg/s/cm (<5,000 mmHg/s/cm) and 1,372 mmHg/s/cm (<8,000 mmHg/s/cm), respectively. The amplitude of proximal esophagus (24.0 cm) was 52 mmHg; the amplitude of middle esophagus (29 and 34 cm) were 43 and 75 mmHg, respectively; the amplitude of distal esophagus (39 cm) was 25 mmHg. A postoperative 1 month esophagography revealed that normal peristalsis passes normally through the entire esophagus (Figure 1B). Therefore, no motility disorders were detected by the postoperative HRM (Figure 2B). The patient was interviewed via telephone at 6 months and at 1 year. The patient reported no further chest pain or dysphagia. The postoperative Eckardt score were 1 and 1 at 6 months and 1 year telephone interviewed. Informed consent was obtained from the patient.
Discussion
The presenting symptoms in primary EGJ outflow obstruction are retrosternal pain, dysphagia, regurgitation, and weight loss (5). This characterization was based on a large cohort of patients undergoing HRM in which 34 out of 1,142 patients were diagnosed with primary EGJ outflow obstruction. Additional research has suggested that if patients with EGJ outflow obstruction present with dysphagia or chest pain as the main symptoms, the patient may need specific treatment and that endoscopic and surgical approaches are more effective than pharmacological treatment (6). This finding was based on a retrospective and prospective study of a historical cohort and a healthy control group that included 28 patients diagnosed with EGJ outflow obstruction receiving different therapeutic treatments including therapeutic abstention, pharmacological, botulinum toxin in the lower esophageal sphincter, endoscopic dilation, and surgery (fundoplication reversal). Extended myotomy with anterior fundoplication via laparotomy for severe DESs has been evaluated in a prospective study (7). In that study, the chest pain score was found to be satisfactory or excellent at 36 months of follow-up in all 20 patients, suggesting that medium-term postoperative functional results were excellent, especially in terms of dysphagia and chest pain (7). Therefore, extended myotomy with anterior fundoplication is an effective treatment for severe DES. Furthermore, several studies have demonstrated the safety and efficacy of the robotic platform for myotomy (8). These studies have revealed a low conversion rate, a low rate of intraoperative complications, and a low rate of postoperative complications. In addition, the robotic platform revealed a high rate of dysphagia resolution (8). In the current study, we presented a case in which a robotic-assisted esophageal myotomy and Belsey-Mark IV fundoplication successfully improved chest pain and dysphagia in a patient who could not tolerate medical treatment. Given these previous studies and our experience, we suggest that if a patient is diagnosed EGJ outflow obstruction, presents with dysphagia or chest pain, and cannot tolerate the side effects of medical treatment, then surgical intervention may be the most appropriate treatment.
Conclusions
EGJ outflow obstruction-related esophageal functional chest pain is almost without the need for any specific treatment. However, if the symptoms persist or the patient cannot tolerate the side effects of a medical treatment, long segment myotomy may be performed for symptom relief. A robotic system has advantages in terms of a magnified image and endowrist instruments. With these advanced techniques, surgeons can perform a more delicate myotomy and anti-reflux procedure. Thus, robotic systems may potentially play an important role in the treatment of EGJ outflow obstruction.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
References
- Sakin YS, Çelebi G, Kekilli M, et al. EGJ outflow obstruction must be excluded in patients with high IRP and weak peristalsis. Turk J Gastroenterol 2015;26:288. [Crossref] [PubMed]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24 Suppl 1:57-65. [Crossref] [PubMed]
- Scherer JR, Kwiatek MA, Soper NJ, et al. Functional esophagogastric junction obstruction with intact peristalsis: a heterogeneous syndrome sometimes akin to achalasia. J Gastrointest Surg 2009;13:2219-25. [Crossref] [PubMed]
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160-74. [Crossref] [PubMed]
- van Hoeij FB, Smout AJ, Bredenoord AJ. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol Motil 2015;27:1310-6. [Crossref] [PubMed]
- Pérez-Fernández MT, Santander C, Marinero A, et al. Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol Motil 2016;28:116-26. [Crossref] [PubMed]
- Leconte M, Douard R, Gaudric M, et al. Functional results after extended myotomy for diffuse oesophageal spasm. Br J Surg 2007;94:1113-8. [Crossref] [PubMed]
- Afaneh C, Finnerty B, Abelson JS, et al. Robotic-assisted Heller myotomy: a modern technique and review of outcomes. J Robot Surg 2015;9:101-8. [Crossref] [PubMed]


