Barbed suture material technique for wound closure and concomitant tube placement in uniportal VATS for pneumothorax
Introduction
Video-assisted thoracoscopic surgery (VATS) has become the reasonable modality with its efficacy in the treatment of primary spontaneous pneumothorax (PSP) for decades (1,2). Recently, uniportal VATS has been applied with minimally invasive concepts in various pulmonary diseases to establish its diagnostic and treatment role in VATS fields (3-5). Thus, several studies already have been described the feasibility of uniportal VATS for PSP over the multi-port VATS with its less invasiveness (6-8). However, a few reports have been introduced for wound management to achieve better cosmetic wound healing and for placement of the chest tube in uniportal VATS. Thus, we introduced a simple technique using knotless, absorbable barbed suture material for wound closure with concomitant anchoring the chest tube in uniportal VATS. In this study, we aimed to present our experiences of the barbed suture material technique in uniportal VATS for PSP, and to evaluate the surgical outcomes and feasibility.
Methods
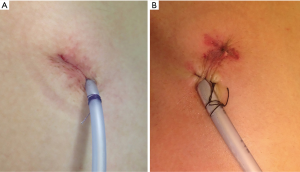
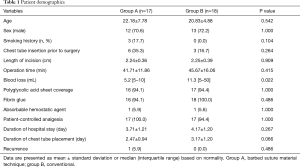
From July 2012 to December 2015, consecutive 31 patients (22 males) with a median age of 21.4 years (range, 14–43 years) underwent uniportal VATS to treat PSP by a single surgeon. Bilateral uniportal VATS were performed in 4 patients, thus total 35 cases were enrolled in this study. There were no patients having underlying pulmonary diseases or a history of trauma. We divided them into two groups with one group of 17 (48.5%) cases (group A), using barbed absorbable wound closure device (V-Loc™ Absorbable Wound Closure Device product line, Covidien, Mansfield, MA) for knotless, continuous wound closure with subsequent chest tube anchoring; and the other group of 18 (51.4%) cases (group B), using conventional suture anchoring with black silk fixation after skin closure using 4-0 braided synthetic absorbable suture device (PolysorbTM, Covidien, Mansfield, MA) (Figure 1). The surgical technique was chosen according to the surgeon’s preference. The patients were followed up using a chest X-ray at 1 week, 1 month, and every 6 to 12 months postoperatively. All patients were followed up during a median follow-up period of 18 months. Surgical outcomes between two groups were compared and analyzed, retrospectively. Institutional Review Board of our institute approved this study (IRB No: KC16RISI0886).
Surgical procedure of uniportal VATS for PSP
Under general anesthesia with double-lumen endotracheal tube intubation for selective one lung ventilation, the patient was placed in the lateral decubitus or supine position. After sterilization and draping procedure, a minimal skin incision (2.0–2.5 cm in length) was made in the fourth or fifth intercostal space at the anterior to middle axillary line. In cases with chest tubes, the tube insertion site was used for uniportal incision. Firstly, full thoracoscopic inspection from the apex to the base was routinely conducted to detect blebs or bullae using a high definition 5-mm, 30° thoracoscope (Karl Storz endoscope; Karl Storz, Tuttlingen, Germany) through the uniport. The wound protector was not routinely used. An identified apical bullae lesion was grasped using endo-grasper and resected with endostaplers (Echelon 60 Endopath stapler; Ethicon Endosurgery Corp., Cincinnati, OH, USA). We also explored the posterior or medial side of the lung thoroughly with retractions using thoracoscopic grasper or curved ring forceps under manipulation of 30° thoracoscope. Saline merging test using warm physiologic saline with manual positive-pressure ventilation was performed to confirm no air leakage. An absorbable polyglycolic acid (PGA) sheet (Neoveil; Gunze, Kyoto, Japan) was covered with fibrin glue (Beriplast-P combiset; CSL Behring GmbH, Marbug, Germany) to reinforce the resected staple lines.
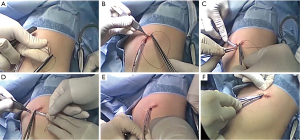
Continuous wound closure and chest tube anchoring using barbed suture material
A 16 or 20 Fr. chest tube was placed at the anterior or the posterior part of the uniportal wound under thoracoscopic guidance for appropriate positioning in the apex of the thoracic cavity. Muscle layer and subcutaneous tissue were approximated with a continuous suture technique using a single 2-0 braided synthetic absorbable suture (PolysorbTM, Covidien, Mansfield, MA, USA). Skin was approximated using a 3-0 or 4-0 barbed absorbable suture material in a unidirectional running fashion following hooking procedure into the locking hole after first stitch. Then, the barbed thread was continuously sutured toward the chest tube. The thread was turned around the chest tube like purse string fashion, and then suture out through the contralateral skin surface. Then, the needle is detached from the thread, and winded around the tube for anchoring purpose. Finally, the tip of the thread is passed under the winded thread using Mosquito forceps, and gently fastened (Figures 2,3). The wound was covered with steri-strips or dressing foam. The patient was extubated in the operation room and transferred with routine check-up of chest X-ray at the recovery.

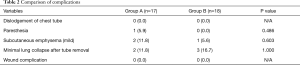
Technique for chest tube removal
The chest tube removal is decided after confirmation of neither air leakage nor residual pneumothorax on the chest X-ray. Firstly, the patient was placed in the supine or semi-lateral position, and a simple dressing was performed before removal procedure. Initially, we rewind the thread, but this procedure was not needed for simple withdrawal of the thread. Recently, we cut the stalk between the skin and the winded barbed suture material around the chest tube. However, to grasp the thread using forceps or fingertips, leaving a very short segment is avoided. After preparation of the patient’s exercise for breath, the tube will be smoothly removed at the pause of respiration. During removal procedure, the residual thread is gently pulled out for concomitant wound closure, directly after the end period of extraction of the chest tube (Figure 4). The small surgical gauze may cover on the minimal skin incision, and neither additional tying nor suture procedure is needed due to concomitant coaptation of the tube removal site.

Statistical analysis
Data are presented as mean with standard deviation or number of patient including percentage. The independent t-test was used for continuous variables and chi square or Fisher’s exact test was used for categorical variables. The P values <0.05 were considered to indicate statistical significance. All statistical analyses were performed with SAS (version 9.3; SAS Institute, Cary, NC, USA) or SPSS (version 19.0; SPSS Inc., Chicago, IL, USA).
Results
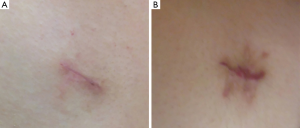
Demographic data demonstrate no significant difference in both groups except blood loss (Table 1). There was no significant difference in length of hospital stay (3.7±1.2 vs. 4.1±1.2 days, P=0.267) and in median chest tube indwelling time (2.4±0.9 vs. 3.1±1.2 days, P=0.066), respectively. Operation time in Group A was shorter than in Group B but there was no significant difference (41.7±11.8 vs. 45.6±16.0 minutes, P=0.415). There was neither conversion to two or three port VATS in all cases. All chest tubes were removed with concomitant sealing the tube removal site by pulling the suture material without difficulty. There was no statistical difference in minimal collapsed lung after tube removal (2 vs. 3, P=1.000) (Table 2). One recurrence was developed in Group A, but the patient was managed with small bore catheter placement due to minimal lung collapse on postoperative 2 months later. There were no wound problems such as dehiscence or infection in both groups during a median follow-up period of 18 months (Figure 5).
Full table
Full table
Discussion
Conventional multi-port VATS have been widely performed as a reasonable surgical modality with many advantages comparing to thoracotomy. Since 1998, single incisional thoracoscopic approach was introduced and has been increasingly performed for treatment of various thoracic diseases (3,4,11). Due to its less-invasiveness such as less pain and cosmetic reasons over the multi-port VATS, uniportal VATS have been broadened its application in lobectomy, limited resection pneumonectomy, even in complex sleeve procedures with favorable results by skillful techniques and accumulated experiences (4-6). For wedge resection, several reports have been demonstrated that single port VATS can be equivocally performed without increasing morbidities or recurrences (7,8,12-14). Thus, uniportal VATS for PSP is increasingly carried out as an alternative modality to the multi-port conventional VATS. Furthermore, various surgical techniques have been developed to achieve better outcomes for treatment of PSP using single, minimal incision (15-18). However, there has been no recommended method for wound closure and chest tube placement despite most surgeons have been trying to decrease the length of uniportal incision. And, we also noticed that the cosmetic wound healing was unsatisfactory using simple interrupted skin sutures or skin staplers, and conventional suture tying technique for tube placement which makes additional wound scars.
Recently, barbed suture materials have been introduced into various surgical fields, demonstrating its efficacy without increasing morbidities (19). In obstetric and gynecologic surgery, several reports reviewed the role of the knotless barbed suture with its tissue approximation ability and time, cost-effectiveness in vitro, animal model, and in human clinical trials (20). Randomized controlled trials also revealed unidirectional barbed suture with intracorporeal knots in laparoscopic myomectomy has equivalent to a conventional suture method for soft tissue reapproximation with acceptable outcomes (21,22). In cardiac surgery fields, the use of barbed suture material in mitral valve surgery was reported showing its usefulness, and randomized controlled trial also showed its feasibility for donor leg wound closure in coronary artery bypass surgery (23,24). In our institution, we have been using barbed suture material for both VATS and non-VATS surgery, and we have neither experienced technical difficulties nor increased morbidities. Thus, application of concomitant chest tube anchoring was followed for the uniportal VATS surgery.
For minimally invasive concepts, wound healing is an important concern that our technique will be beneficial and promising in uniportal VATS fields. A conventional surgical knot, skin stapling, and suture tying technique yield the foreign body material related surrounding inflammatory reaction. For optimized wound healing, minimizing knot sizes or knotless technique is crucial. We established better surgical outcomes with attaining an appropriate skin wound approximation and concomitant chest tube placement, resulting satisfactory cosmetics using single barbed absorbable suture material. Our experiences achieved precise wound closure with adequate tissue approximation without making conventional suture knots. For technical aspects, this technique made surgeon feel more comfortable in closing the minimal skin incision (2 cm) VATS. Moreover, chest tube removal procedure can be performed without difficulty for concomitant closure of the tube removal site by pulling the thread. This technique can be conducted without assistants, and additional tying or suturing is also needless. Furthermore, stitch out procedure was not required since residual knots do not exist. For cost problems, single V-Loc is not expensively charged compared to multiple Vicryl threads, and additional silk suture materials. Furthermore, many patients are willing to pay for postoperative wound care with customized scar formula despite high costs. Thus, we think that barbed suture material is worth to be used for various merits.
The primary purpose of pneumothorax surgery is an appropriate treatment to prevent recurrence with long-term effects. Despite of close VATS exploration and saline merging test, we could not find any tiny lesions in recurrence case. We think that subpleural concealed blebs may be the cause of minimal lung collapse or recurrence. Unfortunately, these findings are not always detectable even in multi-port VATS or thoracotomy. The combination of PGA sheet and surgical glue has shown the effective control for recurrence that we routinely use this method to achieve better outcomes (25). However, further study will be needed to establish its long-term effects.
In summary, we found that there was no difference in surgical outcomes between two groups, whose equivocal effectiveness was achieved without additional adverse effects. Thus, our method as the last step for wound and tube management is thought to be promising technique with the least invasive concepts in uniportal VATS surgery for PSP.
Conclusions
A continuous suture anchoring technique using knotless, barbed absorbable suture material achieved equivocal outcomes without complication and technical difficulty compared to the conventional suture anchoring method in uniportal VATS for PSP. We also identified its feasibility for tube removal and aesthetic wound healing. We suggest this simple technique with various technical advantages for wound closure and concomitant chest tube placement in uniportal VATS.
Acknowledgements
Funding: The statistical consultation was supported by a grant of the Korea Health Technology R & D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C1062).
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The study was approved by IRB of Seoul St. Mary’s Hospital (IRB No: KC16RISI0886) and written informed consents were waived.
References
- Naunheim KS, Mack MJ, Hazelrigg SR, et al. Safety and efficacy of video-assisted thoracic surgical techniques for the treatment of spontaneous pneumothorax. J Thorac Cardiovasc Surg 1995;109:1198-203; discussion 1203-4. [Crossref] [PubMed]
- Ng CS, Lee TW, Wan S, et al. Video assisted thoracic surgery in the management of spontaneous pneumothorax: the current status. Postgrad Med J 2006;82:179-85. [Crossref] [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Jutley RS, Khalil MW, Rocco G., et al. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Kim KS. Procedure of continuous wound closure and chest tube anchoring using barbed suture material. Asvide 2017;4:225. Available online: http://www.asvide.com/articles/1535
- Kim KS. Technique for chest tube removal. Asvide 2017;4:226. Available online: http://www.asvide.com/articles/1536
- Ng CS. Single-port thoracic surgery: a new direction. Korean J Thorac Cardiovasc Surg 2014;47:327-32. [Crossref] [PubMed]
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Qin SL, Huang JB, Yang YL, et al. Uniportal versus three-port video-assisted thoracoscopic surgery for spontaneous pneumothorax: a meta-analysis. J Thorac Dis 2015;7:2274-87. [PubMed]
- Han KN, Kim HK, Lee HJ, et al. Single-port thoracoscopic surgery for pneumothorax under two-lung ventilation with carbon dioxide insufflation. J Thorac Dis 2016;8:1080-6. [Crossref] [PubMed]
- Berlanga LA, Gigirey O. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax using a single-incision laparoscopic surgery port: a feasible and safe procedure. Surg Endosc 2011;25:2044-7. [Crossref] [PubMed]
- Son BS, Kim DH, Lee SK, et al. Small Single-Incision Thoracoscopic Surgery Using an Anchoring Suture in Patients With Primary Spontaneous Pneumothorax: A Safe and Feasible Procedure. Ann Thorac Surg 2015;100:1224-9. [Crossref] [PubMed]
- Tsuboshima K, Wakahara T, Matoba Y, et al. Single-incision thoracoscopic surgery using a chest wall pulley for lung excision in patients with primary spontaneous pneumothorax. Surg Today 2015;45:595-9. [Crossref] [PubMed]
- Tu CC, Hsu PK. Global development and current evidence of uniportal thoracoscopic surgery. J Thorac Dis 2016;8:S308-18. [PubMed]
- Murtha AP, Kaplan AL, Paglia MJ, et al. Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg 2006;117:1769-80. [Crossref] [PubMed]
- Greenberg JA, Goldman RH. Barbed suture: a review of the technology and clinical uses in obstetrics and gynecology. Rev Obstet Gynecol 2013;6:107-15. [PubMed]
- Alessandri F, Remorgida V, Venturini PL, et al. Unidirectional barbed suture versus continuous suture with intracorporeal knots in laparoscopic myomectomy: a randomized study. J Minim Invasive Gynecol 2010;17:725-9. [Crossref] [PubMed]
- Song T, Kim TJ, Kim WY, et al. Comparison of barbed suture versus traditional suture in laparoendoscopic single-site myomectomy. Eur J Obstet Gynecol Reprod Biol 2015;185:99-102. [Crossref] [PubMed]
- Watanabe G, Ishikawa N. Use of barbed suture in robot-assisted mitral valvuloplasty. Ann Thorac Surg 2015;99:343-5. [Crossref] [PubMed]
- Krishnamoorthy B, Shepherd N, Critchley WR, et al. A randomized study comparing traditional monofilament knotted sutures with barbed knotless sutures for donor leg wound closure in coronary artery bypass surgery. Interact Cardiovasc Thorac Surg 2016;22:161-7. [Crossref] [PubMed]
- Hong KP, Kim DK, Kang KH. Staple Line Coverage with a Polyglycolic Acid Patch and Fibrin Glue without Pleural Abrasion after Thoracoscopic Bullectomy for Primary Spontaneous Pneumothorax. Korean J Thorac Cardiovasc Surg 2016;49:85-91. [Crossref] [PubMed]


