Strategies to prevent aortic complications in Marfan syndrome
Introduction
Marfan syndrome (MFS) is an autosomal dominant disorder of the body’s connective tissue, caused by mutations in the fibrillin-1 (FBN1) gene. The estimated prevalence of the syndrome is 1 in 5,000 (1).
Dilation of the aorta (aortic aneurysm) is the gravest expression of MFS. This is a result of a weakening of the tissues in the aortic wall, resulting in reduced capacity to contain the forces created by the heart’s action. The natural history of aneurysm in the aorta is expansion of the aorta over many years, followed by dissection, rupture and premature death (2). The keys to treating the syndrome are: limiting sports, frequent scans, medical treatment, and opportune surgery at the right time (3). Current pharmacological treatment of MFS basically consists of beta-blocker (BB) therapy and angiotensin receptor blockers (ARBs II) (4). Over the last few years, there has been significant growth in the number of studies seeking a drug to slow the disease’s progress. This paper summarises therapeutic advances in slowing down the development of aortic complications.
Molecular and genetic pathogenesis of MFS
The genetic basis of MFS lies in mutations of the gene coding FBN1, which is found in chromosome 15q21.1 (5). FBN1 is a protein that is essential for forming microfibrils, which are the main structural, regulatory components of the extra-cellular matrix of the arterial (6) wall. Over 1,000 FBN1 mutations have been identified in people with classic MFS symptoms (7). FBN1 binds with a latent cytokine complex of transforming growth factor β (TGF-β), which regulates its activation and signalling. Murine models show that a lack of FBN1 is associated with excessive signalling by TGF-β, and by the activation of certain metalloproteinases, especially matrix metalloproteinases 2 and 9 (8). FBN1 gene mutations are found in up to 92% of patients (4). These changes affect the destruction of elastin and collagen. This leads to degeneration of the middle layer, causing progressive dilation of segments of the proximal aorta, predisposing the aorta to dissection. This loss of elasticity in the middle layer leads to progressive aorta stiffness and loss of distensibility. In MFS, normal haemodynamic stress factors are further accentuated by pressure and volume overloads caused by underlying diseases, such as hypertension and aortic insufficiency. This situation coincides with weakness in the wall of the aorta, perpetuating a vicious circle that leads to aortic complications (1).
Pharmacological treatment
The aim of medical treatment is to slow or stop the development of the clinical signs of MFS. Oral BB are the ‘gold standard’ for medical treatment of the cardio-vascular system. BB reduce the expulsion force of the left ventricle, thus reducing both arterial and pulse pressures. All these changes may reduce stress on the wall of the aorta. Initially, treatment by BB proved effective in reducing the dilation rate in both retrospective and prospective studies (9,10). Nevertheless, recent studies in children with MFS has raised doubts about the efficacy of BB therapy (11). Furthermore, many patients cannot tolerate BB either because they have asthma (a condition affecting 20% of children with MFS) or because of drug intolerance or side effects (which include dizziness, nightmares and lethargy). In addition, BB therapy does not alter the underlying disease process causing weakness in and dilation of the wall of the aorta (2). Most subsequent studies confirmed a lower aorta dilation rate but only suggested a reduction in mortality (12). Moreover, no benefit was seen in patients with marked aorta dilation (13).
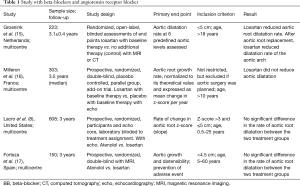
In the quest for therapeutic alternatives, Habashi et al. (14) first documented, in a murine model, the prevention and reversal of MFS-associated structural changes in the aorta by means of pharmacological resources. This study concluded that these results were due to the inhibiting effect of losartan on TGF-β. From this point on, various clinical trials have been conducted in an attempt to translate these results to MFS patients (Table 1).
Full table
Randomised studies have been carried out that compare ARBs with the base therapy. In this respect, we would like to highlight the Dutch COMPARE study and the French Marfan Sartan study.
The COMPARE (15) study covers a random, open, multi-centre drug trial evaluating the efficacy of losartan, although both the study groups received base treatment with BB. The trial was conducted in 233 adults aged over 18 and with MFS diagnosed in accordance with the original Ghent nosology (Ghent-1) criteria (18). Patients with an aorta diameter of >50 mm, a history of aortic dissection, or the presence of more than one vascular prosthesis were excluded from the study. The study revealed a significant drop in average arterial pressure in patients treated with losartan compared with those in the control groups. Among patients with native aortic root, the dilation rate of the aortic root shown by magnetic resonance (MR) and transthoracic echocardiography at the 3-year point was lower than in the group of patients treated with losartan. Nevertheless, there were no differences in the dilation rate in other aorta segments. Among patients with replacement of the baseline aortic root, the dilation rate of the aortic arch shown by MR at 3 years was less than in the group treated with losartan. There was no differential effect in the analysis of the sub-groups, including FBN1 mutation, average arterial pressure, the diameter of the aortic root, the concomitant BB therapy, gender and age. There were no significant differences between treatment groups in the final point of aortic dissection, the aortic surgery chosen, or cardio-vascular death (15). Despite this, using the same cohort of patients, Franken et al. recently found that cases of FBN1 mutations seemed to respond better to treatment with losartan (19).
Another similarly-designed randomised study was a French one—Marfan Sartan (16)—published by Milleron et al. It was a complementary, twin group, randomised, multi-centre trial with a placebo control. It evaluated treatment with losartan versus placebo combined with the standard preventive therapy. In the trial, comparisons were made of 299 patients over the age of 10 and with MFS. The Ghent-1 criteria were used for comparison (18) purposes. The study found that after 3.5 years of monitoring with transthoracic echocardiography, there were no statistically significant differences between the two groups with regard to the average diameters of the various segments of the aorta. There were also no significant differences in the clinical end-points (aortic dissection, aortic surgery, death, and so on) between the treatment groups (16).
Studies have also been conducted to compare ARB II with BB. Perhaps the most representative studies in this respect are those published by Lacro et al. and Forteza et al.
We would first like to highlight the Paediatric Heart Network Marfan trial published by Lacro et al. (8). This randomised study was conducted in 21 clinical centres in the United States, Toronto (Canada) and Ghent (Belgium). The study compared treatment of MFS with losartan and with atenolol in children and young adults. The study covered 608 individuals with MFS and employed the Ghent-1 criteria (18). The age of patients ranged between 6 months and 25 years. An aortic root z-score of over 3.0 formed part of the inclusion criteria for treating patients with atenolol or losartan. Monitoring was carried out through transthoracic echocardiography. The atenolol dose was raised to a maximum of 4 mg/kg/day with the aim of achieving a 20% average reduction in the heart rate. The losartan dose was raised to a maximum of 1.4 mg/kg/day following FDA guidelines. At the 3-year point, a small but significant difference was seen in average diastolic pressure, this being lower in the group treated with atenolol. There were small but significant differences in the annual average change in the aortic ring’s absolute diameter and z-score, with the atenolol group showing the better results. Nevertheless, there were no significant differences in other aorta segments. The fall in the aortic root’s z-score was more pronounced in younger patients, suggesting that it may be more effective to begin the therapy earlier on. At the 3-year point, there were no significant differences in aortic root surgery, dissection and death rates (8).
Another study, this time designed to compare the efficacy of treatment with ARB II versus BB, was published by Forteza et al. (17). This was a Spanish stage IIIb, parallel, randomised, double-blind study that sought to compare the efficacy of losartan and atenolol used as drugs to slow down aortic enlargement in MFS patients (as defined by the Ghent-1 criteria) (18). It included 140 patients, whose ages ranged between 5 and 60 years. An inclusion criterion was an aortic diameter of <45 mm. The maximum dose of losartan and atenolol was 1.4 mg/kg/day or 100 mg/day. The primary end point was the change in the aortic root and the maximum diameter of the ascending aorta indexed by corporal surface area. Monitoring after 36 months of treatment was conducted using MR. The study found no significant differences in changes in the indexed diameter of the aortic root between patients treated with losartan and those given atenolol, yet there was (17) a reduction in the area of the ascending aorta in the group receiving losartan.
As well as studies on ARB II and BB, various small-scale studies have been conducted to evaluate the use of angiotensin-converting enzyme inhibitor (ACE-inhibitor) in individuals with MFS. Their findings have been inconsistent. In an open, non-randomised study, Yetman et al. (20) compared the elastic properties of the aorta and the growth rate of the aortic root in 57 patients, prospectively monitored at an average interval of 3.0±0.2 years. The 32 patients in the study who received ACE-inhibitor showed an improvement in aortic distensibility, a reduction in aortic stiffness, a lower increase in the diameter of the aortic root compared with the 25 patients who received BB (atenolol or propranolol). By contrast, Phomakay et al. (21) retrospectively compared aortic growth rate in 67 MFS patients receiving one of the following: BB, ACE-inhibitor, neither of these. The enlargement rate of the aorta was almost normal in the BB group but was significantly higher in the groups receiving either ACE-inhibitor or left untreated (3). It is likely that more clinical trials are required and that these need to be broader, randomised and with longer monitoring intervals.
There are few studies on the use of calcium channel blockers as a preventative treatment of aortic enlargement in MFS. Once again, the results of such studies do not allow us to reach any conclusions.
Future treatment alternatives
Preliminary findings in MFS studies in rats suggest that the action of doxycycline as a non-specific inhibitor of MMP-2 and MMP-9 could reduce aortic root enlargement (22).
Statins, for example pravastatin, inhibit MMPs at the post-translational level, which may affect aortic root enlargement in MFS. Statins seem to have a similar effect to losartan in attenuating dilation of the aortic root in murine modelling of MFS. Such medication may prove clinically useful given that it is fairly well tolerated in long-term treatment (23).
Apart from these substances, experimental work is under way with various drugs, including resveratrol. Resveratrol (a polyphenol found in the skin of red grapes) lessens vascular cell senescence (discontinuous cell division) by inhibiting nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activity, thus reducing oxidation stress, which is somewhat dependent on the SIRT1 gene. There is data from experimental models that shows that resveratrol has a protecting effect on elastin integrity, thus slowing down aorta enlargement in MFS patients (24).
Conclusions
The results of current basic research and of randomised trials do not reveal one clear therapy for MFS patients. No doubt the genetic heterogeneity of samples and the short monitoring periods used in studies have not allowed differences to emerge regarding the comparative efficacy of the drugs tested. It is likely that the effect of the drugs depends on genetic and/or molecular factors that have yet to be established. Identifying such factors in the future should open the door to treatment that is tailored to each patient. Meanwhile, medical treatment of MFS should be based on the characteristics of each patient, including treatment tolerance, age, aorta size, family history of aortic dissection, genetic mutation, pregnancy, and other risk factors. All MFS patients exhibiting enlargement of the aortic root should receive treatment with suitable doses of BB or ARB II. Despite all the advances in pharmacology, one has to bear in mind that close monitoring and surgery are keys to saving lives in the aortic complications arising from this syndrome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Keane MG, Pyeritz RE. Medical management of Marfan syndrome. Circulation 2008;117:2802-13. [Crossref] [PubMed]
- Mullen MJ, Flather MD, Jin X, et al. A prospective, randomized, placebo-controlled, double-blind, multicenter study of the effects of irbesartan on aortic dilatation in Marfan syndrome (AIMS trial): study protocol. Trials 2013;14:408. [Crossref] [PubMed]
- Singh MN, Lacro RV. Recent Clinical Drug Trials Evidence in Marfan Syndrome and Clinical Implications. Can J Cardiol 2016;32:66-77. [Crossref] [PubMed]
- Pitcher A, Emberson J, Lacro RV, et al. Design and rationale of a prospective, collaborative meta-analysis of all randomized controlled trials of angiotensin receptor antagonists in Marfan syndrome, based on individual patient data: A report from the Marfan Treatment Trialists' Collaboration. Am Heart J 2015;169:605-12. [Crossref] [PubMed]
- Dietz HC, Cutting CR, Pyeritz RE, et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 1991;352:337-9. [Crossref] [PubMed]
- D'Arrigo C, Burl S, Withers AP, et al. TGF-beta1 binding protein-like modules of fibrillin-1 and -2 mediate integrin-dependent cell adhesion. Connect Tissue Res 1998;37:29-51. [Crossref] [PubMed]
- Chung AW, Au Yeung K, Sandor GG, et al. Loss of elastic fiber integrity and reduction of vascular smooth muscle contraction resulting from the upregulated activities of matrix metalloproteinase-2 and -9 in the thoracic aortic aneurysm in Marfan syndrome. Circ Res 2007;101:512-22. [Crossref] [PubMed]
- Lacro RV, Dietz HC, Sleeper LA, et al. Atenolol versus Losartan in Children and Young Adults with Marfan’s Syndrome. N Engl J Med 2014;371:2061-71. [Crossref] [PubMed]
- Shores J, Berger KR, Murphy EA, et al. Progression of aortic dilatation and the benefit of long-term beta-adrenergic blockade in Marfan's syndrome. N Engl J Med 1994;330:1335-41. [Crossref] [PubMed]
- Salim MA, Alpert BS, Ward JC, et al. Effect of beta-adrenergic blockade on aortic root rate of dilation in the Marfan syndrome. Am J Cardiol 1994;74:629-33. [Crossref] [PubMed]
- Gersony DR, McClaughlin MA, Jin Z, et al. The effect of beta-blocker therapy on clinical outcome in patients with Marfan's syndrome: a meta-analysis. Int J Cardiol 2007;114:303-8. [Crossref] [PubMed]
- Ladouceur M, Fermanian C, Lupoglazoff JM, et al. Effect of beta-blockade on ascending aortic dilatation in children with the Marfan syndrome. Am J Cardiol 2007;99:406-9. [Crossref] [PubMed]
- Chung AW, Rauniyar P, Luo H, et al. Pharmacologic relaxation of vein grafts is beneficial compared with pressure distention caused by upregulation of endothelial nitric oxide synthase and nitric oxide production. J Thorac Cardiovasc Surg 2006;132:925-32. [Crossref] [PubMed]
- Habashi JP, Judge DP, Holm TM, et al. Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science 2006;312:117-21. [Crossref] [PubMed]
- Groenink M, den Hartog AW, Franken R, et al. Losartan reduces aortic dilatation rate in adults with Marfan syndrome: a randomized controlled trial. Eur Heart J 2013;34:3491-500. [Crossref] [PubMed]
- Milleron O, Arnoult F, Ropers J, et al. Marfan Sartan: a randomized, double-blind, placebo-controlled trial. Eur Heart J 2015;36:2160-6. [Crossref] [PubMed]
- Forteza A, Evangelista A, Sánchez V, et al. Efficacy of losartan vs. atenolol for the prevention of aortic dilation in Marfan syndrome: a randomized clinical trial. Eur Heart J 2016;37:978-85. [Crossref] [PubMed]
- De Paepe A, Devereux RB, Dietz HC, et al. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 1996;62:417-26. [Crossref] [PubMed]
- Franken R, den Hartog AW, Radonic T, et al. Beneficial Outcome of Losartan Therapy Depends on Type of FBN1 Mutation in Marfan Syndrome. Circ Cardiovasc Genet 2015;8:383-8. [Crossref] [PubMed]
- Yetman AT, Bornemeier RA, McCrindle BW. Usefulness of enalapril versus propranolol or atenolol for prevention of aortic dilation in patients with the Marfan syndrome. Am J Cardiol 2005;95:1125-7. [Crossref] [PubMed]
- Phomakay V, Huett WG, Gossett JM, et al. β-Blockers and angiotensin converting enzyme inhibitors: comparison of effects on aortic growth in pediatric patients with Marfan syndrome. J Pediatr 2014;165:951-5. [Crossref] [PubMed]
- Yang HH, Kim JM, Chum E, et al. Effectiveness of combination of losartan potassium and doxycycline versus single-drug treatments in the secondary prevention of thoracic aortic aneurysm in Marfan syndrome. J Thorac Cardiovasc Surg 2010;140:305-12.e2. [Crossref] [PubMed]
- McLoughlin D, McGuinness J, Byrne J, et al. Pravastatin reduces Marfan aortic dilation. Circulation 2011;124:S168-73. [Crossref] [PubMed]
- Hibender S, Franken R, van Roomen C, et al. Resveratrol Inhibits Aortic Root Dilatation in the Fbn1C1039G/+ Marfan Mouse Model. Arterioscler Thromb Vasc Biol 2016;36:1618-26. [Crossref] [PubMed]


