Hybrid aortic repair with antegrade supra-aortic and renovisceral debranching from ascending aorta
Introduction
Aortic dissection is a life threatening condition and the most common presentation of acute aortic syndrome. Its incidence is about 5–30 cases per million people per year, and often it requires surgery (1).
The current available classifications are the DeBakey and Stanford schemes, being the latter the most widely used, but none considers the involvement of the aortic arch. Due to the fact that the evidence points to an initial nonsurgical treatment of aortic arch dissections, probably this entity should also be considered as a subgroup of type B dissections (2).
Dissections have been reported to affect the ascending aorta in 60% to 75% of the cases, the descending aorta from 30% to 35% and up to 19% in the aortic arch (3,4).
Hybrid repair has been described for the treatment of complex aortic pathology such as thoracoabdominal aortic aneurysms (TAAA) and type A and B dissections in order to deal with the presence of vital branches arising from the aortic arch and the renovisceral aorta. The debranching of these segments of the aorta creates new suitable landing zones for endografts.
Sometimes, aortic arch debranching can be performed without ascending aortic replacement, this is known as type I hybrid reconstruction and avoids the use of cardiopulmonary bypass. However, in other cases, because of ascending aorta dilation or due to the fact that manipulation of the diseased aortic arch during type I procedures is associated with retrograde aortic dissection, some authors advocate for ascending aortic replacement during the debranching surgery, which is known as a type II reconstruction. Currently, in centers with good experience with this techniques, hybrid and endovascular repair are the most frequently used methods of reconstruction of the aortic arch (5).
A recent development for treatment of complex aortic pathology is the Lupiae technique, which consists of a multibranched Dacron graft (Vascutek LupiaeTM) that can be used for thoracic debranching, and retrograde or antegrade renovisceral debranching. An in-hospital mortality from 4.2% to 8.4%; survival rates of 92%, 90% and 94% at 28 months, 6 and 8 years, have been reported with this procedure (6-9). A three-year estimated survival rate of 83%; freedom of type I endoleak and reintervention of 100% and 78%, respectively, have been also reported (10). A similar technique was previously described by Torsello et al., using three bifurcated Dacron grafts for an antegrade thoracic and renovisceral debranching (11).
Case presentation
A 68-year-old female was admitted to the Emergency Department due to severe back and chest pain with concomitant loss of consciousness. Her clinical records showed a past medical history of hypertension, Paget’s disease, cholecystectomy, appendectomy and a known chronic type B aortic dissection that was under follow-up at another center. The emergency angio-CT (computed tomography), showed a 6 cmc TAAA, due to a chronic type B dissection with involvement from Zone 0 of the aortic arch, extending to the right common iliac artery and to the left hypogastric artery. The celiac trunk and the right renal artery were also dissected, with all the renovisceral vessels arising from the true lumen.
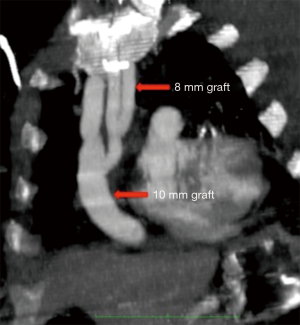
Initially the patient was transferred to the intensive care unit (ICU) for monitoring and blood pressure control. Seventy-two hours later, surgical treatment was decided because of the persistence of symptoms and difficult blood pressure control. An antegrade supra-aortic and renovisceral debranching was decided from ascending aorta due to extensive aortic disease with significant calcification at the renovisceral level and taking into account that the infrarenal aorta and both iliac arteries were not suitable as inflow sites. Under general anaesthesia and with cerebrospinal fluid (CSF) drainage, a median sternotomy was performed, allowing control of the ascending aorta and supra-aortic vessels. With tangential aortic clamping a 16×8 mm bifurcated Dacron graft was sutured to the ascending aorta with downward orientation of its limbs (Figure 1). From the main body of this bifurcated graft, a 10mm Dacron tube was used to debranch the brachiocephalic trunk performing a distal termino-terminal anastomosis. A 8mm Dacron graft was used to create a Y shaped graft, which was sutured proximally to the main body of the bifurcated graft and distally to both the left common carotid artery and the left subclavian artery (Figure 2). Then, a median laparotomy was performed, the renovisceral aorta was dissected and control of both renal arteries and superior mesenteric artery (SMA) was achieved. The celiac trunk was ligated, discarding its revascularization due to local dissection and that the preoperative angio-CT showed the presence of a good collateral network from the SMA.
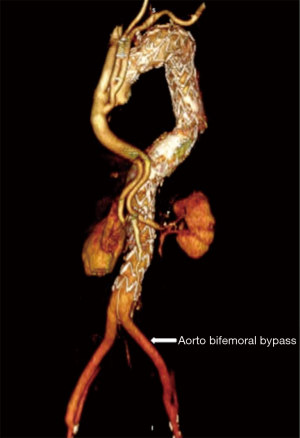
The bifurcated graft was tunnelled via the right anterolateral hemi-thorax through the diaphragm and behind the left lobe of the liver and pancreas, in order to perform a termino-terminal anastomosis to both renal arteries. The SMA was re-implanted in the left limb of the bifurcated graft that had been previously used for left renal revascularization. After completion of the supra-aortic and renovisceral revascularization, the infrarenal aorta was resected and an aorto-bifemoral bypass (Dacron 22×11 mm) was performed, leaving a long body segment in the graft for an adequate distal landing zone of the endoprosthesis.
Finally, endovascular access was gained through both femoral limbs of the aorto-bifemoral graft and four thoracic endoprosthesis were used to cover form the ascending aorta (distal to the origin of the supra-aortic debranching), down to the body of the bifurcated infrarenal graft (Figure 3). Completion angiography showed no endoleaks, correct placement of the endografts and patency of all revascularization branches.
The postoperative period was uneventful except for a long mechanical ventilation weaning process. There were no procedural-related neurological or visceral complications and the patient was discharged in good general condition. Follow-up studies were conducted with angio-CT at six and twelve months and yearly thereafter. At the moment, three years after the surgical procedure, the patient is doing well and free of intervention-related complications.
Discussion
Different options are available for the treatment of complex aortic pathology (aortic dissection and TAAA) including open, hybrid and total endovascular repair.
Conventional surgery is still associated with substantial perioperative morbi-mortality rates, especially in the elderly and fragile patients, which are however, the fastest growing segment of the population. A recent report comparing open and hybrid repair for TAAA showed that patients selected for hybrid procedures were significantly older and showed greater comorbidities (12). Despite this fact, there were no significant differences in the in-hospital mortality and postoperative paraplegia rates between the two groups. There was an increased rate of reintervention due to endoleaks in the hybrid surgery group. One and five-year survival rates were 69% and 32% respectively, in the hybrid group vs. 77% and 56% in open group. The worse late survival rate appears to be mainly influenced by a higher comorbid disease burden in the hybrid patient group (12). Some authors consider hybrid TAAA repair a procedure with unacceptable morbidity and mortality, suggesting that high-risk patients with TAAA should receive a non-interventional approach (13). Patel et al. showed a severe criticism of the hybrid treatment for TAAAs. They compared a group of patients at high risk for conventional surgery in whom a hybrid procedure was performed with another one including patients for a classical operation, and they found that the combined rate of mortality-paraplegia was double in the hybrid group (21.7% hybrid vs. 11.7% conventional). However, upon analysing these results, there is a clear selection bias in this study when comparing patients presenting with more comorbidities and more complex and extensive TAAAs in the hybrid group (61% type I or type II and it does not include any type IV), with another group of patients completely different, in which the type IV TAAAs means the 34% of the cases, and the aneurysms type I and II aneurysms just represent 28% of them (14).
Dilatation or the presence of a tear involving the aortic arch can be considered indications for total arch replacement with surgical alternatives like the Lupiae technique (15). Regarding the renovisceral vessels; with their particular pros and cons, antegrade or retrograde debranching can be an excellent option, mainly when other lesser invasive options are not possible due to extensive disease or complex anatomical factors (tortuosity, kinking or narrow vascular lumen, problems with access, small or duplicated vessels) or the patient can not wait for a customized device, like the case herein reported.
Good results have been showed with antegrade renovisceral debranching from the ascending aorta, despite the need to combine sternotomy and abdominal approach at the same time (16). The majority of authors perform a retrograde renovisceral revascularization from the distal aorta or iliac axis. However, the distal thoracic aorta or ascending aorta can also be used for antegrade revascularization, which is more physiological, with better inflow and avoids calcification or disease of the distal aorta or iliac vessels.
Several benefits are associated with staged procedures, such as a shorter duration of the intervention, lesser hypothermia and blood loss, with lower paraplegia rates. On the contrary, a single approach offers the possibility to deploy endografts, protecting the visceral grafts from embolization, checking the patency of the supra-aortic and/or renovisceral revascularization and it avoids the risk of rupture while waiting for the endovascular stage (17).
Creation of a long proximal and distal landing zones allows for the correct repair of the intimal tear, reduces the risks of type Ia and Ib endoleaks and is associated with a high probability of thrombosis of the false lumen in cases with aortic dissection. In general, the ICU and postoperative length of stay is shorter than with the traditional open repair. Open repair is still considered the gold standard method of treatment for TAAA, with excellent reported results from high volume centres. However, not all the patients have access to such institutions. Probably, for selected patients, the total endovascular repair would be the desirable option. The reduced invasiveness associated to fenestrated or branched endografts is beyond question, however these are also complex procedures and moreover, there are anatomic challenges, manufacturing delays and financial restrictions that can limit their applicability. The advantages of hybrid repair are mainly achieved when these procedures are applied to extensive aneurysmal disease and for such cases it remains a flexible and durable treatment (18).
In summary, the combination of endovascular and open revascularization of supra-aortic and renovisceral vessels can be a good strategy for selected cases unfit for open repair or for those with anatomical conditions not suitable for a total endovascular repair.
Acknowledgements
None.
Footnote
Conflicts of Interests: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and accompanying images.
References
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The international registry of acute aortic dissection (IRAD). JAMA 2000;283:897-903. [Crossref] [PubMed]
- Lempel JK, Frazier AA, Jeudy J, et al. Aortic arch dissection: a controversy of classification. Radiology 2014;271:848-55. [Crossref] [PubMed]
- Lansman SL, Raissi S, Ergin MA, et al. Urgent operation for acute transverse aortic arch dissection. J Thorac Cardiovasc Surg 1989;97:334-41. [PubMed]
- Lansman SL, McCulough JN, Nguyen KH, et al. Subtypes of acute aortic dissection. Ann Thorac Surg 1999;67:1975-78. [Crossref] [PubMed]
- Faulds J, Sandhu HK, Estrera AL, et al. Minimally invasive techniques for total aortic arch reconstruction. Methodist Debakey Cardiovasc J 2016;12:41-44. [Crossref] [PubMed]
- Marullo AGM, Bichi S, Pennetta RA, et al. Hybrid aortic arch debranching with staged endovascular completion in DeBakey type I aortic dissection. Ann Thorac Surg 2010;90:1847-53. [Crossref] [PubMed]
- Esposito G, Pennesi M, Bichi S, et al. Hybrid multistep approach to mega-aortic syndrome: the Lupiae technique. Eur J Cardiothorac Surg 2015;47:126-33. [Crossref] [PubMed]
- Esposito G, Cappabianca G, Ciano M, et al. Mid-term results of the Lupiae technique in patients with DeBakey Type I acute aortic dissection. Eur J Cardiothorac Surg 2012;42:242-7; discussion 247-8. [Crossref] [PubMed]
- Esposito G, Cappiabianca G, Bichi S, et al. Hybrid repair of type A acute aortic dissections with the Lupiae technique: Ten-year results. J Thorac Cardiovasc Surg 2015;149:S99-104. [Crossref] [PubMed]
- Troisi N, Bichi S, Patrini D, et al. Hybrid three-stage repair of mega aorta syndrome with the Lupiae technique. J Thorac Cardiovasc Surg 2013;145:S171-7. [Crossref] [PubMed]
- Torsello G, Can A, Umscheid T, et al. Hybrid thoracoabdominal aneurysm repair with simultaneous antegrade visceral revascularization and supra-aortic debranching from the ascending aorta. J Endovasc Ther 2007;14:342-46. [Crossref] [PubMed]
- Benrashid E, Wang H, Andersen ND, et al. Complementary roles of open and hybrid approaches to thoracoabdominal aortic aneurysm repair. J Vasc Surg 2016;64:1228-38. [Crossref] [PubMed]
- Patel R, Conrad MF, Paruchuri V, et al. Thoracoabdominal aneurysm repair: Hybrid versus open repair. J Vasc Surg 2009;50:15-22. [Crossref] [PubMed]
- Alonso M, Camblor LA, Gonzalez M, et al. Abdominal hybrid procedures fro treatment of complex thoracoabdominal aortic aneurysms. Angiologia 2016;68:491-8.
- Di Bartolomeo R, Leone A, Di Marco L, et al. When and how to replace the aortic arch for type A dissection. Ann Cardiothorac Surg 2016;5:383-88. [Crossref] [PubMed]
- Vivacqua A, Albacker TB, Roseli EE. Hybrid thoracoabdominal aneurysm repair with antegrade visceral debranching from the ascending aorta: concomitant cardiac surgery and stent-grafting. Ann Thorac Surg 2011;92:2275-7. [Crossref] [PubMed]
- Donas KP, Torsello G, Lazaridis K. Current status of hybrid procedures for thoracoabdominal and pararenal aortic aneurysm repair. J Endovasc Ther 2010;17:602-8. [Crossref] [PubMed]
- Jenkins MP, Haulon S, Greenberg RK, et al. Debate regarding the best surgical option for type IV thoracoabdominal aortic aneurysms. J Vasc Surg 2011;54:258-67. [Crossref] [PubMed]