Anomalous right coronary artery origin with interarterial pathway—importance of morphological origin assessment and the role of percutaneous interventionism
Introduction
Anomalies in Coronary Arteries (CA) are an important issue in cardiology and cardiovascular surgery. In this sense, it is an important entity because of its clinical impact, risk of sudden death (SD), prevalence and practical management complexity (1). For this reason they require a multidisciplinary approach, which includes the clinical Cardiologist, the Cardiovascular Surgeon and other specialists such as interventional Cardiologists and Cardiovascular Radiologists. Specifically, the assessment of the anomalous origin of the right coronary artery (RCA) is of special importance because it is the most frequent anomaly and also presents different possibilities of approach, depending on the form of presentation. Specifically we wanted to review the clinical situation of the anomalous RCA origin with interarterial pathway, regarding two clinical cases presented in our hospital.
Both the anterior descendent artery and the RCA are the elemental components of the coronary circulation and therefore both must be present to be considered a normal coronary circulation. In addition, in the case of RCA, it is defined as that subepicardial artery located in the right atrioventricular sulcus and gives rise to at least one acute marginal branch. The origin in the right sinus of Valsalva is therefore not an indispensable condition to identify this artery, but in those cases in which this does not happen, we would be talking about a situation of anomalous RCA origin (2). In these situations of anomalous CA origin, the description of the arterial pathway in relation to the large vessels (Pulmonar and Aorta Arteries) is also important, in order to rule out the presence of an interarterial pathway (3), due to the risk of ischemia and SD in these cases (4).
Coronary artery anomalies are described in a classic manner with an incidence of around 1%, although in different studies these were between 1.16% in consecutive studies of coronary Angio computed tomography (CT) (5) and 5.6% in consecutive records of invasive Coronary Artery Angiography (6). The anomalous RCA origin is the most common anomaly within these, with a general prevalence in the adult population ranging from 0.1% to 0.3% (5,7).
The clinical presentation of this entity is very variable. It may appear as dyspnea, syncope, precordial pain or even SD. The risk of SD is variable among the different studies. In post-mortem studies of individuals with SD, the prevalence of coronary anomalies ranges from 0.6% in the general population (8) to 23% in young athletes (9), with RCA accounting for around 46% of cases in the general population registry. The mechanism responsible for the clinic is not clear and several hypotheses have been proposed. In the case of interarterial pathways, compression in situations of increased cardiac output is postulated as the main cause of symptomatology in these patients, but it is also necessary to take into account the angulation at the origin of CA, accentuated in situations of exercise, as well as other extrinsic or intrinsic obstructions to the artery (4).
In the specific case of the anomalous origin of the RCA, the 2008 AHA/ACCA clinical practice guidelines on congenital heart disease recommend the revascularization treatment in cases of interarterial pathway and documented myocardial ischemia, with a level of recommendation IA. In cases without documented ischemia but where hypoplasia, compression or obstruction is evident by other imaging techniques the level of recommendation is IIA (10).
The revascularization in this entity is generally surgical, being the most widespread approach at present. However, there are documented cases of satisfactory percutaneous coronary intervention in obstructive CA cases (11,12) and our group believes that this may be a sensible approach in certain circumstances, as presented in this paper.
We report two different cases of patients with anomalous origin of RCA and associated interarterial pathway. With them we want to highlight the different presentation forms of these patients and the different diagnostic alternatives available in each of the steps. Furthermore, based on the recommendations of the clinical practice guidelines published, as well as the different evidences available to date, we intend to create a small diagnostic algorithm that facilitates the adequate management of this type of patients.
Case presentation
Clinical case 1
A 40-year-old male athlete, with no history of cardiovascular risk factors or cardiovascular pathology, consults in cardiology outpatient clinic for atypical precordial pain. It is done an exercise stress test that is conclusive and negative for ischemia, but because clinical persistence it is decided to perform CT angiography of CA. This shows an anomalous origin from the left Valsalva sinus of the RCA, with interarterial trajectory and without compression or stenosis. It was decided to complete the study with Coronary Artery Angiography that does not show any angiographic narrowing and with Exercise Perfusion Scintigraphy, which is also negative.
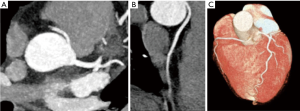
The case is presented in a multidisciplinary session, where because the absence of inducibility of ischemia in the performed tests, it is decided to manage conservatively. Subsequently, the patient is followed in our outpatient clinic remaining asymptomatic. In addition, stress echocardiography is performed during the follow-up, with the intention of actively discard subclinical ischemia in the evolution, which is negative (Figure 1).
Clinical case 2
A 75-year-old woman, with a history of arterial hypertension and dyslipidemia on pharmacological treatment for 5 years, has no cardiovascular history of interest. It is evaluated in Cardiology outpatient clinic by repeated episodes of precordial pain with the effort and an Exercise Perfusion Scintigraphy is realized being negative. Subsequently, she consulted in the emergency department for symptomatic progression, where electrocardiogram and routine laboratory tests (including myocardial damage markers) were performed, all with normal results.
As usual management within the precordial pain protocol in the emergency room, Coronary Artery Angiography is performed. This shows an RCA with anomalous origin in the left Valsalva sinus, interarterial pathway and luminal loss at this level.
The case is presented in multidisciplinary session, where given the age of the patient, as well as the possibility of a satisfactory percutaneous approach, it is decided to program for percutaneous treatment. Angioplasty with a stent implantation is performed on coronary lesion located in the interarterial pathway of the RCA, with satisfactory angiographic result. Two days later the patient is discharged from the hospital without clinical recurrence and is subsequently evaluated in outpatient clinic where the good clinical evolution of the cardiology is verified.
Discussion
In the patient with anomalous origin of the RCA and associated interarterial pathway, the first step after establishing the diagnosis is to rule out the presence of inducible ischemia, since in these cases the general recommendations are to revascularize to reduce the symptoms and the risk of SD. In those patients in whom ischemia induction tests are negative, the second step is to adequately assess the interarterial pathway, in order to rule out obstructions or compressions that also justify revascularization.
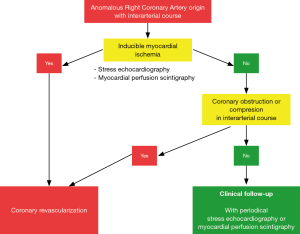
In those cases in which all the tests are negative, the current evidence does not recommend revascularization, but adequate periodic follow-up is recommended to rule out a possible appearance of clinical angina. In these cases, our group is also a strong supporter of the active search for ischemia. This is the periodic performance of an ischemia induction test that may reveal some degree of silent ischemia. For this reason, we believe that the stress echocardiogram and Exercise Perfusion Scintigraphy (based on availability and experience in each center) are fundamental because of their high sensitivity and specificity. Figure 2 shows a simplified algorithm that we believe may be useful for the clinician, in order to handle these patients adequately.
In the first case presented, we found a patient with anomalous origin of the RCA, asymptomatic interarterial pathway and negative ischemia induction tests. In these cases, after completing the appropriate complementary tests (Coronary Angio CT and Coronary Artery Angiography), an eventual compression or obstruction in this arterial pathway is ruled out. For this reason it was decided not to revascularizate this patient and not to follow up him periodically. In addition to periodic clinical follow-up, the active search for ischemia is necessary either with a stress echocardiogram or with an Exercise Perfusion Scintigraphy.
The case of patient number 2 is completely different. In this case, despite the history of negative ischemia induction tests, it presents an evident compression in the interarterial pathway (Figure 3). This is evidenced by both the Coronary Angio CT and the Coronary Artery Angiography. This is important because despite initially negative ischemia tests, any kind of compression or obstruction that compromises the vascular caliber should always be carefully discarded. Accordingly to clinical practice guidelines, these patients are also candidates for revascularization for symptomatic improvement and risk of SD reduction, despite the presence of negative ischemia detection tests.
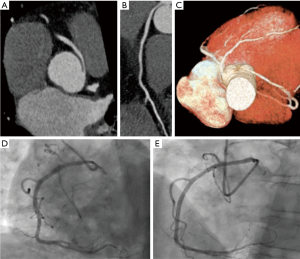
Finally, we would like to highlight the role that percutaneous interventionism can play in this type of clinical cases. There are several published cases of percutaneous approach with satisfactory results (11,12). In this sense case number 2 is an elderly patient, in which the percutaneous approach is feasible. Once the case has been evaluated in a multidisciplinary session, percutaneous coronary intervention is decided and the result is satisfactory.
Commentary
Coronary anomalies are frequent congenital heart diseases, with anomalies in the origin of RCA being the most frequent. In addition, it is an entity with significant clinical relevance because of the risk of associated myocardial ischemia and SD, especially related to the practice of intense physical exercise.
It is important to emphasize the need for a careful anatomical evaluation with different imaging techniques, in order to rule-out associated anomalies, beyond the interarterial pathway, which may be responsible for the symptomatology. Initial management includes different cardiac imaging techniques (Coronary Angio CT and Coronary Artery Angiography fundamentally), in order to discard compression or significant obstruction in the RCA interarterial pathway. In cases in which these initial tests do not present data compatible with compression or obstruction, it is important to perform other functional tests to detect myocardial ischemia such as Exercise Perfusion Scintigraphy and stress echocardiography.
Finally, it is important to highlight the role that percutaneous approach of these lesions can play in these patients. Especially as in the presented case, with patients of high surgical risk because of the advanced age and in whom the percutaneous approach is feasible.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation 2002;105:2449-54. [Crossref] [PubMed]
- Angelini P, Coronary artery anomalies--current clinical issues: definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 2002;29:271-8. [PubMed]
- Pérez-Pomares JM, de la Pompa JL, Franco D, et al. Congenital coronary artery anomalies: a bridge from embryology to anatomy and pathophysiology--a position statement of the development, anatomy, and pathology ESC Working Group. Cardiovasc Res 2016;109:204-16. [Crossref] [PubMed]
- Basso C, Maron BJ, Corrado D, et al. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol 2000;35:1493-501. [Crossref] [PubMed]
- Namgung J, Kim JA. The prevalence of coronary anomalies in a single center of Korea: origination, course, and termination anomalies of aberrant coronary arteries detected by ECG-gated cardiac MDCT. BMC Cardiovasc Disord 2014;14:48. [Crossref] [PubMed]
- Angelini P, Villason S, Chan AV Jr, et al. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Philadelphia: Lippincott Williams & Wilkins, 1999; 27-150.
- Szymczyk K, Polguj M, Szymczyk E, et al. Prevalence of congenital coronary artery anomalies and variants in 726 consecutive patients based on 64-slice coronary computed tomography angiography. Folia Morphol (Warsz) 2014;73:51-7. [Crossref] [PubMed]
- Drory Y, Turetz Y, Hiss Y, et al. Sudden unexpected death in persons less than 40 years of age. Am J Cardiol 1991;68:1388-92. [Crossref] [PubMed]
- Maron BJ, Shirani J, Poliac LC, et al. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA 1996;276:199-204. [Crossref] [PubMed]
- Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation 2008;118:2395-451. [Crossref] [PubMed]
- Shah N, Cheng VE, Cox N, et al. Percutaneous Coronary Intervention of an Anomalous Left Main Coronary Artery Arising from the Right Sinus of Valsalva. Heart Lung Circ 2015;24:e123-6. [Crossref] [PubMed]
- Komatsu T, Yaguchi I, Yufu T. Successful percutaneous coronary intervention of an anomalous right coronary artery with high anterior takeoff using a DIO thrombus aspiration catheter. J Invasive Cardiol 2012;24:E185-7. [PubMed]


