Aortic polyaneurysmal disease: case report
Introduction
Polyaneurysmal disease and arteriomegaly are frequently associated entities. Up to 13% of patients with aortic aneurism present multiple locations. Most of them (72%) are diagnosed together while the other are subsequently done. The primary aneurysm are more frequently the abdominal one, in fact the most common pattern is the infrarenal injury associated to another in the thoracic descending aorta (1).
A complete evaluation of the aorta is recommended in light of the existence of an aneurysm, specially when the first location is the thoracic, due to the high probability of an abdominal concurrent one. Also it is recommended when the patient is younger than usual (2).
Case presentation
A 78-year-old man was referred to our department with a casual find of an infrarenal aortic abdominal aneurism (AAA) in the context of an imaging test because of chronic spine arthrosis pain. The patient had no clinical symptoms associated with the aneurism.
In a more detailed anamnesis, the patient referred that he underwent open repair of an infrarenal AAA 20 years ago by median laparotomy and aorto-aortic tube prosthesis.
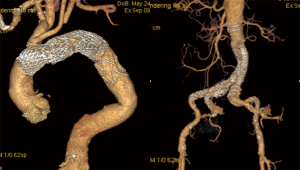
A full computed tomography (CT) scan revealed aneurysmatic pathology in three locations: descendant thoracic aorta close to the arch (with left subclavian artery affected) and infrarenal aorta above previous surgery both in a surgical range diameter, and left iliac artery aneurysm involving the internal, but not in range at that moment. An open surgery approach was rejected due to extension, patient age, previous abdominal surgery, co-morbidities such us chronic bronchitis and the existence of a favorable anatomy for the endovascular treatment. Therefore we scheduled a repair of the thoracic and the abdominal aneurysms with endografts and ambulatory image follow-up with the left iliac one. Both endoprosthesis were deployed through bifemoral access. The thoracic aneurysm required covering the left subclavian artery with the deployment of one 40 mm × 170 mm stent graft (E-vita THORACIC, Jotec GmbH) distal to innominate trunk in a short landing zone (0.9 mm length), the left carotid artery originates from the trunk. There was no leak in control angiography but regarding potential future complications such us migration or later endoleak one non-covered 40 mm × 130 mm stent (E-XL, Jotec Gmbh) was deployed from distal ascending aorta to the middle length of the previous stentgraft. The infrarenal aneurysm was managed with a 32 mm × 12 mm × 12 mm bifurcated stent graft (anaconda, Vascutek Ltd, a Terumo Company) extending to left iliac artery with 12 mm × 80 mm plus 12 mm × 90 mm grafts and 12 mm × 100 mm plus 12 mm × 80 mm to the right preserving both internal iliac arteries. During and after the procedure cerebrospinal fluid drainage was established in order to prevent spinal cord injury (SCI). The postoperative evolution was favorable and three days after surgery the patient was discharged from hospital.
Yearly CT scan (Figure 1) follow-up was scheduled, for surveillance of non treated iliac aneurysm and thoracic and abdominal endovascular procedure. In the next 4 years there were no complications in previous surgery but the iliac pathology increased his size to surgical range, therefore a new “endo” approach was scheduled.
With bifemoral access the intervention was started. Then, both iliac axis were connected using a snare wire due to the high angulated bifurcation of previous abdominal stent graft. In the right position, a bifurcated iliac stent graft 14 mm × 12 mm × 8 mm (E-iliac, Jotec GmbH) was released, after that a covered balloon-expandable 10 mm × 37 mm stent (BeGraft, Bentley Innomed GmbH) was deployed connecting the bifurcated graft with the left internal iliac artery preserving direct flow to this artery. In the control angiography a stenosis in the right branch of the previous abdominal stent graft was seen so it was managed with an iliac 14 mm × 40 mm stent (Protege Everflex, Covidien a Medtronic company). The postoperative evolution occurred without complications and the patient could leave the hospital 2 days after procedure.
Nowadays, period control CT scan are still being performed and the patient is asymptomatic, without endoleaks neither migration. He present now a non-complicated visceral aorta aneurysm which its growth is followed-up periodically.
Discussion
Despite improvement of surgical techniques and strategies, open surgery for multiple aortic aneurysms is still highly invasive. In fact, 30-day mortality after surgery has been reported to be 5–14% (3). In addition, co-morbidities such as renal dysfunction, cardiac disorders, and chronic obstructive pulmonary disease are critical issues to deal with. On the other hand, the endovascular approach has been reported as a reasonable alternative improving perioperative complication rates (4) and allows the treatment in aged patients. However, this technique have a significantly higher reintervention rate with necessitates follow-up surveillance imaging of these repairs (5). A simultaneous treatment of thoracic and abdominal aneurysms can be performed successfully with minimal morbidity and mortality and this is an alternative to staged repair (6), even more in this kind of patients who probably will require further interventions.
The SCI after thoracic aneurysm repair is a devastating complication both in open repair and endovascular. Although a thoracic endovascular stent graft often occludes the segmental artery connecting to the Adamkiewicz artery, the incidence of paraplegia is lower compared with open repair. Higher blood pressure and lower blood loss during endovascular repair are associated with a low incidence of SCI (7). This also indicates that spinal cord blood supply is unlikely to depend on a single segmental artery, and occlusion of one of these arteries may not be the only causative factor affecting SCI (8). Cerebrospinal fluid drainage is effective for preventing this complication (9) and should be considered to deploy a stent graft as short as possible.
The risk of a future type I endoleak is higher in thoracic landing zones 0–2 and also associated with the covered of the left subclavian artery (10), in our case a non-covered stent through the aortic arch could help for a stronger implantation of the thoracic stent graft. After 5 years there is no type I endoleak and the patient has not suffered complications related with the non-covered stent.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Crawford ES, Cohen ES. Aortic aneurysm: a multifocal disease. Presidential address. Arch Surg 1982;117:1393-400. [Crossref] [PubMed]
- Gloviczki P, Pairolero P, Welch T, et al. Multiple aortic aneurysms: the results of surgical management. J Vasc Surg 1990;11:19-27; discussion 27-8. [Crossref] [PubMed]
- Coselli JS, Bozinovski J, LeMaire SA. Open surgical repair of 2286 thoracoabdominal aortic aneurysms. Ann Thorac Surg 2007;83:S862-4; discussion S890-2.
- Desai ND, Burtch K, Moser W, et al. Long-term comparison of thoracic endovascular aortic repair (TEVAR) to open surgery for the treatment of thoracic aortic aneurysms. J Thorac Cardiovasc Surg 2012;144:604-9; discussion 609-11. [Crossref] [PubMed]
- Chang JM, Davila VJ, Lanza LA, et al. Endovascular repair of expanding thoracic aortic aneurysms in high surgical risk patients. Ann Card Anaesth 2016;19:158-61. [Crossref] [PubMed]
- Guo Y, Cai H, Yang B, et al. Simultaneous Endovascular Repair for Thoracic and Abdominal Aortic Pathologies: Early and Midterm Results. Ann Vasc Surg 2017;40:178-82. [Crossref] [PubMed]
- Leurs LJ, Bell R, Degrieck Y, et al. Endovascular treatment of thoracic aortic diseases: combined experience from the EUROSTAR and United Kingdom Thoracic Endograft registries. J Vasc Surg 2004;40:670-9; discussion 679-80. [Crossref] [PubMed]
- Fukui S, Tanaka H, Kobayashi K, et al. Development of Collaterals to the Spinal Cord after Endovascular Stent Graft Repair of Thoracic Aneurysms. Eur J Vasc Endovasc Surg 2016;52:801-7. [Crossref] [PubMed]
- Weigang E, Hartert M, von Samson P, et al. Thoracoabdominal aortic aneurysm repair: interplay of spinal cord protecting modalities. Eur J Vasc Endovasc Surg 2005;30:624-31. [Crossref] [PubMed]
- Kanaoka Y, Ohki T, Maeda K, et al. Analysis of Risk Factors for Early Type I Endoleaks After Thoracic Endovascular Aneurysm Repair. J Endovasc Ther 2017;24:89-96. [Crossref] [PubMed]