Analysis of the risk factors of postoperative cardiopulmonary complications and ability to predicate the risk in patients after lung cancer surgery
Introduction
Lung cancer is one of the most commonly diagnosed cancers all over the world and remains the leading cause of cancer-related deaths in China (1). Surgery was one of the most sufficient treatments for patients with lung cancer. However, with optimal surgical treatment, more than 20% of patients designated as early stages by conventional criteria would recur, and several eventually died of recurrent lung cancer (2,3). Because of the lung loss, functions of respiratory system and circulation system might be badly influenced. Complications might be developed for many patients after pulmonectomy and these complications could even be fatal. The lung infection, cardiac functional insufficiency and arrhythmia after pulmonectomy were the most common difficult problems perplexing surgeons with a high rate of fatality (4,5). This study was to investigate the causes of pulmonectomy complications by collecting clinical information of 653 patients underwent lung cancer surgery.
Material and methods
We conducted a retrospective study of 653 patients with lung cancer who underwent lung cancer surgery at Tianjin Cancer Institute and Hospital from January to December 2014. Data were collected for ages, genders, smoking status, medical histories of respiratory and circulation systems, blood responding quotas, forced expiratory volume in one second (FEV1)% Forced vital capacity (FVC)%, surgical approaches, extent of resections and pathological stages. Complete resection was defined as cancer-free surgical margins, both grossly and histologically. In addition, preoperative evaluation included medical histories, physical and laboratory examinations.
Of the 653 surgical lung cancer patients, 186 patients were aged 65 years or older. 386 patients were males. In our study, 584 patients underwent complete pulmonary resection and systematic node dissection, among these patients, 510 patients were performed lobectomy with lymph node dissection, 38 patients were performed pneumonectomy with lymph node dissection, 36 were performed segmentectomy with lymph node dissection and 69 patients underwent palliative pulmonary resection.
In this study, cases were excluded in patients who had lung infection or other infective diseases before surgeries, used antibiotic before surgeries, were given tracheotomy and other traumatic operations or those with long time of mechanical ventilation, who were liable to get secondary infection. Lung infection was diagnosed based on the following evidences: the main evidences include coughing, expectorating, bilateral or unilateral lung with wet rales or percussion dullness, chest CT or chest X-ray showed new or progressive exudative lesions; Secondary evidences include fever with body temperature ≥38 °C, peripheral blood white cells being equal to or more than 10×109 /L, secretion and lavage fluid culture positive by deep sputum bacterial culture and fiber optic bronchoscopy. Arrhythmia was recorded only when patients with arrhythmia needed to be treated. Cases with postoperative sinus tachycardia were not recorded as arrhythmia when induced by fever or pain.
The study was approved by institutional ethics committee of Tianjin Medical University Cancer Institute and Hospital (No. Ek2017088).
Statistical analysis
Related factors of pulmonary infection and arrhythmia after lung cancer surgery were estimated using Univariate Analysis of Chi-square test table. For multivariate analysis, non-conditional logistic regression analysis was applied. We determined the variables for multivariate analysis that showed a statistical significance in Univariate analysis for pulmonary infection and arrhythmia after lung cancer surgery. All statistical analysis above was carried out using the statistical package SPSS for windows 22.0 (Chicago, USA). P values <0.05 were considered statistically significant. All tests were two-sided. The factors, which were proved to be statistical significance, such as history of smoking, history of chronic bronchitis (binary variables) and actual clinical data such as ages, mode of operations, lymphocyte counts (continuous variables), were selected for calculating a predicting formula of complications incidences using R program. According to analysis by R program, age, lymphocyte count, surgical methods had a strong correlation to postoperative pulmonary infection which was a kind of generalized multiple linear regression. We adopted y=a+bx+cx2, quadratic curve fitting, and used linear regression to fit the factors of smoking history, history of chronic bronchitis.
Results
Lung infection
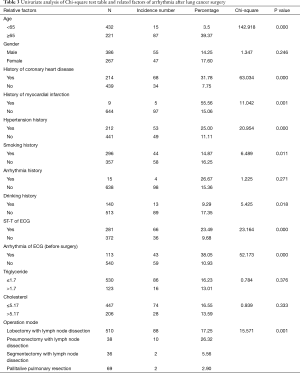
A total of 653 patients after surgery of lung cancer in our hospital were analyzed. Table 1 summarized the population characteristics of our study accompanied with lung infection. The relevant data of single factor Chi-square test analysis revealed that pulmonary infection after operation of lung cancer occurrence showed significant difference with ages (P<0.001), genders (P=0.012), lymphocyte counts (P=0.023), smoking histories (P<0.001), chronic respiratory diseases (P=0.023), FEV1/FVC (P=0.042), patients after drainage tube in dwelling time (P=0.024) and operation modes (P<0.001). Through logistic regression multivariate analysis, it was found that ages (P=0.022, 95% CI: 1.077–2.540), lymphocyte counts (P=0.017, 95% CI: 1.248–9.304), smoking histories (P<0.001, 95% CI: 1.665–3.691), histories of chronic bronchitis (P=0.007, 95% CI: 1.194–3.013), exudation time (P=0.011, 95% CI: 1.124–2.519) and operation modes (P<0.001, 95% CI: 1.836–3.078) remained significantly independent. Other factors were confirmed as false correlation (Table 2).

Full table

Full table
Arrhythmia
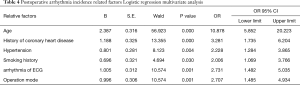
Table 3 summarized the population characteristics of our study accompanied with arrhythmia after lung cancer surgery. The relevant data of single factor χ2 test analysis revealed that pulmonary infection after operation of lung cancer occurrence showed significant difference with ages (P<0.001), histories of coronary heart disease (P<0.001), histories of myocardial infarction (P=0.001), hypertension histories (P<0.001), drinking histories (P=0.011), ST-T of electrocardiogram (ECG) (P<0.001), arrhythmia of ECG (P<0.001) and operation modes (P=0.001). Through logistic regression multivariate analysis, it was found that ages (P<0.001, 95% CI: 5.852–20.223), histories of coronary heart disease (P<0.001, 95% CI: 1.735–6.204), hypertension histories (P=0.004, 95% CI 1.284-3.865), smoking histories (P=0.030, 95% CI: 1.069–3.766), arrhythmia of ECG (P=0.001, 95% CI: 1.482–5.035) and operation modes (P=0.001, 95% CI: 1.485–4.934) remained significantly independent. Other factors were confirmed as false correlation (Table 4).
Full table
Full table
Predicting formula
Infection Rate= –0.4238687 – 0.0137439 × A + 0.0001784 × A2 + 0.0956266 × B + 0.1435408 × S – 0.0361227 × L+ 0.0011634 × L2 + 1.0366447 × O – 0.1924415 × O2
Arrhythmia Rate= –1.0859 + 0.0156 × A + 0.1147 × C + 0.0485 × H + 0.1027 × S + 0.1593 × AC + 0.0635 × O
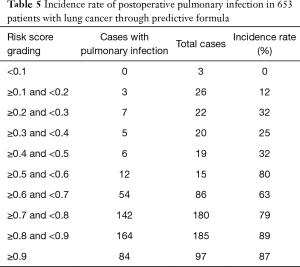
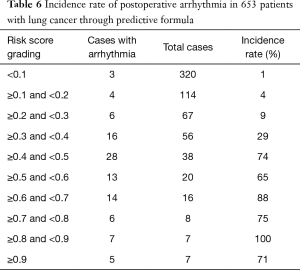
By this formula, where A was age, B was chronic bronchitis history, S was smoking history, L was Lymphocyte count, O was Operation mode, C was history of coronary heart disease, H was hypertension. and AC was arrhythmia of ECG, we could obtain the risk score for each patient. Then we calculated the occurrence probability of each patient to compared with the actual results. Table 5 summarized the data analysis of lung infection after lung surgery. Table 6 summarized the data analysis of arrhythmia. It was found that higher the risk scores, higher the complications incidence rates. We could observe that in Table 5 that scores more than 0.5 of the patients had a significantly higher risk. The lung infection risk rate of patients after surgery with scores more than 0.9 was 87%. The risk rate with scores 0.8–0.9 was 89%. On the other hand, the risk rate with scores less than 0.1 was 0. The similarly result could be obtained in patients with arrhythmia. The risk rate with scores more than 0.9 was 71%. The risk rate with scores 0.8-0.9 was 100%.
Full table
Full table
Discussion
Lung cancer is a common solid tumor of respiratory system. It is the most common cause of cancer death in men in the world, and is the second most common cause of death in women (6). Besides tumor recurrence and metastasis, postoperative complication was also a fatal factor for lung cancer patients. It is observed that lung cancer could be accompanied by immune abnormalities because of surgery and chemotherapy. And thoracic surgical trauma, long operative time and surgical resection of lung tissue may also lead to respiratory function insufficiency and caused complications related to heart and lung. It was reported that the incidence rate of pulmonary infections was 2.5%–25% (7-9). It is important to investigate the risk factors of postoperative complications for patient management. A systematic evaluation to predict the risk rate for patient before surgery is needed (10).
Our work showed that ages, lymphocyte counts, smoking histories, histories of chronic bronchitis, operation modes and postoperative extubation time were significantly associated with pulmonary infection. Schussler (9) determined that postoperative pneumonia after lung resection developed in 25% of patients, and others also have demonstrated that elderly patients tend to develop respiratory infections after thoracic surgery (11,12). It was demonstrated, by multivariate analysis, that lung cancer patients of advanced ages, in particular those 75 years of age and older, was a high-risk group for postoperative pneumonia (12). It might be related to the decline of body’s function and immune function of elder patients (13). The growth of beta-lactamase producing bacteria is particularly favoured in elderly people (14). Elder patients would be prone to get postoperative secondary infection.
Long-term history of smoking could impair the barrier function of respiratory epithelium and alveolar macrophages (15,16). Smoking could suppress the cilia activity, stimulate the glands secretion and tracheal spasm, and seriously destroy the ventilator function (17,18). Furthermore, the chest tube drainage was routinely placed after pulmonary resection for lung cancer. Patients with long time of indwelling pipe was prone to get retrograde infection. It was reported by Pimentel that S. agalactiae infections were mostly detected among patients who have used indwelling medical devices (77.2%) (19). Operation mode also would be an important factor of lung infection after surgery. Okada (20) reported that selective lymphadenectomy may be considered in elderly lung cancer patients. Our study also proved this viewpoint that larger wound of surgery would be easier to be infected.
Arrhythmia was also one of the main causes of death in patients with lung cancer during postoperative period, and it directly affected the postoperative recovery (21,22). It could be seen that the occurrence of arrhythmia after lung cancer surgery was influenced by a variety of factors, such as preoperative ECG abnormalities, advanced ages, and hypertension, operation modes. A report revealed age to be an independent risk factor for postoperative arrhythmia (23). In elderly lung cancer patients with postoperative complications, the incidence of arrhythmia was high (24,25). Our study confirmed that age was an independent risk factor. Cardiovascular disease history was also considered to be a high-risk factor for lung cancer surgery in postoperative correlation factors (26). The results of our study suggested that patients with a history of cardiovascular disease before surgery had a high rate of postoperative arrhythmia. Moreover, patients who had a long history of smoking might accompanied with a decreased pulmonary function, and smoking history would reduce the compensatory ability of cardiac pulmonary function after surgery and further increase the risk of arrhythmia (27). Also, pulmonary capillary bed reduction and insufficiency of pulmonary ventilation function after lung resection would result in decreasing of lung ventilation/perfusion ratio and increasing of pulmonary capillary blood flow (28). Cardiac function would also significantly be reduced (29). The above factors played important roles in the induction of arrhythmia. Heart and lung comorbidities treatments, heart function improvement, well-controlling of hypertension before operations would reduce the occurrence of heart complication. Respiratory tract cleaning during and after the procedure of surgery would be important for lung infection prevention. In addition, ECG monitoring and preventive treatment for arrhythmia would be helpful to reduce the risk of arrhythmia (30-32).
Our study finally obtained a formula to calculate the probability of complications occurrence for each patient after the operation, so that the risk quantization could be achieved. The formulas seemed to perform well for predicting the complications. The ability to predict which patient is at high risk for the cardiopulmonary complications may help to select patients who are appropriate for surgeries, advise preoperative interventions to decrease operative risks, and provide increased therapeutic measures to decrease the incidence of complications (4). Other scoring systems specific for lung resection have been reported, including the CPRI, the PRQ, and the PPP (33-35). Despite their potential utility, other scoring systems required the collection of large amounts of data and time-consuming calculations in order to generate a risk score for an individual patient. In our study, we investigated 653 cases and generated stratification of the scores, indicating that with increasing the score the likelihood of adverse outcome increases. It is beneficial to predict the risk of postoperative complications by collecting relevant medical histories. The practicality of the formula also needs to be further verified by prospective researches of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics committee of Tianjin Medical University Cancer Institute and Hospital (No. Ek2017088) and written informed consent was obtained from all patients.
References
- Siegs, 2014. CA Cancer J Clin 2014;64:9-29. [PubMed]
- Kelsey CR, Marks LB, Hollis D, et al. Local recurrence after surgery for early stage lung cancer: an 11-year experience with 975 patients. Cancer 2009;115:5218-27. [Crossref] [PubMed]
- Song IH, Yeom SW, Heo S, et al. Prognostic factors for post-recurrence survival in patients with completely resected Stage I non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:262-7. [Crossref] [PubMed]
- Ferguson MK, Durkin AE. A comparison of three scoring systems for predicting complications after major lung resection. Eur J Cardiothorac Surg 2003;23:35-42. [Crossref] [PubMed]
- el Hammami S, Djilani-Horchani H, Smati B, et al. Tunis Med 2001;79:617-20. [Immediate postoperative arrhythmias follwing pneumonectomy for lung cancer]. [PubMed]
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- Andalib A, Ramana-Kumar AV, Bartlett G, et al. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol 2013;8:554-61. [Crossref] [PubMed]
- Yamauchi Y, Isaka M, Maniwa T, et al. Chest tube tip culture as a predictor of postoperative infection in lung cancer operations. Ann Thorac Surg 2013;96:1796-802. [Crossref] [PubMed]
- Schussler O, Alifano M, Dermine H, et al. Postoperative pneumonia after major lung resection. Am J Respir Crit Care Med 2006;173:1161-9. [Crossref] [PubMed]
- Shiono S, Abiko M, Sato T. Postoperative complications in elderly patients after lung cancer surgery. Interact Cardiovasc Thorac Surg 2013;16:819-23. [Crossref] [PubMed]
- Iwamoto K, Ichiyama S, Shimokata K, et al. Postoperative pneumonia in elderly patients: incidence and mortality in comparison with younger patients. Intern Med 1993;32:274-7. [Crossref] [PubMed]
- Shiono S, Yoshida J, Nishimura M, et al. Risk factors of postoperative respiratory infections in lung cancer surgery. J Thorac Oncol 2007;2:34-8. [Crossref] [PubMed]
- Miura N, Kohno M, Ito K, et al. Lung cancer surgery in patients aged 80 years or older: an analysis of risk factors, morbidity, and mortality. Gen Thorac Cardiovasc Surg 2015;63:401-5. [Crossref] [PubMed]
- Sanguinetti CM, De Benedetto F, Miragliotta G. Bacterial agents of lower respiratory tract infections (LRTIs), beta-lactamase production, and resistance to antibiotics in elderly people. DEDALO Study Group. Int J Antimicrob Agents 2000;16:467-71. [Crossref] [PubMed]
- Li C, Zhihong H, Wenlong L, et al. The Nucleotide-Binding Oligomerization Domain-Like Receptor Family Pyrin Domain-Containing 3 Inflammasome Regulates Bronchial Epithelial Cell Injury and Proapoptosis after Exposure to Biomass Fuel Smoke. Am J Respir Cell Mol Biol 2016;55:815-24. [Crossref] [PubMed]
- Li L, Zhang M, Zhang L, et al. Klotho Regulates Cigarette Smoke-Induced Autophagy: Implication in Pathogenesis of COPD. Lung 2017;195:295-301. [Crossref] [PubMed]
- Iskandar AR, Mathis C, Schlage WK, et al. A systems toxicology approach for comparative assessment: Biological impact of an aerosol from a candidate modified-risk tobacco product and cigarette smoke on human organotypic bronchial epithelial cultures. Toxicol In Vitro 2017;39:29-51. [Crossref] [PubMed]
- Taylor RF, Bernard GR. Airway complications from free-basing cocaine. Chest 1989;95:476-7. [Crossref] [PubMed]
- Pimentel BA, Martins CA, Mendonca JC, et al. Streptococcus agalactiae infection in cancer patients: a five-year study. Eur J Clin Microbiol Infect Dis 2016;35:927-33. [Crossref] [PubMed]
- Okada M, Tsubota N, Yoshimura M, et al. Proposal for reasonable mediastinal lymphadenectomy in bronchogenic carcinomas: role of subcarinal nodes in selective dissection. J Thorac Cardiovasc Surg 1998;116:949-53. [Crossref] [PubMed]
- Amar D, Roistacher N, Rusch VW, et al. Effects of diltiazem prophylaxis on the incidence and clinical outcome of atrial arrhythmias after thoracic surgery. J Thorac Cardiovasc Surg 2000;120:790-8. [Crossref] [PubMed]
- von Knorring J, Lepantalo M, Lindgren L, et al. Cardiac arrhythmias and myocardial ischemia after thoracotomy for lung cancer. Ann Thorac Surg 1992;53:642-7. [Crossref] [PubMed]
- Asamura H, Naruke T, Tsuchiya R, et al. What are the risk factors for arrhythmias after thoracic operations? A retrospective multivariate analysis of 267 consecutive thoracic operations. J Thorac Cardiovasc Surg 1993;106:1104-10. [PubMed]
- Chkhikvadze VD, Sokolova VS, Lisitskii AN, et al. Khirurgiia (Mosk) 2003.15-6. [Results of surgical treatment of lung cancer in patients over 70 years old]. [PubMed]
- Annessi V, Paci M, Ricchetti T, et al. Is age over 70 years a risk factor for pneumonectomy? Asian Cardiovasc Thorac Ann 2009;17:272-7. [Crossref] [PubMed]
- Barbetakis N, Vassiliadis M. Is amiodarone a safe antiarrhythmic to use in supraventricular tachyarrhythmias after lung cancer surgery? BMC Surg 2004;4:7. [Crossref] [PubMed]
- Morice RC, Peters EJ, Ryan MB, et al. Exercise testing in the evaluation of patients at high risk for complications from lung resection. Chest 1992;101:356-61. [Crossref] [PubMed]
- Izquierdo JM, Pac JJ, Casanova J, et al. Arch Bronconeumol 1995;31:328-32. [Lung resection surgery in patients with functional limits]. [Crossref] [PubMed]
- Sumler ML, Andritsos MJ, Blank RS. Anesthetic management of the patient with dilated cardiomyopathy undergoing pulmonary resection surgery: a case-based discussion. Semin Cardiothorac Vasc Anesth 2013;17:9-27. [Crossref] [PubMed]
- Nair AS, Macherla G, Sahoo RK, et al. Electrocardiographic changes after lung resection: Case report and brief review. Anesth Essays Res 2015;9:263-5. [Crossref] [PubMed]
- Zhang L, Gao S. Systematic Review and Meta-analysis of Atrial Fibrillation Prophylaxis After Lung Surgery. J Cardiovasc Pharmacol 2016;67:351-7. [Crossref] [PubMed]
- Aoyama H, Otsuka Y, Aoyama Y. Landiolol infusion during general anesthesia does not prevent postoperative atrial fibrillation in patients undergoing lung resection. Gen Thorac Cardiovasc Surg 2016;64:735-41. [Crossref] [PubMed]
- Epstein SK, Faling LJ, Daly BD, et al. Predicting complications after pulmonary resection. Preoperative exercise testing vs a multifactorial cardiopulmonary risk index. Chest 1993;104:694-700. [Crossref] [PubMed]
- Pierce RJ, Copland JM, Sharpe K, et al. Preoperative risk evaluation for lung cancer resection: predicted postoperative product as a predictor of surgical mortality. Am J Respir Crit Care Med 1994;150:947-55. [Crossref] [PubMed]
- Melendez JA, Barrera R. Predictive respiratory complication quotient predicts pulmonary complications in thoracic surgical patients. Ann Thorac Surg 1998;66:220-4. [Crossref] [PubMed]


