Complete spontaneous resolution of a giant bulla without rupture or infection: a case report and literature review
Introduction
Bullous emphysema is a common obstructive pulmonary disease induced by tobacco smoke inhalation. Bulla is abnormal air collection within the lung parenchyma. It can cause some complications such as pneumothorax and superinfection. A giant bulla is a huge lesion occupying more than one third of the involved hemithorax. It can cause compressive atelectasis of the adjacent normal lung parenchyma (1). Usually the size of the bulla progressively increases over time and the patient can develop respiratory distress symptoms. The treatment of choice for a giant bulla is bullectomy (2). Spontaneous resolution of a giant bulla, termed autobullectomy, occurs very rarely (3). The mechanism of autobullectomy remains unclear. However, spontaneous regression of a bulla usually occurs in most cases after infection and rupture (4). Here we report a patient with recurrent pneumothorax who experienced complete resolution of a contralateral giant bulla without any subsequent infectious episode or rupture.
Case presentation
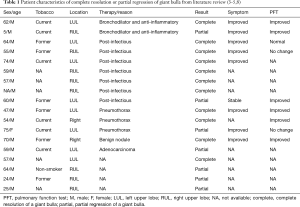
A 67-year-old male patient was transferred to our emergency room due to dyspnea. He had a history of hypertension. He was an ex-smoker. Chest X-ray revealed right spontaneous pneumothorax. Closed thoracostomy was performed. After expansion of the right lung, multiple large bullae were seen on chest computed tomography (Figure 1). Patient was discharged after removal of the chest tube drain at seven days after admission. There was no symptom or episode of recurrence of pneumothorax on regular follow up. After two years from the first attack of pneumothorax, the patient visited the outpatient department with a complaint of dyspnea. He stated that repeated right closed thoracostomy was performed at another hospital one month earlier. On chest computed tomography, the size of bullae had increased than that on the previous scan (Figure 2). The forced vital capacity (FVC) of the patient was 2,070 mL (58% of predicted capacity) with forced expiratory volume in 1 second (FEV1) of 1,490 mL (60% of predicted value). The FEV1/FVC ratio was 70% after the right closed thoracostomy. We planned two-stage bullectomy due to his impaired pulmonary function. The first operation was performed for recurrent spontaneous pneumothorax of the right side. Under general anesthesia, bullae on the apical and anterior segment of the right upper lobe were resected by thoracoscopic surgery. Chemical pleurodesis with talc powder was performed after bullectomy. The patient was discharged without any complication eight days after the operation. The patient did not have dyspnea, chest discomfort, or evidence of pneumothorax or superinfection of the large bulla on monthly follow up. Chest computed tomography was performed every six months. At one year after the operation, complete resolution of the giant bulla on superior segment of the left lower lobe was observed on chest computed tomography (Figure 3A,B). The patient denied any symptoms including dyspnea, chest pain or fever sensation during regular follow up period. After spontaneous resolution of a giant bulla of the left lung, his pulmonary function was improved (FVC of 3,150 mL, FEV1 of 2,120, above 90% of predicted value). The patient avoided the invasive bilateral surgery and achieved improvement of pulmonary function.

Discussion
A giant pulmonary bulla is defined as a pulmonary bulla occupying at least one third of the involved hemithorax. It typically occurs in the upper lobes. It is more frequent in men. Tobacco smoke inhalation is a leading cause of giant bullae (5). The mechanism causing enlargement of the bulla is currently unclear. The most widely known hypothesis is that the check valve of distal to terminal bronchioles might increase positive end-expiratory pressure and results in gradual expansion of bullae (6).
For giant emphysematous bullae cases, it remains controversial whether it is better to perform bullectomy at the same time for bilateral lungs or to perform two-stage bullectomy. Simultaneous bilateral surgery seems to be more invasive. It can trigger postoperative respiratory failure due to bilateral re-expansion edema especially for patient with impaired pulmonary function. Prolonged one lung ventilation for bilateral surgery can cause rupture of a giant bulla on contralateral lung. It can lead to potential life-threatening situations such as pneumothorax, pneumopericardium, hypoxemia, and death in spite of cardiopulmonary bypass (7).
Spontaneous reduction in size of a giant bulla occurs infrequently. Eleven cases of complete resolution and seven cases of partial regression of giant bullae have been reported in the English medical literature (Table 1).
Full table
The pathophysiology of spontaneous resolution or regression of giant bullae is not well understood yet. However, spontaneous regression and resolution of giant bullae can occur in most cases after an infectious process. Six patients had air-fluid levels within giant bullae and subsequent resolution of the bullae. Infection of the bullae might have caused airway inflammation and resulted in closure of communication between the airway and bullae. Obliteration of communication might have converted the bullae into a closed space. Air within the bullae might have been absorbed (8). Two patients have experienced complete resolution of giant bullae after spontaneous pneumothoraces. After rupture of bullae, intrapleural air was evacuated by closed thoracostomy. It resulted in re-expansion of the lung. The check valve mechanism in these patients might have facilitated healing of communication between the airway and bullae, finally resulting in resolution of ruptured giant bullae (9).
Pulmonary nodule is also associated with giant bullae. One patient with lung cancer has experienced partial regression of a giant bulla. Adenocarcinoma in the upper lobe of the left lung caused obstruction of the airway to a bulla. The size of the bulla was decreased. A benign nodule was also reported. It caused obliteration of communication between the airway and the bulla (10).
Some authors have reported spontaneous regression of giant bullae after cessation of smoking and intensive care with inhaled bronchodilator and anti-inflammatory medication. Tobacco smoke is a major irritant of the airway. It increases inflammation. Smoking cessation and anti-inflammatory medication could decrease airway inflammation and relieve check-valve pathophysiology of the airway, resulting in regression of bullae (5).
Our case is interesting because complete spontaneous resolution of a giant bulla is found. In addition, it is not associated with pneumothorax, overt infection, or tumor presumed as major causes of spontaneous resolution in the literature. The patient had not been treated with any medication including inhaled bronchodilator either resolution of a giant bulla might have re-expanded the compressed lung, thus improving symptoms.
Acknowledgements
This research was partially supported by Soonchunhyang University Research Fund.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Kayawake H, Chen F, Date H. Surgical resection of a giant emphysematous bulla occupying the entire hemithorax. Eur J Cardiothorac Surg 2013;43:e136-8. [Crossref] [PubMed]
- Kitazawa S, Saeki Y, Kikuchi S, et al. Surgical resection for bilateral giant emphysematous bullae. Clin Med Invest 2017;2:1-3. [Crossref]
- Wahbi ZK, Arnold AG. Spontaneous closure of a large emphysematous bulla. Respir Med 1995;89:377-9. [Crossref] [PubMed]
- Ridgeway NA, Ginn DR. Rupture and spontaneous resolution of a giant bulla with improvement in airways obstruction. Tenn Med 1998;91:431-2. [PubMed]
- Stone DJ, Schwartz A, Feltman JA. Bullous emphysema: A long-term study of the natural history and the effects of therapy. Am Rev Respir Dis 1960;94:493-507.
- Boushy SF, Kohen R, Billig DM, et al. Bullous emphysema: clinical, roentgenologic and physiologic study of 49 patients. Dis Chest 1968;54:327-34. [Crossref] [PubMed]
- Conacher ID. Anaesthesia for the surgery of emphysema. Br J Anaesth 1997;79:530-8. [Crossref] [PubMed]
- Byrd RP Jr, Roy TM. Spontaneous partial resolution of a giant pulmonary bulla. Austin J Pulm Respir Med 2014;1:1017-20.
- Millar EA. d'A Semple P. Spontaneous closure of a large emphysematous bulla. Respir Med 1996;90:120-1. [Crossref] [PubMed]
- Stern EJ, Webb WR, Weinacker A, et al. Idiopathic giant bullous emphysema (vanishing lung syndrome): imaging findings in nine patients. AJR Am J Roentgenol 1994;162:279-82. [Crossref] [PubMed]


