Robotic trans-subxiphoid extended thymectomy in a patient with thymoma-associated pemphigus
Introduction
Recently, the approach of trans-subxiphoid thymectomy has gained increasing attention as a treatment for myasthenia gravis and anterior mediastinal mass. In addition, robotic surgical systems have also been increasingly used in thymectomy. Herein, we report our surgical experience, and the outcome, of a 47-year-old man with thymoma-associated pemphigus (TAP). Notably, the condition of the patient improved to a significant extent because of an extended thymectomy during the follow-up period.
Case presentation
A 47-year-old male was putatively diagnosed with pemphigus vulgaris in outpatient department and admitted to the Department of Dermatology of our institution. He suffered from stomatitis including pharyngalgia (6 months ago), bullae on the tongue with pain (5 months ago), and cutaneous disorders including erythema and bullae on the trunk and anterior lower limbs with slight pruritus (3 months ago). The clinical diagnosis of pemphigus was confirmed by cutaneous biopsy specimens. The intravenous infusion of methylprednisolone sodium succinate was performed at a dose of 60 mg/day, then this was changed to an orally administered dose of 60 mg/day five days later.
To determine whether, or not, there was an underlying neoplasm, computed tomography (CT) of the chest, abdomen, and pelvis CT was performed and indicated the presence of an anterior mediastinal mass (1.3 cm × 1.9 cm), as shown in Figure 1. So, a TAP was suspected, and the chest CT scans also indicated slight pneumonia. Sputum culture showed mixed bacterial respiratory infections. Laboratory blood examination revealed: a procalcitonin level of 0.06 ng/ml, an albumin level of 27.5 g/L, a CRP of 19.20 mg/L, and IL-6 at 62.61 pg/mL. Intravenous levofloxacin (2 weeks, 500 mg/day), immunoglobulin (6 days, 15 g/day) were administered. The anti-BP-180 antibody increased consistent with the severity of the disease (135.51 to 158.54 µ/mL; norm <10 µ/mL). The anti-desmoglein 3 antibody titre was also elevated (167.17 µ/mL; norm <10 µ/mL), while it was normal in anti-desmoglein 1 antibody (7.37 µ/mL; norm <15 µ/mL).

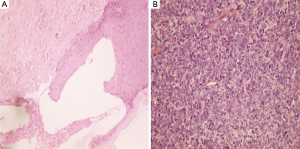
Preoperatively, a histological examination of cutaneous lesions showed acantholysis, as shown in Figure 2A. A robot-assisted trans-subxiphoid thoracoscopic extensive thymectomy was then performed. Postoperative intravenous levofloxacin (1 week, 500 mg/day), immunoglobulin (3 days, 20 g/day), and albumin (3 days, 10 g/day) were administered and the condition of the patient improved significantly by one week post-surgery. Both autoimmune antibodies showed significant decrease after thymectomy in parallel to clinical remission. The anti-BP-180 and anti-desmoglein 3 antibodies dropped to 90.58 and 161.08 µ/mL on postoperative day 6, respectively. The encapsulated tumour was diagnosed as a type-A thymoma according to the World Health Organisation (WHO) classification (Figure 2B). Soon after the thymectomy, the skin and oral mucosa conditions improved, especially for lesions on the trunk and lower-limbs, and no new mucocutaneous damage developed. On postoperative day 15, the patient began to take a soft oral diet, we therefore gradually lowered the prednisone dose to 40 mg/day to control the oral symptoms.
Surgical technique
An extended thymectomy was defined as the en bloc resection of the thymus and all adipose tissue anterior to both phrenic nerves. The present surgical procedure of robotic trans-subxiphoid extended thymectomy was similar to the technique performed by Suda et al. (1), as shown in Figure 3. After general anaesthesia with double-lung ventilation, the patient was placed in a supine position. A 2 cm-long longitudinal skin incision for camera insertion was created below the xiphoid process. Carbon dioxide was insufflated under a pressure of 8 mmHg through the subxiphoid camera access incision. Excellent operative space was achieved due to the trans-subxiphoid approach (Figure 4A). The lower section of the mediastinal pleura was detached from the back of the sternum. Two operation holes were then made below the bilateral costal arches. After dissection of the bilateral mediastinal pleura, the removal of the thymus and perithymic fatty tissue started at the pericardiophrenic angle, along the bilateral phrenic nerves, to the lower margin of the innominate vein. Thereafter, starting at the embouchement of the left internal mammary vein, the thymic gland was carefully separated from the underlying left innominate vein (Figure 4B). The dissection continued rightward to the conjunction of the innominate vein and superior vena cava. After exposure of the superior thymic horns, the upper thymic lobes and the perithymic adipose were resected caudally. When the resection was completed, the specimen was removed through the subxiphoid incision. A chest tube was inserted through one of the subcostal arch incisions.

Discussion
Paraneoplastic pemphigus (PNP) is a rare group of blistering autoimmune diseases resembling pemphigus vulgaris that affect the skin and mucous membranes. Some patients present with PNP in coexistence with other autoimmune diseases, such as myasthenia gravis and systemic lupus erythematosus. PNP patients usually present with polymorphous mucocutaneous lesions, including pruritus, cutaneous erythema and eruptions, large tense subepidermal bullae; symmetric skin lesions on abdomen, flexor forearms, medial thighs, lower legs, axillae, or groin; mild mucosal involvement of eyes, nose, oesophagus, pharynx, anus, or genitalia. Clinical manifestations usually start on the oral cavity mucosa with erosive stomatitis. Notably, the life-threatening respiratory complications possibly lead to dyspnea, bronchiolitis obliterans, sepsis, and a potentially high mortality rate (90%) without treatment, with respiratory failure being the main cause of death from TAP (2). Pulmonary injury may occur due to ectopic expression of epiplakin and desmoglein 3, which might represent possible targets for autoimmunity in bronchiolitis obliterans. In addition, pulmonary injury can increase the risk of respiratory infection (3).
The most commonly associated neoplasm in PNP is Castleman’s disease in China (77%) and hematological malignancies in European countries (74%), respectively (4). PNP is rarely associated with thymoma, either alone, or concomitantly with other autoimmune disorders. Of PNP patients, about 6% of them suffer from TAP. In previous reports, the majority of thymoma in patients with TAP were non-invasive and complete thymectomy was demonstrated as effective for this disease. A TAP patient reported by Zhang et al. (5) was successfully treated with complete removal of the thymoma after presenting with preoperative respiratory symptoms. Winkler et al. (6) published a case report about a patient with a rare triad of thymoma, myasthenia, and TAP. The patient reached the obvious clinical resolution of myasthenic and pemphigoid symptoms four months after thymectomy, without recurrence during the follow-up period. In addition, a recent case reported by Xie et al. (7) also showed a favourable outcome after thoracoscopic thymectomy for TAP. However, rare cases were exacerbated following operation. Another patient with a triad of thymoma, myasthenia, and TAP had markedly alleviated pemphigoid cutaneous lesions two months after operation, but developed myasthenic crisis and eventual respiratory failure, and died five months after operation (8). Interestingly, the patient did not suffer from mucosal involvement. In all, for patients suffering from solitary tumours associated with pemphigus, complete resection significantly reduces the risk of invasion of tumour and paraneoplastic disease. Recently, a 53-year-old man with TAP underwent an extended thymectomy with concomitant steroid treatment and then achieved complete recovery four years after operation (9).
Extended thymectomy is probably a favourable intervention in patients with TAP due to its poor response to medication alone. Compared with median sternotomy, a minimally invasive thymectomy is able to reduce the potential for pulmonary function injury, and the risk of pneumonia and respiratory failure (10). However, a unilateral approach cannot provide sufficient visualisation of bilateral upper thymus lobes and the contralateral phrenic nerve. Adequate anterior mediastinal adipose tissues dissection or invasive thymic tumour, or ectopic thymic, tissue may not be completely removed.
Trans-subxiphoid thoracoscopic thymectomy is documented as being able to provide excellent visualisation of the upper pole of the thymus and the bilateral phrenic nerves (1), so it becomes possible, using an extended thymectomy approach, that adequate bilateral mediastinal fatty tissue can be excised. Besides, the robotic surgical system (Intuitive Surgical, Inc., USA) provides considerable advantages over standard thoracoscopy, including articulating surgical instruments, the three-dimensional aspect, magnified operative images, and tremor filtration: it yields excellent surgical outcomes, such as completeness of resection and reduced risk of postoperative complication (11). Of note, one investigation verified that there is an improved neurological outcome for myasthenia gravis after robotic thoracoscopic thymectomy compared with thoracoscopic thymectomy (12). Therefore, robotic-assisted trans-subxiphoid thoracoscopic extended thymectomy seems an optimal technique for TAP. To our knowledge, this procedure has not been previously reported. In the present case, a robotic trans-subxiphoid extended thymectomy was successfully performed and the condition of the patient improved during the follow-up period.
Among improved TAP patients after thymectomy, postoperative disease durations varied, ranging from one year to four years (9,13). The course of the disease in this present patient was similar to that reported by Barbetakis et al. (13). In our case, after steroid treatment for four months, he received a robotic extended thymectomy. The postoperative period was eventful. Both positive autoimmune antibodies showed significant decreases one week after the thymectomy. The lesions on the trunk showed the better response to surgery than oral stomatitis. Cutaneous lesions achieved complete resolution one month after thymectomy without exacerbation at time of writing. He has received prednisolone treatment for his oral condition for four months.
Conclusions
In conclusion, robot-assisted thymectomy can be performed safely and efficiently in patients with TAP. Besides, according to the available literature and our clinical data, we can conclude that early robotic subxiphoid extended thymectomy, combined with other types of medical treatment, is an effective strategy for patients with TAP.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Suda T, Kaneda S, Hachimaru A, et al. Thymectomy via a subxiphoid approach: single-port and robot-assisted. J Thorac Dis 2016;8:S265-71. [PubMed]
- Nguyen VT, Ndoye A, Bassler KD, et al. Classification, clinical manifestations, and immunopathological mechanisms of the epithelial variant of paraneoplastic autoimmune multiorgan syndrome: a reappraisal of paraneoplastic pemphigus. Arch Dermatol 2001;137:193-206. [PubMed]
- Kartan S, Shi VY, Clark AK, et al. Paraneoplastic Pemphigus and Autoimmune Blistering Diseases Associated with Neoplasm: Characteristics, Diagnosis, Associated Neoplasms, Proposed Pathogenesis, Treatment. Am J Clin Dermatol 2017;18:105-26. [Crossref] [PubMed]
- Wang J, Zhu X, Li R, et al. Paraneoplastic pemphigus associated with Castleman tumor: a commonly reported subtype of paraneoplastic pemphigus in China. Arch Dermatol 2005;141:1285-93. [Crossref] [PubMed]
- Zhang J, Qiao QL, Chen XX, et al. Improved outcomes after complete resection of underlying tumors for patients with paraneoplastic pemphigus: a single-center experience of 22 cases. J Cancer Res Clin Oncol 2011;137:229-34. [Crossref] [PubMed]
- Winkler DT, Strnad P, Meier ML, et al. Myasthenia gravis, paraneoplastic pemphigus and thymoma, a rare triade. J Neurol 2007;254:1601-3. [Crossref] [PubMed]
- Xie A, Yan TD. Thoracoscopic thymectomy in a patient with pemphigus. Ann Cardiothorac Surg 2015;4:571-2. [PubMed]
- Lee SE, Hashimoto T, Kim SC. No mucosal involvement in a patient with paraneoplastic pemphigus associated with thymoma and myasthenia gravis. Br J Dermatol 2008;159:986-8. [Crossref] [PubMed]
- Yoshida M, Miyoshi T, Sakiyama S, et al. Pemphigus with thymoma improved by thymectomy: report of a case. Surg Today 2013;43:806-8. [Crossref] [PubMed]
- Weksler B, Tavares J, Newhook TE, et al. Robot-assisted thymectomy is superior to transsternal thymectomy. Surg Endosc 2012;26:261-6. [Crossref] [PubMed]
- Wei B, D'Amico TA. Thoracoscopic versus robotic approaches: advantages and disadvantages. Thorac Surg Clin 2014;24:177-88. vi. [Crossref] [PubMed]
- Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011;141:673-7. [Crossref] [PubMed]
- Barbetakis N, Samanidis G, Paliouras D, et al. Paraneoplastic pemphigus regression after thymoma resection. World J Surg Oncol 2008;6:83. [Crossref] [PubMed]



