Temporary bypass for superior vena cava reconstruction with Anthron bypass tubeTM
Introduction
The replacement or repair of a patient’s superior vena cava (SVC) can be challenging, as it requires the interruption of the upper body venous return, which could lead to life-threatening conditions if not appropriately managed. SVC clamping and repair may be required in the context of resections of non-small cell lung cancers (NSCLCs) or mediastinal tumors. The procedure of SVC clamping can cause an increase in cerebral venous pressure, a reduction in venous return, and a reduction in cardiac output. This can lead to hemodynamic deterioration, airway edema, and brain damage. Prior to replacement of the SVC, a temporary or permanent bypass from the left brachiocephalic vein to the atrium can be performed to avoid these issues. However, this strategy is not feasible in cases in which the brachiocephalic vein is completely implicated by the tumor. For these cases, a temporary bypass between the right brachiocephalic vein and right atrium can be used prior to SVC replacement. The present report describes a venous bypass technique using Anthron bypass tubeTM for total SVC clamping.
Case presentation
Equipment
Anthron bypass tubeTM (Toray Medical Co., Ltd., Tokyo, Japan), which is made of polyurethane coated with AnthronTM, was used in this procedure. There are two types of this catheter: straight and taper shaped. This catheter is designed and frequently used for surgeries involving portal vein resection or portal-venous bypass (1,2). Advantages include avoidance of the need for systematic anticoagulant drugs and easy access to vessels (3).
Surgical procedure
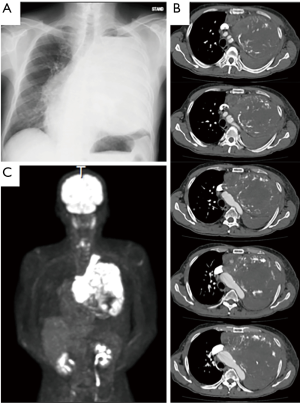
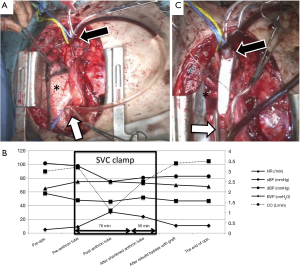
A 69-year-old man was referred to our department with a suspected mediastinal tumor. Chest x-ray and enhanced computed tomography showed a large tumor with involvement of the SVC, left brachiocephalic vein, pericardium and right upper lung lobe. In particular, the tumor invaded more than 50% of the SVC circumference and extended into the vessel lumen. The tumor occupied the left thoracic cavity and caused left lung atelectasis (Figure 1A,B). Positron emission tomography (PET) revealed strong uptake of fluorodeoxyglucose (FDG) in the tumor (Figure 1C). Underlying renal dysfunction was a contraindication to chemotherapy, and surgery was performed without biopsy. Median sternotomy was done with left cervical incision with cardiopulmonary bypass on standby in case of hemodynamic instability during operation. Although the large tumor occupied the entire left cavity, the left lung was not implicated in the tumor and remained inflated. However, the tumor had invaded the left brachiocephalic vein and extended into the peripheral left jugular vein and subclavian vein, thereby interfering with bypass between the left brachiocephalic vein and the right atrium that would otherwise have been used to reduce cerebral pressure prior to SVC replacement. Therefore, total SVC clamping was necessary during replacement by a synthetic graft. In this case, firstly, to avoid the initial drop in cardiac output intravenous volume expansion was performed and pharmacologic vasoconstrictors was used before ligation of the peripheral left jugular and subclavian veins. Secondly, the Anthron bypass tubeTM (VVT-51160) was chosen for bypass between the right brachiocephalic vein and the right atrium to reduce cerebral pressure (Figure 2A). Cerebral pressure was monitored by insertion of a catheter into the right brachiocephalic vein. As shown in Figure 2B, after total clamping of the SVC, hemodynamic status became unstable and systolic blood pressure dropped to 75 mmHg, cardiac output decreased to 1.1 L/min and brachiocephalic vein pressure increased up to 31 mmHg despite establishment of a bypass using the Anthron bypass tubeTM between the right brachiocephalic vein and the right atrium. The blood flow in the Anthron bypass tubeTM may not have been sufficient to maintain stable hemodynamics. This issue was solved by shortening the tapered Anthron bypass tubeTM by cutting it, which allowed the blood flow to increase. The adjustment of the length of Anthron bypass tubeTM by repeated clamping and de-clamping of the SVC required 76 minutes. Eventually, tumor resection combined with resection of the left brachiocephalic vein, SVC, pericardium and left phrenic nerve were performed in this case. The SVC was replaced with a 12-mm polytetrafluoroethylene graft with rings (Figure 2C) and the replacement of SVC required 56 minutes in total. The tumor was diagnosed as a sarcomatoid carcinoma originating from the thymus. There were some postoperative complications, which were atrial fibrillation and bilateral pleural effusion 23 days after the operation, however this was relieved by medication and drainage and the patient had no swelling of his extremities. The patient was discharged from the hospital 30 days after the operation. This patient was followed up, however, pulmonary metastasis was detected three months after the operation. Chemotherapy treatment was administered, however the patient died fifteen months after the operation due to tumor progression.
Discussion
The replacement or repair of a patient’s SVC is often required in cases of advanced mediastinal tumor or lung cancer (4). The standard procedure for replacement of the SVC is partial clamping of the SVC for direct repair or to establish a bypass between the left brachiocephalic vein and the right atrium before replacement of the SVC (5). In rare cases in which it is not possible to use the left brachiocephalic vein for bypass, SVC replacement with resection of the left brachiocephalic vein, using the Anthron bypass tubeTM as a temporary bypass provides an effective option for advanced tumors. SVC reconstruction has been performed safely in 45 minutes of total SVC clamping, however, it is difficult to predict the exact time of total SVC clamping (6). In this regard, a temporary bypass could be a useful tool to reduce risk. On the other hand, unilateral brachiocephalic ligation is acceptable and commonly performed in the thoracic surgery because ligation of the unilateral brachiocephalic vein is physiologically tolerated. However, usually we ligate left brachiocephalic vein only because unilateral left brachiocephalic vein reconstruction is not recommended because of the high thrombosis risk (7).
Anthron bypass tubeTM was designed for portal vein bypass, its inner and outer surfaces are coated with heparin. Therefore, systematic heparinization is not required when using the Anthron bypass tubeTM. This is helpful to reduce the risk of intraoperative bleeding, especially as resection of advanced tumors tends to result in more bleeding compared to other procedures. Another advantage is that the Anthron bypass tubeTM is easy to use, it simply requires insertion into the vessel with a purse-string suture.
In this case, the brachiocephalic vein pressure was measured, which approximates intracranial venous pressure. Immediately after insertion of the Anthron bypass tubeTM and total clamping of the SVC, the brachiocephalic vein pressure increased to approximately 40 mmHg, which is excessive for intracranial venous pressure. After cutting the edges of the Anthron bypass tubeTM, the pressure decreased to approximately 25 mmHg, which is a significant improvement but still relatively high. The Anthron bypass tubeTM was designed specifically for portal vein bypass, particularly to increase the blood flow in the portal veins [13.45±3.20 mL/min/kg (8), which is less than the SVC blood flow (16–17 mL/min, calculated as one-third of the venous return into right ventricle (50 mL/kg/min)] and flow velocity is about 35.2±7.3 mL/min during systole (9). 25 mmHg in the right brachiocephalic vein is sufficient to permit replacement of the SVC using a synthetic graft. Cutting the edges of the Anthron bypass tubeTM was effective towards increasing blood flow. Additionally, during this procedure, intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry was helpful for monitoring the incidence of cerebral damage (10).
As an alternative procedure, a Swan-Ganz sheath catheter has been used as a bypass between the right brachiocephalic vein and the femoral vein (11). This procedure prevented the occurrence of hemodynamic instability and upper body venous hypertension despite the required dose of noradrenaline increasing during the procedure.
As a last resort, if it is not possible to stabilize the hemodynamics using SVC clamping, cardiopulmonary bypass through the femoral artery and vein is possible. In this case, the SVC replacement using the Anthron bypass tubeTM was performed with the cardiopulmonary bypass procedure on standby. However, as cardiopulmonary bypass tends to cause adverse effects such as systemic inflammatory response, destruction of blood cells, numerous emboli and organ dysfunction (12), the SVC clamping using the Anthron bypass tubeTM could be considered prior to considering using a cardiopulmonary bypass.
SVC clamping may be a useful option for cases of advanced thoracic tumors invading the SVC and, in particular, for tumors invading the peripheral brachiocephalic vein. This procedure provides surgeons with sufficient time to complete replacement of SVC with a minimum of adverse effects.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nakao A, Nonami T, Harada A, et al. Portal vein resection with a new antithrombogenic catheter. Surgery 1990;108:913-8. [PubMed]
- Nakao A, Takagi H. Disseminated intravascular coagulation (DIC) in the intestinal circulation by acute portal vein occlusion and the effectiveness of portal-venous bypass using an antithrombogenic catheter. Hepatogastroenterology 1993;40:167-72. [PubMed]
- Nakao A, Kano T, Nonami T, et al. Application of an Antithrombogenic Anthron(R) Bypass Tube to Experimental Orthotopic Liver Transplantation: Studies on Blood Coagulation and Fibrinolysis. ASAIO Transactions 1986;32:503-7. [Crossref] [PubMed]
- Spaggiari L, Leo F, Veronesi G, et al. Superior vena cava resection for lung and mediastinal malignancies: a single-center experience with 70 cases. Ann Thorac Surg 2007;83:223-9; discussion 229-30. [Crossref] [PubMed]
- Garcia A, Flores RM. Surgical management of tumors invading the superior vena cava. Ann Thorac Surg 2008;85:2144-6. [Crossref] [PubMed]
- Dartevelle P, Macchiarini P, Chapelier A. Technique of superior vena cava resection and reconstruction. Chest Surg Clin N Am 1995;5:345-58. [PubMed]
- Shintani Y, Ohta M, Minami M, et al. Long-term graft patency after replacement of the brachiocephalic veins combined with resection of mediastinal tumors. J Thorac Cardiovasc Surg 2005;129:809-12. [Crossref] [PubMed]
- Brown HS, Halliwell M, Qamar M, et al. Measurement of normal portal venous blood flow by Doppler ultrasound. Gut 1989;30:503-9. [Crossref] [PubMed]
- Cohen ML, Cohen BS, Kronzon I, et al. Superior vena caval blood flow velocities in adults: a Doppler echocardiographic study. J Appl Physiol (1985) 1986;61:215-9. [PubMed]
- Goldman S, Sutter F, Ferdinand F, et al. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum 2004;7:E376-81. [Crossref] [PubMed]
- Perentes JY, Erling CC, Ris HB, et al. A simple bypass technique for superior vena cava reconstruction. Interact Cardiovasc Thorac Surg 2011;12:15-9. [Crossref] [PubMed]
- Murphy GJ, Angelini GD. Side effects of cardiopulmonary bypass: what is the reality? J Card Surg 2004;19:481-8. [Crossref] [PubMed]


