Outcomes of minimally invasive double valve surgery
Introduction
The benefits of minimally invasive valve surgery are well recognized when compared with a standard median sternotomy, in terms of reduced blood loss and less post-operative pain, and reductions in morbidity, hospital lengths of stay, and costs (1-4). Of all the potential benefits, an enhanced recovery with a faster return to normal activity is the most consistent finding (5). These advantages are seen particularly in high-risk populations, such as elderly and obese patients, and in those who undergoing re-operative valve surgery (6-12). However, data evaluating the feasibility and benefits of minimally invasive double valve surgery are limited (13-15). Our study aim was to analyze the outcomes of minimally invasive double valve surgery, performed via a right thoracotomy approach.
Methods
With Institutional Review Board approval, the institutional Society of Thoracic Surgeons database was retrospectively reviewed from January 2009 to December 2011, to identify patients who underwent minimally invasive repair or replacement of two simultaneous valves (double valve surgery). Excluded were patients in cardiogenic shock, those requiring emergency surgery, patients with prior valve surgery, or those who underwent concomitant cardiac surgical procedures such as coronary artery bypass grafting, surgery of the aorta, or triple valve surgery. We have previously published our results of patients undergoing combined mitral and tricuspid valve surgery, and some of those patients are included in this study (13).
All collected data were reviewed, including pertinent diagnostic testing prior to admission, operative reports, post-operative outcomes and discharge documentation. The total operative times, as well as the intensive care unit and postoperative length of stays were reviewed. The outcome variables evaluated were: prolonged mechanical ventilation (>24 hours), re-intubation, development of acute kidney injury, bleeding requiring re-operation, cerebrovascular accident, sepsis, post-operative atrial fibrillation, and in-hospital mortality.
Our approach to minimally invasive double valve surgery has been previously described in detail, and involves the utilization of a right thoracotomy (14). In summary, cardiopulmonary bypass was established utilizing a femoral platform. For combined aortic and mitral valve surgery, and for combined aortic and tricuspid procedures, a 6–7 cm incision was performed over the 4th intercostal space starting at the mid-clavicular line and extended laterally. For mitral and tricuspid valve surgery, the incision was made at the right 4th to 5th intercostal space, at the anterior axillary line. In the patients with prior coronary artery bypass grafting undergoing mitral and tricuspid valve surgery, moderate-to-deep hypothermia (24–26 °C) was utilized with fibrillatory arrest.
Statistical analysis
All variables are reported as the mean ±1 standard deviation (SD), median and interquartile range (IQR, 25–75%), or number (N) and percentage. The statistical software utilized for the analyses was the Statistical Package for Social Sciences, version 21 (SPSS Inc., Chicago, IL, USA).
Results
A total of 117 patients underwent double valve surgery during the study timeframe, consisting of 68 (58.1%) females and 49 (41.9%) males. The mean age and left ventricular ejection fraction were 73±11 years and 52±11%, respectively. Forty-three (36.8%) patients had congestive heart failure, 45 (38.5%) had chronic obstructive pulmonary disease, and 5 (4.3%) had a history of chronic kidney disease. There were 11 (9.4%) patients who had undergone prior coronary artery bypass graft surgery (Table 1). The types of surgery performed consisted of 50 (42.7%) aortic valve replacement and mitral valve repair, 31 (26.5%) mitral and tricuspid valve repair, 18 (15.4%) aortic and mitral valve replacement, 17 (14.5%) mitral valve replacement and tricuspid valve repair, and 1 (0.9%) aortic valve replacement and tricuspid valve repair. The median aortic cross-clamp and cardiopulmonary bypass times were 110 minutes (IQR 94–136), and 141 minutes (IQR 121–180) (Table 2).
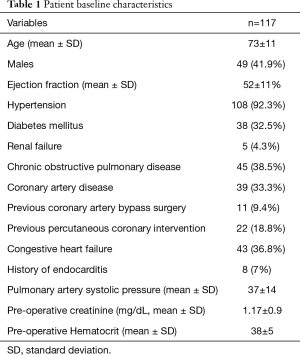
Full table
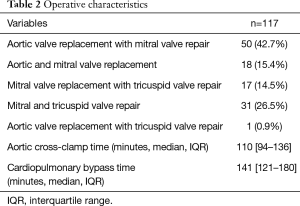
Full table
No patient required conversion to median sternotomy. Post-operatively, the median intensive care unit length of stay was 70 hours (IQR 46–135). There were 40 (34.2%) cases of prolonged mechanical ventilation, 9 (7.7%) cases of acute kidney injury, 6 (5.1%) re-operations for bleeding, 1 (0.9%) cerebrovascular accident, and 15 (12.8%) cases of atrial fibrillation. The mean total inpatient length of stay was 12±12 days, with an in-hospital mortality of 2 (1.7%) (Table 3).
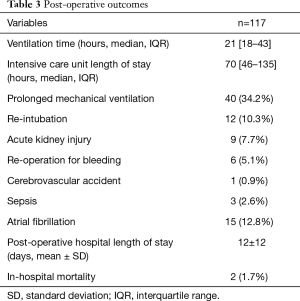
Full table
Discussion
Double valve surgery accounts for 10% of valve procedures performed in the United States (16). Patients requiring a multiple valve operation have an operative mortality that is more than twice that of single valve operations, which is cited at 9.7% for patients undergoing combined mitral and tricuspid valve surgery, 10.7% for those undergoing aortic and mitral valve surgery, and 13.2% for those underdoing aortic and tricuspid valve surgery (17). Since a minimally invasive approach has been shown to be associated with a decreased morbidity, shorter hospital lengths of stay, and an enhanced recovery with a faster return to normal activity when compared with median sternotomy valve operations, we hypothesized that higher-risk patients such as those undergoing double valve surgery may benefit from this approach (5,18).
The present study demonstrated an excellent in-hospital mortality of 1.7% utilizing a minimally invasive right thoracotomy in patients requiring double valve surgery. It also demonstrated acceptable outcomes in the incidence of post-operative cerebrovascular accidents, renal failure, and re-operation for bleeding. The most common post-operative complication noted was the incidence of prolonged mechanical ventilation, which occurred in 34% of the patients. This may be explained by the relatively high prevalence of chronic obstructive pulmonary disease in the cohort, as well as the timeframe in which the study took place. Following this institutional era, we implemented several changes in our post-cardiac surgery extubation practices, including standardized multidisciplinary ventilation weaning protocols. As a result, we observed a significant reduction in the length of mechanical ventilation and intensive care unit stay in subsequent analyses, in which a minimally invasive approach often proved superior to median sternotomy (6-9).
Some authors have expressed concern regarding the possibility of having lower repair rates of the mitral valve with minimally invasive valve surgery (19). This was not found to be an issue in the present study, as 80 (69%) of the 116 patients who underwent a mitral valve operation were able to have their mitral valve repaired. This repair rate of 69% is higher than the 57.4% reported by the Society of Thoracic Surgeons (20). This issue is important because mitral valve repair does not only demonstrate a lower mortality than replacement for isolated mitral valve surgery, but it is also associated with a lower mortality when performed in those undergoing multiple valve surgery, such as the cohort of the present study (21-23).
Another concern with minimally invasive valve surgery is obtaining adequate exposure, and this is especially true in patients undergoing double valve surgery and re-operative valve surgery. In circumstances where adequate exposure cannot be obtained, the minimally invasive surgery may need to be converted to a standard median sternotomy. Although data for double valve surgery are scarce, the conversion rate of minimally invasive surgery to median sternotomy is 1.0–4.0% during single valve operations (24,25). In the present study, even though 9.4% underwent re-operative surgery, adequate exposure was obtained in all patients, and none required conversion to a median sternotomy.
Data involving minimally invasive double valve surgery are somewhat limited. A propensity-matched analysis by Atik et al., compared the outcomes of 162 patients undergoing aortic and mitral valve surgery via a right thoracotomy (N=81) or conventional median sternotomy (N=81) (13). No difference was found in the outcomes of operative mortality (6.2% versus 2.5%, P=0.4), acute kidney injury (4.9% versus 1.2%, P=0.4), cerebrovascular accidents (2.5% versus 2.5%, P=1.0), or re-operation for bleeding (8.6% versus 4.9%, P=0.5). Survival at 10 years was also similar, being 82% and 76% for the minimally invasive and median sternotomy group, respectively (P=0.7). The authors concluded that minimally invasive surgery had cosmetic and blood product use advantages over conventional surgery, with no apparent detriments. Pfannmüller et al. reported their experience with 441 consecutive patients who underwent mitral and tricuspid valve surgery over a 10-year period, with the utilization of a right thoracotomy approach (14). Post-operative outcomes included 37 (8%) re-operations for bleeding, 10 (2%) cerebrovascular accidents, and 19 (4%) deaths at 30 days. The actuarial survival at 5 years was 77.2±2.5%. Finally, Mihos et al. evaluated the outcomes of 132 patients who had combined mitral and tricuspid valve surgery via a right thoracotomy, of which 12% underwent re-operative double valve surgery (15). Post-operative outcomes included 6 (5%) cases of acute kidney injury, 6 (5%) re-operations for bleeding, 4 (3%) cerebrovascular accidents, and 5 (4%) in-hospital deaths. The 1- and 5-year survival rates were 93% and 88%, respectively.
The current study is subject to the limitations inherent in a single center, retrospective design. Firstly, the study cohort is made up of a heterogeneous group of patients, with the results being limited to in-hospital outcomes. Secondly, the types of valve operations performed varied, and the etiologies of the valve dysfunction were not available. These are important factors that typically present in distinct demographic groups, and are associated with differing clinical and surgical risk profiles. What impact these variables may have had on the observed outcomes is unknown. Thirdly, there is no median sternotomy control group, which limits the conclusions that can be draw from the current data. Finally, all of the operations were performed via a right thoracotomy approach, and cannot be extrapolated to represent outcomes that may be obtained from other minimally invasive approaches. The results should be viewed as an observational study of a consecutive series of minimally invasive right thoracotomy double valve surgery, and as supportive of the hypothesis that this approach may be an alternative option to median sternotomy.
In summary, in patients requiring primary, or re-operative, double valve surgery, a minimally invasive right thoracotomy approach may be utilized with an acceptable peri-operative morbidity and mortality. It may be considered as a feasible alternative to the standard median sternotomy approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by the Institutional Review Board at the Mount Sinai Medical Center, Miami Beach, Florida, USA.
References
- Cohn LH, Adams DH, Couper GS, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Ann Surg 1997;226:421-6; discussion 427-8. [Crossref] [PubMed]
- Phan K, Xie A, Di Eusanio M, et al. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg 2014;98:1499-511. [Crossref] [PubMed]
- Cheng DC, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations (Phila) 2011;6:84-103. [Crossref] [PubMed]
- Santana O, Larrauri-Reyes M, Zamora C, et al. Is a minimally invasive approach for mitral valve surgery more cost-effective than median sternotomy? Interact Cardiovasc Thorac Surg 2016;22:97-100. [Crossref] [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol 2010;56:455-62. [Crossref] [PubMed]
- Lamelas J, Sarria A, Santana O, et al. Outcomes of minimally invasive valve surgery versus median sternotomy in patients age 75 years or greater. Ann Thorac Surg 2011;91:79-84. [Crossref] [PubMed]
- Santana O, Reyna J, Grana R, et al. Outcomes of minimally invasive valve surgery versus standard sternotomy in obese patients undergoing isolated valve surgery. Ann Thorac Surg 2011;91:406-10. [Crossref] [PubMed]
- Santana O, Reyna J, Benjo AM, et al. Outcomes of minimally invasive valve surgery in patients with chronic obstructive pulmonary disease. Eur J Cardiothorac Surg 2012;42:648-52. [Crossref] [PubMed]
- Mihos CG, Santana O, Lamas GA, et al. Outcomes of right minithoracotomy mitral valve surgery in patients with previous sternotomy. Ann Thorac Surg 2011;91:1824-7. [Crossref] [PubMed]
- Moscarelli M, Fattouch K, Casula R, et al. What Is the Role of Minimally Invasive Mitral Valve Surgery in High-Risk Patients? A Meta-Analysis of Observational Studies. Ann Thorac Surg 2016;101:981-9. [Crossref] [PubMed]
- Moscarelli M, Margaryan R, Cerillo A, et al. Minimally Invasive Mitral Valve Surgery in Truly High-Risk Patients: Are We Pushing the Boundaries?: An Observational Study. Innovations (Phila) 2015;10:328-33. [Crossref] [PubMed]
- Pineda AM, Santana O, Lamas GA, et al. Is a minimally invasive approach for re-operative aortic valve replacement superior to standard full resternotomy? Interact Cardiovasc Thorac Surg 2012;15:248-52. [Crossref] [PubMed]
- Atik FA, Svensson LG, Blackstone EH, et al. Less invasive versus conventional double-valve surgery: a propensity-matched comparison. J Thorac Cardiovasc Surg 2011;141:1461-8.e4. [Crossref] [PubMed]
- Pfannmüller B, Davierwala P, Hirnle G, et al. Concomitant tricuspid valve repair in patients with minimally invasive mitral valve surgery. Ann Cardiothorac Surg 2013;2:758-64. [PubMed]
- Mihos CG, Pineda AM, Davila H, et al. Combined Mitral and Tricuspid Valve Surgery Performed via a Right Minithoracotomy Approach. Innovations (Phila) 2015;10:304-8. [Crossref] [PubMed]
- Lee R, Li S, Rankin JS, et al. Fifteen-year outcome trends for valve surgery in North America. Ann Thorac Surg 2011;91:677-84; discussion p 684.
- Vassileva CM, Li S, Thourani VH, et al. Outcome characteristics of multiple-valve surgery: comparison with single-valve procedures. Innovations (Phila) 2014;9:27-32. [Crossref] [PubMed]
- Santana O, Xydas S, Williams RF, et al. Minimally invasive valve surgery in high-risk patients. J Thorac Dis 2017. [Epub ahead of print].
- Anyanwu AC, Adams DH. Should complex mitral valve repair be routinely performed using a minimally invasive approach? Curr Opin Cardiol 2012;27:118-24. [Crossref] [PubMed]
- Badhwar V, Rankin JS, He X, et al. The Society of Thoracic Surgeons Mitral Repair/Replacement Composite Score: A Report of The Society of Thoracic Surgeons Quality Measurement Task Force. Ann Thorac Surg 2016;101:2265-71. [Crossref] [PubMed]
- D'Agostino RS, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2017 Update on Outcomes and Quality. Ann Thorac Surg 2017;103:18-24. [Crossref] [PubMed]
- Rankin JS, He X, O'Brien SM, et al. The Society of Thoracic Surgeons risk model for operative mortality after multiple valve surgery. Ann Thorac Surg 2013;95:1484-90. [Crossref] [PubMed]
- Gillinov AM, Blackstone EH, Cosgrove DM 3rd, et al. Mitral valve repair with aortic valve replacement is superior to double valve replacement. J Thorac Cardiovasc Surg 2003;125:1372-87. [Crossref] [PubMed]
- Vollroth M, Seeburger J, Garbade J, et al. Minimally invasive mitral valve surgery is a very safe procedure with very low rates of conversion to full sternotomy. Eur J Cardiothorac Surg 2012;42:e13-5; discusson e16.
- Tabata M, Umakanthan R, Khalpey Z, et al. Conversion to full sternotomy during minimal-access cardiac surgery: reasons and results during a 9.5-year experience. J Thorac Cardiovasc Surg 2007;134:165-9. [Crossref] [PubMed]


