Intensive care unit and lung cancer: when should we intubate?
Introduction
Lung cancer still remains the leading cause of cancer death for males and the second most common cancer for females (1). There are currently several methods for lung cancer diagnosis such as the endobronchial ultrasound bronchoscopy, positron emission tomography and tissue biomarkers (2,3). Currently there also novel optical tools evaluated for rapid on site tissue specimen diagnosis (4). Novel treatments are also administered or are under development (5-13). However, early diagnosis and disease management are the cornerstone for efficient treatment (14,15). The current algorithm that is used for lung cancer patient treatment has prolonged the survival of these patients, including those not eligible for surgery (16). Therefore these patients present more often during their treatment complications attributed to the cancer disease or their treatment (17,18). The prolongation of patients not eligible for surgery reaches the 5 years in 16% of these patients (19). Treatment of lung cancer with radiation or tyrosine kinase inhibitors is also responsible for short term respiratory distress (20,21). Taken under consideration these factors and especially the advances in pharmacological treatment a larger number of patients are now eligible for admission in the intensive care unit (ICU) while before it was considered futile (22). There are currently novel non-invasive diagnostic and therapeutic techniques in the ICU making the short term admission of such a patient feasible (23). The ICU admission decision should be based on short-term and long-term outcome for the patient. The characteristics of the patients that would benefit from short-term or long-term are still not clarified. The ICU medical care is costly, burdensome and associated with increased risk (24). Until now the deterioration within the first 72 hours of the patient [measured with the logistic organ dysfunction score (LOD)] (25) has been identified as an early marker for worse survival and the use of vasopressors in combination with two-three organ system failures have been identified as a long term prediction factor for the intubated lung cancer patient (26). Moreover, other important factors identified to be negatively associated with survival where hemoptysis and acute respiratory failure upon admission. The mechanical ventilation and performance status (PS) ≥2 have been identified as independent factors indicating a worse prognosis for lung cancer patients (27). Furthermore, there is the subgroup of lung cancer patients which has been diagnosed and treated for a prolonged time and their disease related problems have been managed with different medications and non-invasive methods. Most importantly these patients have the time to decide how they want to be treated when their disease has progressed and the treatment options are no more efficient/availiable (28). We should also consider the fact that aggressive care in several situations does not provide the patient with the quality of life that deserves (29). Patient candidates for curative chemotherapy administration during ICU hospitalisation have not been yet identified. In the current review we will present published data for patients admitted in the ICU with two approaches: (I) patients admitted with known extensive disease or unknown however admitted (diagnosed upon admission); (II) patients with early stage lung cancer and (III) ICU as palliative care for lung cancer patients.
Search methods
We performed an electronic article search through PubMed, Google Scholar, Medscape, and Scopus databases, using combinations of the following keywords: ICU and lung cancer, ICU and cancer. All types of articles (randomized controlled trials, clinical observational cohort studies, review articles, case reports) were included. Selected references from identified articles were searched for further consideration, without language limitation.
Intensive care and lung cancer patients
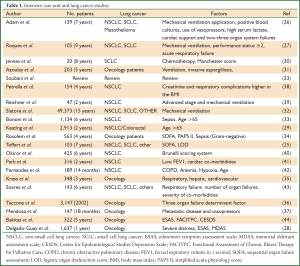
In the study by Adam et al. (26), 139 patients were included retrospectively. The mean age of the patients was 64.2 years [96 non-small cell lung cancer (NSCLC), 18 small cell lung cancer (SCLC) and 1 mesothelioma] and two evaluation scores were used: (I) acute physiology and chronic health evaluation III and (II) simplified acute physiology score (SAPS) III. The following data were recorded: (I) mechanical ventilation application; (II) positive blood cultures; (III) use of vasopressors; (IV) high serum lactate; (V) cardiac support and (VI) two-three organ system failures. The multivariate analysis demonstrated that the most important factors affected the final outcome (mortality) were the use of vasopressors and the presence of more than two organ failures. In another study by Roques et al. (27), 105 patients with mean age 64.8 years were included (87 NSCLC and 18 SCLC) and the following scores were used for patient assesment: (I) sequential organ failure assessment score (SOFA) and (II) SAPS II. Sixty-eight NSCLC patients had extensive stage disease (IIIB-IV). Only 30 patients after hospital discharge received chemotherapy treatment. The following factors were identified as prognostic: (I) mechanical ventilation and (II) PS ≥2 and (III) acute respiratory failure. The authors state that when PS ≤2 and the patient has stable disease then the outcome will be positive for the patient. However, stable disease in a patient with extensive disease is a combination that narrows the candidates and we should not forget that ICU hospitalisation triggers other mechanisms which can induce adverse effects such as, thrombosis. In the study by Toffart et al. (25) again Eastern Cooperative Oncology Group (ECOG)-PS <2 along with the LOD were established as prognostic factors for the outcome of these patients. In specific the reduction of LOD score within the first 72 hours of ICU admission was associated with severe outcome. The administration of chemotherapy in lung cancer patients was investigated as a prognostic factor in 20 SCLC patients (8 limited disease/12 extensive disease). The patients were evaluated with the adjusted Manchester score [0-4]. Five patients received chemotherapy while being intubated and 2 of them were free of tumour recurrence 7 months later. Patients who did not received chemotherapy died within 40 days. The patients administered chemotherapy were weaned-off early. A variety of chemotherapy agents were used and therefore no clear conclusions can be drawn which would be the best regimen for SCLC patients under these conditions. The Manchester score is a valuable tool for decision making for administering chemotherapy in patients admitted to the ICU and ICU admission (30). Moreover; other factors affecting lung cancer patients such as; infections, congestive heart failure and unidentifiable causes were assessed in a large study of 203 oncology patients (31). Mechanical ventilation was correlated with increased mortality (75.4%). The predictive factors were: (I) invasive aspergillosis; (II) unidentifiable diagnosis; (III) use of vasopressors; (IV) late initiation of mechanical ventilation; and (V) failure of non-invasive mechanical ventilation. Patients intubated due to with pulmonary oedema had the best prognosis and outcome. In the largest study including 49,373 lung cancer patients the mechanical ventilation was found to be the determinant factor affecting the outcome of these patients. Most patients were observed to die within 6 months of admission (32). In another large study with 1,134 older patients (>65) with extensive IIIB-IV stage NSCLC the following factors were recorded: sepsis, respiratory, cardiac, neurological and renal failure. Sepsis and >65 years of age were identified as the major prognosis factors. Survivors required multiple hospitalisations after ICU discharge and the 1 year mortality was observed to be 90% (33). Sepsis from gram-negative bacteria upon ICU admission has been also identified as a major factor for increased mortality among lung cancer patients in another large study of 563 patients (34). In the study by Kress et al. (35) with 348 patients included, the following factors were identified as predictive: (I) respiratory distress; (II) hepatic and (III) cardiovascular failure. Another large study comparing several types of cancers was carried out 2,009 including 3,147 patients (Sepsis Occurrence in Acutely Ill Patients-SOAP) (36). The determinant prognostic factor was the three organ failure. In the study by Mendoza et al. (37), 147 oncology patients were included and the most important factors affecting the prognosis of ICU admitted cancer patients were: (I) use of vasopressors and (II) metastatic disease (Table 1).
ICU and early stage lung cancer
Early stage lung cancer is another category of patients and a different mentality for ICU admission should be applied. In the study by Petrella et al. (38), an effort was made to identify the factors affecting the ICU admission outcome in surgically resected NSCLC patients. In specific the body mass index (BMI) was recorded and a cut off value of 25 kg/m2 was applied. Several other values such as, creatinine, forced expiratory value in 1 second (FEV1), Carbon Monoxide Diffusing Capacity (DLCO), histology and pathological stage, sex, cigarette history, preoperative albumin and total protein. The major results from this study indicate that the creatinine levels and the respiratory complications were 5.3 times higher in the BMI group >25 kg/m2. In the study by Okiror et al. (40), 425 patients were included with mean age 65 years. The respiratory functions were not identified as a prognostic marker for ICU outcome and the Brunelli score which was used, did not offer the expected results as an evaluation method for ICU outcome. In the study by Park et al. (41), 425 patients were included and the following factors were identified as prognostic postoperatively: (I) low FEV1 and cardiac co-morbidities. The type of surgery and the scoring systems (American Society of Anesthesiology, Charlson Co-morbidity Index) that were used were not identified as prognostic factors for the ICU outcome. Moreover in the study by Park et al. (41), two groups were identified: (I) early complications and (II) late complications. In the first group the major factors identified were the low expected FEV1 and the cardiac co-morbidity. In the second group the advanced age, low expected FEV1 and the cardiac co-morbidity were identified as prognostic factors. In the study by Fernandes et al. (42), 189 patients were included. The major factors identified as prognostic were: (I) anaemia; (II) age (≥65); (III) hypoxia and (IV) chronic obstructive pulmonary disease (COPD). In the SOAP study early lung cancer patients had increased rate of sepsis after surgery (36) (Table 1).
Full Table
ICU as palliative care for lung cancer patients
In an effort to identify the cancer patients that would benefit from palliative care intervention the ENABLE II study was conducted. The quality of life was measured with three scoring systems: (I) Center for Epidemiological Studies Depression Scale (CESDS); (II) Edmonton Symptom Assessment Scale (ESAS); and (III) Functional Assessment of Chronic Illness Therapy for Palliative Care (FACITPC). However, it was observed that palliative care intervention did not reduce the days of hospitalisation in the ICU or hospital wards and time in the emergency department (44). In another study by Delgado-Guay et al. (45), 1,637 oncology patients with median age of 60 years were included. The major findings were delirium, dyspnea, pain, fatigue and anxiety. The major pharmacologic and non-pharmacologic findings were: opioid management, steroids, antipsychotics and counselling. The patients were informed for withdrawal of mechanical ventilation, do not resuscitate conversion and withdrawal of bi-level-positive airway pressure. The two questionnaires used were the ESAS and Memorial Delirium Assessment Scale (MDAS). The pharmacological and non-pharmacological recommendations contributed in the quality of life of the patients and in several patients reduced the emotional distress (Table 1).
Discussion
Pulmonary physicians play a key role in the admission of lung cancer patients since they are also responsible for the ‘end of life’ decision making in several situations when the patient cannot be weaned-off the mechanical ventilation. The pulmonary physicians based on their expertise along with the anaesthesiologists are usually called to decide regarding the outcome of a lung cancer patient requiring intensive medical care. This is observed for patients with known lung cancer, while in the situation where a patient has not been yet diagnosed with lung cancer the decision is usually made by the internal medicine doctors (39). Older patients with extensive lung cancer usually receive less aggressive treatment in comparison to younger patients (<65 years) (29). Patients with lung cancer and pulmonary oedema should be intubated since positive outcome is expected, although the characteristics of these patients have not been clearly defined (disease stage and response) (31). We should state at this point that cardiovascular failure is a negative prognostic factor for early and extensive stage lung cancer patients and although it has previously stated that patients with pulmonary oedema should be intubated because of favourable outcome, we should firstly identify and clarify the characteristics of patients with coronary heart disease (35,41). The BMI >25 kg/m2 can be used as a predictive factor for early lung cancer patients admitted to the ICU (38). The low postoperative FEV1 can be also used as a predictive factor for early stage lung cancer patients admitted to the ICU (41). We should consider administering chemotherapy at least for SCLC which has a fast growth rate and the respiratory failure is due to obstruction from the lesion (endobronchial or intrathoracic pressure to the airways). The mechanical ventilation and not the cancer per se is the most important prognostic factor for lung cancer patients admitted to the ICU (43). Additionally, failure of more than 3 organs is attributed to 75% of mortality rate (36). Hepatic metastatic disease has the worse prognosis among other distant metastasis (35). The use of vasopressors and metastatic disease was also observed to affect the prognosis of the patients (37). Economical studies regarding these patients should be performed dividing them in patients with early lung cancer, patients >65 years and patients to treat based on the fact that they will benefit early from chemotherapy during their ICU hospitalisation (46). In the study by Au et al. (47), patient’s characteristics with COPD were compared with lung cancer patients. In specific a record was made with the two groups of patients regarding the cost of ICU admission. It was observed that the COPD patients visited their care providers several times more than the lung cancer patients for reasons other than their disease and when intubated their length of stay in the ICU was at least prolonged by 2 weeks. Also, the odds of a patient with COPD to be intubated are twice as much higher than a lung cancer patient. Therefore the cost of a patient with COPD is much higher. The COPD patients, however, were observed to receive less palliative care in comparison to lung cancer patients (47). These observations vary geographically and depend of the center’s experience that the patients are admitted for care (Table 2). We recommend based on the published literature that the LOD score is used as a predictive factor for extensive stage lung cancer patients (25) and the Manchester score when we want to administer chemotherapy in ICU admitted lung cancer patients (30). The early stage lung cancer patients can be probably identified as a separate group of patients and different evaluation factors for ICU admission should be applied. In specific pneumonectomy has been observed to induce postoperatively acute respiratory distress syndrome (ARDS) and patients which had a large pericardial effusion have been observed to develop acute cardiac decompensation (23). There are other situations that are related with cancer treatment; In specific radiation pneumonitis is an inflammatory process where the administration of corticosteroids can assist the respiratory function of the patient. The admission in the ICU could be considered for these patients mandatory, since it could provide them the time to recover and regain part of their respiratory capacity (20). Another treatment related situation is observed when several chemotherapeutic agents are administered. The following agents used in oncologic patients nowadays have been identified to induce ARDS; tyrosine kinase inhibitors, docetaxel, paclitaxel, etoposide, mitomycin, methotrexate and bevacizumab. The ARDS caused from these agents can be treated again with corticosteroids and in several situations admission in the ICU provides a window for these patients to regain their respiratory capacity. However, the identification of an infection from a pneumonitis in a neutropenic patient still remains a challenge for the clinician and we should have caution. Neutropenia on its own it is not a negative prognostic factor (36). There are data regarding NSCLC and SCLC patients admitted in the ICU, however, there are limited data regarding patients with mesothelioma. A future study presenting data regarding these patients would be most welcomed. Nutrition while ICU hospitalisation is a subject that has not been thoroughly investigated in correlation with lung cancer patients and whether it affects the outcome of these patients. Upon lung cancer diagnosis and specifically for extensive stage, the caregiver should discuss thoroughly with the patient the course of the disease and options. The patient and relatives should be aware of the complications and treatment management. Still there are no guidelines for lung cancer patient admission to the ICU and the burden for this decision is usually for the caregiver who provides the oncologic treatment to take. Future studies and committees should establish the criteria for ICU admission for lung cancer patients, taking into account also the quality of life of the patient.

Full Table
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ma J, Ward EM, Smith R, et al. Annual number of lung cancer deaths potentially avertable by screening in the United States. Cancer 2013;119:1381-5. [PubMed]
- Darwiche K, Freitag L, Nair A, et al. Evaluation of a novel endobronchial ultrasound-guided lymph node forceps in enlarged mediastinal lymph nodes. Respiration 2013;86:229-36. [PubMed]
- Darwiche K, Baumbach JI, Sommerwerck U, et al. Bronchoscopically obtained volatile biomarkers in lung cancer. Lung 2011;189:445-52. [PubMed]
- Fuchs FS, Zirlik S, Hildner K, et al. Confocal laser endomicroscopy for diagnosing lung cancer in vivo. Eur Respir J 2013;41:1401-8. [PubMed]
- Boutsikou E, Kontakiotis T, Zarogoulidis P, et al. Docetaxel-carboplatin in combination with erlotinib and/or bevacizumab in patients with non-small cell lung cancer. Onco Targets Ther 2013;6:125-34. [PubMed]
- Zarogoulidis K, Ziogas E, Boutsikou E, et al. Immunomodifiers in combination with conventional chemotherapy in small cell lung cancer: a phase II, randomized study. Drug Des Devel Ther 2013;7:611-7. [PubMed]
- Keam B, Kim DW, Park JH, et al. Rare and complex mutations of epidermal growth factor receptor, and efficacy of tyrosine kinase inhibitor in patients with non-small cell lung cancer. Int J Clin Oncol 2013. [Epub ahead of print]. [PubMed]
- Zarogoulidis K, Ziogas E, Papagiannis A, et al. Interferon alpha-2a and combined chemotherapy as first line treatment in SCLC patients: a randomized trial. Lung Cancer 1996;15:197-205. [PubMed]
- Zarogoulidis P, Chatzaki E, Hohenforst-Schmidt W, et al. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: a case series and literature review. Cancer Gene Ther 2012;19:593-600. [PubMed]
- Zarogoulidis P, Chatzaki E, Porpodis K, et al. Inhaled chemotherapy in lung cancer: future concept of nanomedicine. Int J Nanomedicine 2012;7:1551-72. [PubMed]
- Darwiche K, Zarogoulidis P, Karamanos NK, et al. Efficacy versus safety concerns for aerosol chemotherapy in non-small-cell lung cancer: a future dilemma for micro-oncology. Future Oncol 2013;9:505-25. [PubMed]
- Zarogoulidis P, Darwiche K, Hohenforst-Schmidt W, et al. Inhaled gene therapy in lung cancer: proof-of-concept for nano-oncology and nanobiotechnology in the management of lung cancer. Future Oncol 2013;9:1171-94. [PubMed]
- Zarogoulidis P, Eleftheriadou E, Sapardanis I, et al. Feasibility and effectiveness of inhaled carboplatin in NSCLC patients. Invest New Drugs 2012;30:1628-40. [PubMed]
- Szabo E, Mao JT, Lam S, et al. Chemoprevention of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e40S-60S.
- Zarogoulidis K, Latsios D, Porpodis K, et al. New dilemmas in small-cell lung cancer TNM clinical staging. Onco Targets Ther 2013;6:539-47. [PubMed]
- Reck M, von Pawel J, Zatloukal P, et al. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non-small-cell lung cancer: AVAil. J Clin Oncol 2009;27:1227-34. [PubMed]
- Barber NA, Ganti AK. Pulmonary toxicities from targeted therapies: a review. Target Oncol 2011;6:235-43. [PubMed]
- Crolow C, Samulowski M, Blum T, et al. Frequency of thromboembolic complications in patients with lung cancer. Pneumologie 2013;67:442-7. [PubMed]
- Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin 2009;59:225-49. [PubMed]
- Byhardt RW, Abrams R, Almagro U. The association of adult respiratory distress syndrome (ARDS) with thoracic irradiation (RT). Int J Radiat Oncol Biol Phys 1988;15:1441-6. [PubMed]
- Onal C, Abali H, Koc Z, et al. Radiation recall pneumonitis caused by erlotinib after palliative definitive radiotherapy. Onkologie 2012;35:191-4. [PubMed]
- Schapira DV, Studnicki J, Bradham DD, et al. Intensive care, survival, and expense of treating critically ill cancer patients. JAMA 1993;269:783-6. [PubMed]
- Soubani AO, Adam AK. Medical intensive care for lung cancer patients: better than we thought? Future Oncol 2008;4:141-4. [PubMed]
- Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med 2001;29:277-82. [PubMed]
- Toffart AC, Minet C, Raynard B, et al. Use of intensive care in patients with nonresectable lung cancer. Chest 2011;139:101-8. [PubMed]
- Adam AK, Soubani AO. Outcome and prognostic factors of lung cancer patients admitted to the medical intensive care unit. Eur Respir J 2008;31:47-53. [PubMed]
- Roques S, Parrot A, Lavole A, et al. Six-month prognosis of patients with lung cancer admitted to the intensive care unit. Intensive Care Med 2009;35:2044-50. [PubMed]
- Delgado-Guay M, Parsons HA, Li Z, et al. Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Support Care Cancer 2009;17:573-9. [PubMed]
- Keating NL, Landrum MB, Lamont EB, et al. End-of-life care for older cancer patients in the veterans health administration versus the private sector. Cancer 2010;116:3732-9. [PubMed]
- Jennens RR, Rosenthal MA, Mitchell P, et al. Outcome of patients admitted to the intensive care unit with newly diagnosed small cell lung cancer. Lung Cancer 2002;38:291-6. [PubMed]
- Azoulay E, Thiéry G, Chevret S, et al. The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 2004;83:360-70. [PubMed]
- Slatore CG, Cecere LM, Letourneau JL, et al. Intensive care unit outcomes among patients with lung cancer in the surveillance, epidemiology, and end results-medicare registry. J Clin Oncol 2012;30:1686-91. [PubMed]
- Bonomi MR, Smith CB, Mhango G, et al. Outcomes of elderly patients with stage IIIB-IV non-small cell lung cancer admitted to the intensive care unit. Lung Cancer 2012;77:600-4. [PubMed]
- Rosolem MM, Rabello LS, Lisboa T, et al. Critically ill patients with cancer and sepsis: clinical course and prognostic factors. J Crit Care 2012;27:301-7. [PubMed]
- Kress JP, Christenson J, Pohlman AS, et al. Outcomes of critically ill cancer patients in a university hospital setting. Am J Respir Crit Care Med 1999;160:1957-61. [PubMed]
- Taccone FS, Artigas AA, Sprung CL, et al. Characteristics and outcomes of cancer patients in European ICUs. Crit Care 2009;13:R15. [PubMed]
- Mendoza V, Lee A, Marik PE. The hospital-survival and prognostic factors of patients with solid tumors admitted to an ICU. Am J Hosp Palliat Care 2008;25:240-3. [PubMed]
- Petrella F, Radice D, Borri A, et al. The impact of preoperative body mass index on respiratory complications after pneumonectomy for non-small-cell lung cancer. Results from a series of 154 consecutive standard pneumonectomies. Eur J Cardiothorac Surg 2011;39:738-44. [PubMed]
- Reichner CA, Thompson JA, O’Brien S, et al. Outcome and code status of lung cancer patients admitted to the medical icu. Chest 2006;130:719-23. [PubMed]
- Okiror L, Patel N, Kho P, et al. Predicting risk of intensive care unit admission after resection for non-small cell lung cancer: a validation study. Interact Cardiovasc Thorac Surg 2012;14:31-3. [PubMed]
- Park SY, Park IK, Hwang Y, et al. Immediate postoperative care in the general thoracic ward is safe for low-risk patients after lobectomy for lung cancer. Korean J Thorac Cardiovasc Surg 2011;44:229-35. [PubMed]
- Fernandes EO, Teixeira C, Silva LC. Thoracic surgery: risk factors for postoperative complications of lung resection. Rev Assoc Med Bras 2011;57:292-8. [PubMed]
- Soares M, Darmon M, Salluh JI, et al. Prognosis of lung cancer patients with life-threatening complications. Chest 2007;131:840-6. [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the project enable ii randomized controlled trial. JAMA 2009;302:741-9. [PubMed]
- Parsons HA, Delgado-Guay MO, El Osta B, et al. Alcoholism screening in Patients with advanced cancer: impact on symptom burden and opioid use. J Palliat Med 2008;11:964-8. [PubMed]
- Leftakis A, Geitona M. Cost analysis and estimation of thoracic surgical patients with lung cancer in greece: the case of sotiria icu. Intensive Crit Care Nurs 2001;17:322-30. [PubMed]
- Au DH, Udris EM, Fihn SD, et al. Differences in health care utilization at the end of life among patients with chronic obstructive pulmonary disease and patients with lung cancer. Arch Intern Med 2006;166:326-31. [PubMed]


