Pulmonary mixed squamous cell and glandular papilloma mimicking adenocarcinoma: a case study and literature review
Introduction
The solitary pulmonary papillomas in adults are rare neoplasms, with about one hundred cases described to date in the English literature (1-9). In 1980, Spencer et al. first comprehensively summarized these kinds of neoplasms and named them non-invasive bronchial epithelial papillary tumors (1). In 1998, a classic review was made by Flieder et al. who subdivided solitary pulmonary papillomas into three separate categories: squamous cell papilloma, glandular papilloma and mixed squamous cell and glandular papilloma (mixed papilloma) (2). Flieder et al. also divided these neoplasms into central endobronchial type and peripheral bronchiolar type according to the location (2). Among the mentioned three types, mixed papilloma was the rarest one. Herein we report an additional case of mixed papilloma, which showed extension into adjacent bronchiolar and alveolar spaces mimicking adenocarcinoma. In the current study, we present some pathologic findings of the mixed papilloma in a 64-year-old Chinese female, and then carry out a thorough literature review.
Case report
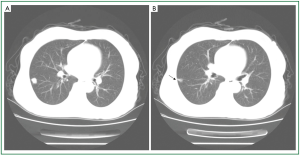
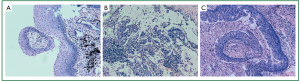
A 64-year-old female nonsmoker was admitted to our hospital because of chest pain without cough, hemoptysis, and other systemic symptoms. A chest CT scan revealed a peripheral solid nodule with a diameter of 13 mm in the lower lobe of the right lung (Figure 1A). The lesion did not present lobulated sign or spiculated sign, however, focal pleural indentation was observed (Figure 1B). From the CT scan, the diagnosis of lung cancer could not be excluded. Following wedge resection was performed. On gross examination, the tumor itself varied from grey to pale yellow. Microscopically, squamous and glandular epithelium could be observed, and in some area transitional epithelium like urothelium with morphology between the two kinds of epithelium was also present. Including transitional epithelium, all kinds of epithelium displayed papillary growth architectures (Figure 2A-C). The glandular epithelium consisted of non-ciliated columnar cells with eosinophilic cytoplasm and some mucin-filled cells (Figure 2B). In addition, the different epithelium showed no significant atypia, while some glandular tumor cells extended into adjacent bronchiolar and alveolar spaces with mucus which is similar to adenocarcinoma with lepidic-like pattern (Figure 2B). Further Immunohistochemical analysis showed these different components were diffusely positive for cytokeratin (CK) 7 (Figure 3A), CK19, CAM5.2, CK5/6 (the staining of the mucous cells were weak) (Figure 3B), and CK34βE12, but negative for CK20 or p16. The p63 staining showed immunoreactivity in the basal layer of glandular epithelium, and mostly in basal and parabasal layers of squamous and transitional epithelium. The different components were also positive for TTF-1, and in the squamous component, cells in the upper layers had weaker staining compared with that in the basal and parabasal layers (Figure 3C). The present case has been followed up for 24 months with no recurrence.

Discussion
Solitary pulmonary papillomas are rare tumors (1-3). The recent World Health Organization classification of lung tumors subdivides papillomas into three separate categories: squamous cell papilloma, glandular papilloma and mixed papilloma, of which mixed papilloma is the most extremely rare entity which accounted for 15.85% of all cases (3).
All mixed papillomas occurred in middle-aged and old people with a male preponderance (14 males and 5 females). Most patients are smokers, suggests smoking be a causative factor for that. Initial symptoms could be hemoptysis, syndromes of pneumonia or chest pain, but some cases was found by chance and showed no significant symptoms (1-7). Most cases were central endobronchial type arising from the wall of a stem bronchus or its major subdivisions (1-3,5-7). Of the 18 reported cases, only 3 were peripheral type which arose within the peripheral small bronchus (4,8,9). The present case is an additional case of peripheral mixed papilloma in the lung. HPV DNA was detected in most cases of squamous cell papilloma, indicating HPV may be a cause of that (2), however, HPV DNA has not been found yet in mixed papilloma and glandular papilloma of the lung (2,5-8,10). Although HPV ISH was not investigated in this case, the negative p16 staining indirectly suggests there is no existence of HPV.
Microscopically, the tumor was composed of squamous and glandular epithelium, and transitional urothelium-like morphology between the two kinds of epithelium was also present, which suggested the different kinds of epithelium come from the same origin. Some cases showed malignant transformation including focal squamous cell carcinoma in situ, adenocarcinoma (1-3) and spindle and squamous cell carcinoma (9). But it seemingly didn’t have influence to the favourable prognosis (1-3). In this case, the epithelium showed no significant atypia, however, some of its glandular tumor cells extended into adjacent bronchiolar and alveolar spaces with abundant mucus. This growth pattern could be confused with bronchoalveolar carcinoma or adenocarcinoma with papillary or micropapillary features. In fact, this morphology had been mentioned in a few cases of mixed papillomas (7,9) and glandular papillomas (10). We consider that different kinds of tumor cells lacking atypia can assist pathologists to make the correct diagnosis.
Interestingly, the immunohistochemical analysis showed these different kinds of epithelia had similar immunophenotype. Our findings were similar to that of Inamura et al. reported (7): all kinds of epithelia were diffusely positive for CK7, CK19, CAM5.2, CK5/6 (the staining of the mucous cells were weak) and CK34βE12, but negative for CK20. All kinds of epithelia were positive for TTF-1, which was strongly immunostained in the basal cells of squamous component, while became weaker as the maturity of squamous epithelium, and finally disappeared in the surface layer of the squamous epithelium. In consideration of aboving histological and immunohistochemical findings, we consider the tumor’s different components arise from the same kind of progenitor cells which can differentiate into different components, including glandular, squamous and urothelium-like epitheliums.
Herein, we reported a case of mixed papilloma in the lung. Since this tumor is extremely rare, the etiology and pathological characteristics are still unclear. In a few cases of mixed papilloma, glandular tumor cells can extend into bronchiolar and alveolar spaces with mucus, therefore, pathologists need to watch for it to avoid misdiagnosis. To our knowledge, recurrence has not been reported in mixed papilloma, and complete resection appears to be a curative treatment for this rare tumor.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Spencer H, Dail DH, Arneaud J. Non-invasive bronchial epithelial papillary tumors. Cancer 1980;45:1486-97. [PubMed]
- Flieder DB, Koss MN, Nicholson A, et al. Solitary pulmonary papillomas in adults: a clinicopathologic and in situ hybridization study of 14 cases combined with 27 cases in the literature. Am J Surg Pathol 1998;22:1328-42. [PubMed]
- Tryfon S, Dramba V, Zoglopitis F, et al. Solitary papillomas of the lower airways: epidemiological, clinical, and therapeutic data during a 22-year period and review of the literature. J Thorac Oncol 2012;7:643-8. [PubMed]
- Sung CO, Kim J, Do IG, et al. Solitary pulmonary mixed squamous cell and glandular papilloma: brief case report. Korean J Pathol 2008;42:393-5.
- Paganin F, Prevot M, Noel JB, et al. A solitary bronchial papilloma with unusual endoscopic presentation: case study and literature review. BMC Pulm Med 2009;9:40. [PubMed]
- Kadota K, Haba R, Katsuki N, et al. Cytological findings of mixed squamous cell and glandular papilloma in the lung. Diagn Cytopathol 2010;38:913-7. [PubMed]
- Inamura K, Kumasaka T, Furuta R, et al. Mixed squamous cell and glandular papilloma of the lung: a case study and literature review. Pathol Int 2011;61:252-8. [PubMed]
- Abiko T, Koizumi S, Takanami I, et al. 18F-FDG-PET/CT findings in primary pulmonary mixed squamous cell and glandular papilloma. Ann Nucl Med 2011;25:227-9. [PubMed]
- Lagana SM, Hanna RF, Borczuk AC. Pleomorphic (spindle and squamous cell) carcinoma arising in a peripheral mixed squamous and glandular papilloma in a 70-year-old man. Arch Pathol Lab Med 2011;135:1353-6. [PubMed]
- Aida S, Ohara I, Shimazaki H, et al. Solitary peripheral ciliated glandular papillomas of the lung: a report of 3 cases. Am J Surg Pathol 2008;32:1489-94. [PubMed]


