A tuberculous abscess of the chest wall in a renal allograft recipient
Introduction
Tuberculosis (TB) is a common cause of death among renal allograft recipients in developing countries (1-5). It is often presented with disseminated disease and extra pulmonary manifestations. Though T-cell immunosuppression advances the onset of TB, some patients showed late TB even under heavy immunosuppression therapy. However, tuberculous abscess of the chest wall without involvement of ribs is rare and usually manifests as part of disseminated disease in immunosuppressed individuals. It is still remained as a diagnostic and therapeutic challenge. In this article we report such a rare case of a renal allograft recipient.
Case
In 2013, a 40 year old male with chronic glomerulonephritis was admitted to our hospital with symptoms of persistent fever, weight loss and swelling over the back on the right side. There was no history of breathlessness, chest pain or hemoptysis. He received a renal allograft in 2000 with using prednisolone, cyclosporine and azathioprine without induction therapy. In 2011 he was diagnosed with acute type hematogenous disseminated pulmonary TB and endobronchial TB. Anti-tuberculous treatment including Isoniazid and Rifampicin had been administered for 15 months.
Examination showed moderately built and nourished male with weight of 70 kg, height of 183 cm, pulse rate of 110/min, blood pressure of 140/90 mmHg. There was no cervical lymphadenopathy. Local examination revealed a swelling in right side of the chest on posterior aspect in infrascapular region. The swelling measuring 15 cm × 12 cm in size was non tender, soft in consistency with no local rise of temperature. The swelling was also fluctuant and irreducible, had no cough impulse, and was situated in the subcutaneous plane. Respiratory system examination revealed dullness in left infra-axillary area with reduced intensity of breath sounds. Laboratory investigations revealed anemia (hemoglobin of 10.8 g/dL), a total leukocyte count of 4000/mm3, a normal platelet count and serum albumin of 3.0 g/dL. He had renal allograft dysfunction (serum creatinine of 43.7 mg/dL) with normal electrolyte profile and liver enzymes. Tuberculin skin test was negative.
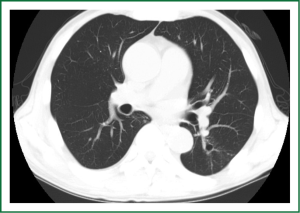
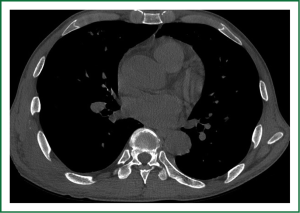
Computed tomography (CT) of the thorax showed stricture, narrowing and calcification in left lower lobar bronchus and uniform-sized small nodules randomly distributed throughout both lungs (Figure 1). The CT also showed a necrotic lesion located on the posterolateral aspect of the rib cage with a small nodular focus of calcification adjacent to the inner aspect. There is no evidence of bone erosion and no communication between the pleural cavity and the soft tissue swelling (Figure 2).
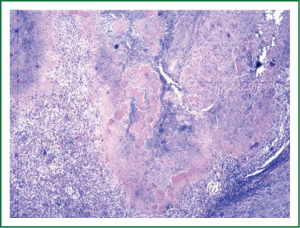
The patient underwent a complete excision of the abscess and primary closure of the wound (Figure 3). Histopathological examination of the abscess and nodule revealed fragments of extensive caseation necrosis and many acid-fast bacilli (AFB) (Figure 4). Sputum analysis didn’t reveal Acid Fast Bacilli in all samples.
Patient was administered with anti-Tuberculous therapy including Isoniazid, Rifampicin, Ethambutol and Pyrazinamide starting two weeks before operation and six months after operation. There was no incidence of postoperative wound infection and recurrence.
Discussion
The incidence rate of post-transplant tuberculosis (PTTB) in renal allograft recipients is between 0.3% to 1.7% in United States and Europe (1-3), but it is much higher in developing countries (3.1-15.2%) (1,4,5). One study shows in Southern China 51.8% of renal allograft recipients are diagnosed with extra pulmonary tuberculosis with a median interval of 8 months after renal transplantation (6). Among them, disseminated tuberculosis is the most common (19.3%), followed by pyrexia of unknown origin (15.7%), tuberculosis lymphadenopathy (4.8%), involvement of skin and soft tissue (4.2%), intestine (3%), central nervous system (1.8%), bone (1.2%), pericardium (1.2%) and urinary tract (0.6%) (4). T-cell immunosuppression favors dissemination of mycobacteria and varied presentation. However, tuberculous abscess of the chest wall is a rare form of extra pulmonary TB.
Timing of presentation of PTTB varies with types of immunosuppression. Cyclosporine advances the onset of PTTB from a median of 26 months (for patients on prednisolone and azathioprine regimen) to 11.5 months (4). But our patient presented PTTB 13 years after transplantation, even though being on cyclosporine. The presentation of tuberculous abscess of the chest wall is a progressively enlarging mass with or without pain. Sometimes abscess makes a fistulous tract to the pleural cavity and destroy underlying bone or cartilage. There are three mechanisms in the pathogenesis of a tuberculous abscess of the chest wall (7): (I) direct extension from the underlying pleural or pulmonary tuberculosis; (II) direct extension from lymphadenitis of the chest wall; and (III) hematogeneous dissemination from dormant tuberculous lesions. Regarding diagnosis, chest CT scan should be performed for every patient to examine the extent of abscess cavities and status of the ribs, sternum, cartilage and pleural space. CT scan can also provide information on functional state of the lung parenchyma, thoracic cavities and concomitant diseases and excludes other inflammatory or tumor lesions (8). Our patient’s chest CT showed features suggesting subacute type hematogenous disseminated pulmonary TB and endobronchial TB in the left lower lobe and also showed right side of the chest wall and the region inferior to right breast, which indicating cold abscess. There was no communication between the pleural cavity and the soft tissue swelling. But Cho et al. (9) found that multiple superficial locations of the abscess did not exclude the risk of rib involvement. These lesions are generally solitary, but in some patients multiple lesions were found. The diagnosis of tuberculous abscess of the chest wall remains difficult and is often diagnosed by postoperative pathologic examination. Many authors recommend needle aspiration or incisional biopsy to confirm the tuberculous disease or to exclude other inflammatory disease (7,10-12,). Cho et al. (9) recommended needle aspiration or biopsy preoperatively if the patient has no past history of TB and no concomitant active pulmonary lesions when CT scan showing poorly demarcated mass lesions. The gold standard remains characteristic histomorphological findings with demonstration of AFB and/or growth of MTB in culture (13).
The tuberculous abscess of the chest wall remains one of the differential diagnoses of a chest wall tumour, such as breast tumour in females (14), and the management strategy is controversial. On optimal therapeutic management, anti-tuberculosis medication may be very important. A few studies have reported successful treatment with anti-tuberculosis chemotherapy alone (10,15,16), but many authors have reported frequent recurrence after medication only (7,12). Hence, medical treatment alone is not sufficient for this disease. Many authors recommended a combination of medical and surgical management to reduce the recurrence, while Faure et al. (7) strongly suggested chemotherapy when tuberculous infection is confirmed or highly suspected but failed to improve with 1 to 3 months medication; if it worsens, surgical intervention is indicated. In our case, the patient was treated with preoperative anti-tuberculosis medication.
The methods of surgical treatment are also controversial. Weissberg (17) suggested treatment of antimicrobials and drainage, while debridement and excision are reserved for the most extensive cases. Paik et al. (18) documented a recurrence rate of 16% after abscess-only excision and 4.7% recurrence after complete resection of chest wall mass including any involved ribs. Kim et al. (19) also concluded that complete resection with or without skeletal resection achieved a low recurrence rate (9.2%). Recurrence was usually due to insufficient resection of involved ribs or infected pleura (20). We think that partial resection of the involved ribs is sufficient. In addition, curettage of infected pleural peel should be performed if necessary. Intraoperative evaluation of the extent of the abscess is important since preoperative imaging does not always show the involvement of the ribs or pleura. Regarding the risk of radical surgery, operative morbidity was reported to be about 5% (19).
Preoperative and postoperative drug therapy is mandatory to achieve acceptable cure rates (8,9). If the diagnosis of this disease is confirmed after radical surgery, a sufficient postoperative antitubercular therapy should be given. The duration of antituberculous therapy has been controversial, but a 6- to 9-month regimen including isoniazid and refampicin is considered standard (9,19,20). Thus, complete resection with sufficient antitubercular therapy is considered to offer a satisfactory cure rate with low recurrence. Our patient was administered with anti-Tuberculous therapy including Isoniazid, Rifampicin, Ethambutol and Pyrazinamide starting two weeks before operation and six months after operation. There was no incidence of postoperative wound infection and recurrence.
Conclusions
Disseminated TB manifesting with a tuberculous abscess of the chest wall with concomitant pulmonary tuberculosis is distinctly unusual in a renal transplant recipient. The diagnosis and management of PTTB can be complex and challenging. Chest CT scan is usually helpful method for showing the extent of the abscess and also provides information on the functional state of the lung parenchyma and thoracic cavities, and concomitant diseases, and excludes other inflammatory or tumor lesions. The optimal treatment approach consists of preoperative medication and excising the abscess, and complete surgical resection may be needed to keep the recurrence rate low. Adequate postoperative medication may reduce the chance of recurrence.
Acknowledgements
Disclosure: Signed consent is obtained from the patient for publication of this report and is available upon request. The authors declare no conflict of interest.
References
- Sakhuja V, Jha V, Varma PP, et al. The high incidence of tuberculosis among renal transplant recipients in India. Transplantation 1996;61:211-5. [PubMed]
- Jarrett O, Grim SA, Benedetti E, et al. Gastrointestinal tuberculosis in renal transplant recipients: case report and review of the literature. Transpl Infect Dis 2011;13:52-7. [PubMed]
- Yildiz A, Sever MS, Türkmen A, et al. Tuberculosis after renal transplantation: experience of one Turkish centre. Nephrol Dial Transplant 1998;13:1872-5. [PubMed]
- John GT, Shankar V, Abraham AM, et al. Risk factors for post-transplant tuberculosis. Kidney Int 2001;60:1148-53. [PubMed]
- Sayiner A, Ece T, Duman S, et al. Tuberculosis in renal transplant recipients. Transplantation 1999;68:1268-71. [PubMed]
- Chen SY, Wang CX, Chen LZ, et al. Tuberculosis in southern Chinese renal-transplant recipients. Clin Transplant 2008;22:780-4. [PubMed]
- Faure E, Souilamas R, Riquet M, et al. Cold abscess of the chest wall: a surgical entity? Ann Thorac Surg 1998;66:1174-8. [PubMed]
- Lee G, Im JG, Kim JS, et al. Tuberculosis of the ribs: CT appearance. J Comput Assist Tomogr 1993;17:363-6. [PubMed]
- Cho KD, Cho DG, Jo MS, et al. Current surgical therapy for patients with tuberculous abscess of the chest wall. Ann Thorac Surg 2006;81:1220-6. [PubMed]
- Hsu HS, Wang LS, Wu YC, et al. Management of primary chest wall tuberculosis. Scand J Thorac Cardiovasc Surg 1995;29:119-23. [PubMed]
- Kuzucu A, Soysal O, Günen H. The role of surgery in chest wall tuberculosis. Interact Cardiovasc Thorac Surg 2004;3:99-103. [PubMed]
- Sakuraba M, Sagara Y, Komatsu H. Surgical treatment of tuberculous abscess in the chest wall. Ann Thorac Surg 2005;79:964-7. [PubMed]
- Siu YP, Tong MK, Kwok YL, et al. An unusual case of both upper and lower gastrointestinal bleeding in a kidney transplant recipient. Transpl Infect Dis 2008;10:276-9. [PubMed]
- Eroğlu A, Kürkçüoglu C, Karaoglanoglu N, et al. Breast mass caused by rib tuberculous abscess. Eur J Cardiothorac Surg 2002;22:324-6. [PubMed]
- Chen CH, Shih JF, Wang LS, et al. Tuberculous subcutaneous abscess: an analysis of seven cases. Tuber Lung Dis 1996;77:184-7. [PubMed]
- Blunt SB, Harries MG. Discrete pleural masses without effusion in a young man: an unusual presentation of tuberculosis. Thorax 1989;44:436-7. [PubMed]
- Faure E, Souilamas R, Riquet M, et al. Cold abscess of the chest wall: a surgical entity? Ann Thorac Surg 1998;66:1174-8. [PubMed]
- Paik HC, Chung KY, Kang JH, et al. Surgical treatment of tuberculous cold abscess of the chest wall. Yonsei Med J 2002;43:309-14. [PubMed]
- Kim YT, Han KN, Kang CH, et al. Complete resection is mandatory for tubercular cold abscess of the chest wall. Ann Thorac Surg 2008;85:273-7. [PubMed]
- Kimura T, Funakoshi Y, Takeuchi Y, et al. Surgical treatment of tuberculous abscess of the chest wall: clinical analysis of 13 cases. The Journal of the Japanese Association for Chest Surgery 2010;24:134-9.



