Trans-aortic excision of intraventricular lipoma with the assistance of arthroscopic camera
Introduction
Primary cardiac tumors are rare, with an incidence of 0.2% to 0.4% in autopsy series (1,2). Around 75% of primary cardiac tumors are benign. Among them, 8% are represented by lipomas (2). Cardiac lipomas are encapsulated tumors, composed of mature fat cells. They are true neoplasms and should be differentiated from hypertrophic lipomatosis of the interatrial septum, in which there is deposition of non-encapsulated mature and fetal adipose tissue (3). Lipomas of the heart can be epimyocardial, intracavitary or intramyocardial and may be located in the atria or ventricles. Here, we reported a rare case of surgical resection of intracavitary lipoma located on the left side of the interventricular septum.
Case report
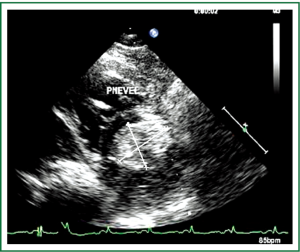
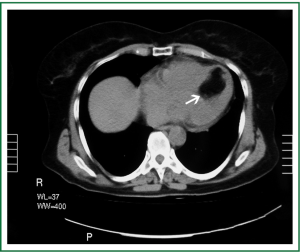
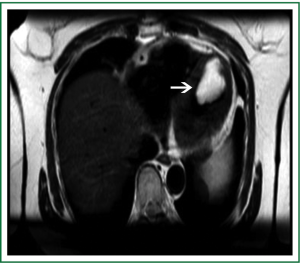
A 64-year-old female was referred to our institution complaining of dyspnea when exerting physical effort the last few years progressively worsening the last few months (NYHA III), palpitations and lower limb edema. Transthoracic (TTE) and Transesophageal (TEE) echocardiograms were performed and showed a hyperechoic mass with dimensions 50 mm × 70 mm on the left side of the interventricular septum (IVS), occupying almost ⅔ of the left ventricle (Figure 1). The left ventricle was mildly dilated with a normal systolic function and no significant obstacle observed to ventricular ejection. Computed Tomography (CT) of the chest, confirmed the existence of a hypodense mass, measuring 48 mm × 70 mm, affecting the topography of the interventricular septum with –92 IU Hounsfield (Figure 2). Magnetic Resonance Imaging (MRI) of the heart, confirmed the presence of a mass with irregular borders and defined limits, surrounded by a fibrous capsule, measuring 48 mm × 68 mm, located in the mid-basal portion of the interventricular septum (Figure 3). The radiographic signs were suggestive for lipoma or liposarcoma. Prior surgery a coronary angiogram was performed with normal findings.
Surgery was performed via median sternotomy and extracorporeal circulation with bicaval cannulation, mild hypothermia at 30 °C. Myocardial protection was established with infusion of cold Custodiol<sup>®</sup> HTK (Histidine-Tryptophan-Ketoglutarate) solution (Custodiol<sup>®</sup> Dr. Franz Kohler Chemie, Alsbach-Hahnlein, Germany) through the aortic root. A transverse incision was made over the aortic root, the cusps of the aortic valve were displaced and a 27-mm 0° Strycker<sup>®</sup> arthroscope was advanced into the ventricle through the aortic valve (Figure 4). The tumor was rising from the ventricular septum occupying the lower half of the ventricle. Although the macroscopic findings were in favor of lipoma, the result of the performed intra-operative frozen section was non-malignant speculating lipoma. Under direct vision the lipoma was totally resected and the ventricular cavity was rinsed and cleared with long laparoscopy forceps and continuous suction (Figure 5). The postoperative course was uneventful and the patient was discharged on the 6th postoperative day. Pathological examination confirmed the diagnosis of the tumor as lipoma.
Two years after the operation the patient is asymptomatic leading an active life. Consecutive TTEs performed during these two years of follow-up, were negative for recurrence.
Discussion
Lipomas of the heart are very rare tumors. Albers was responsible for the first report in 1856, and about 60 cases have been reported up until 1995 (4). It is also very rare to discover a cardiac tumor in the interventricular septum, which occurs in only 2% of cases (5). Therefore, the combination of a rare tumor (lipoma) with a rare location (interventricular septum) is particularly unusual (6-8).
An interventricular lipoma was first described and successfully removed by Bradford et al. (9). Surgical excision, whenever possible, is the treatment of choice for all primary cardiac tumors (10). Most patients with benign tumors are cured with resection and no recurrence afterwards. Palliative treatment may be used for malignant tumors, but adjuvant therapies are required to improve the patient’s prognoses (10). The great problem of the benign cardiac tumor does not reside in its histological characteristic, but in its intracavitary component, when the tumor invades cardiac cavities. The tumor becomes potentially lethal when it occupies the left ventricular cavity, as in our patient’s case, because it may alter the cardiac output, which is clinically indicated by syncope or may simulate left ventricular failure, peripheral embolism, and rhythm and conduction disorders (11). Therefore, surgery is mandatory after the determination of a diagnosis.
Lipomas occur at any age and the frequency is equal in both genders. Symptoms are not characteristic. The clinical manifestations of cardiac lipoma depend on its location and the possible resultant compression or obstruction. Usually they are asymptomatic and found accidentally. Arrhythmia, angina and syncope are some of the symptoms that a patient may complain. Our patient’s symptoms were those of heart failure with dyspnea and peripheral edemas. No evidence of stroke or embolus was recorded in her clinical history.
TTE is usually the initial diagnostic test for patients with a suspected cardiac mass or myocardial infiltration, due to its portability and availability. However, its sensitivity for differentiating tissue characteristics is limited. On the other hand, multislice CT allows for a characterization of the components within the mass. Low-attenuation features with a density similar to fat on CT are pathognomonic for lipoma, as in our case. Similarly, MRI also shows cardiac lipomas or lipomatous hypertrophy with characteristic low-signal-intensity margins and high-central-signal intensity on “bright-blood” balanced gradient-echo sequences (12).
Differential diagnosis is quite challenging. Pre-operative diagnosis includes cardiac tumors such as myxomas, lipomatous hypertrophy, fibromas, intracardiac varix (12,13).
The major surgical challenge and consideration when treating intracavitary lesions, is excision of the benign lesion from the left ventricle without injuring it, preservation of an adequate portion of the ventricular myocardium, maintenance of adequate atrioventricular valvular function and preservation, as much as possible, of the conduction system. Usually the full excision of the tumor is accomplished via left or right ventriculotomy, according to its location. Video-assisted removal of cardiac tumors, which avoids a left ventriculotomy, improves the lighting inside the surgical field that makes easier the vision of the remote part of the intracardiac anatomy, giving additional protection from possible injuries of surrounding structures and facilitating the completeness of the procedure has been reported (13). In our case, we choose to establish an opening and to perform the cardioscopy via the aortotomy, which helped us avoiding the ventriculotomy and enabled us to discern the precise extent of the tumor and rule out concomitant pathology. The use of arthroscope as an adjunct for excision of intraventricular abnormalities can assist in determining the precise location and size of tumors and in resecting tumors in areas of the heart that might otherwise be difficult to visualize. The full removal of the mass is suggested to be performed, in order to have a better visualization of the surgical margins.
This is a novel surgical approach for this kind of operation, and has proven to have great outcomes for the patient. The major benefits mostly stem from the fact that by avoiding a ventriculotomy, there is less damage to the cardiac muscle, reducing scarring, arrhythmias and blood loss. This approach results in reducing patient complications, the length of hospital stay and have a faster recovery. The above technique proved adequate because it allowed good technical management and good postoperative recovery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- McAllister HA Jr. Tumors of the heart and pericardium In: Silver. eds. Cardiovascular pathology. 2nd ed. New York: Churchill Livinstone, 1991:1297-333.
- Colucci WS, Schoen FJ, Braunwald E. Primary tumors of the heart. In: Braunwald E. eds. Heart disease: a textbook of cardiovascular medicine. vol. 2. Philadelphia: WB Saunders, 1997:1464-77.
- Alcocer JJ, Katz WE, Hattler BG. Surgical treatment of lipomatous hypertrophy of the interatrial septum. Ann Thorac Surg 1998;65:1784-6. [PubMed]
- Mullen JC, Schipper SA, Sett SS, et al. Right atrial lipoma. Ann Thorac Surg 1995;59:1239-41. [PubMed]
- Fernandes F, Soufen HN, Ianni BM, et al. Primary neoplasms of the heart. Clinical and histological presentation of 50 cases. Arq Bras Cardiol 2001;76:231-7. [PubMed]
- Nishi H, Mitsuno M, Ryomoto M, et al. Giant cardiac lipoma in the ventricular septum involving the tricuspid valve. Ann Thorac Surg 2009;88:1337-9. [PubMed]
- Ozaki N, Mukohara N, Yoshida M, et al. Cardiac lipoma in the ventricular septum--a case report. Thorac Cardiovasc Surg 2006;54:356-7. [PubMed]
- Kato Y, Murata H, Kitai K, et al. A case of cardiac lipoma in the ventricular septum. Jpn J Thorac Cardiovasc Surg 1998;46:1057-60. [PubMed]
- Bradford JH, Nomeir AM, Watts LE. Left ventricular lipoma: echocardiographic and angiographic features. South Med J 1980;73:663-5. [PubMed]
- Centofanti P, Di Rosa E, Deorsola L, et al. Primary cardiac tumors: early and late results of surgical treatment in 91 patients. Ann Thorac Surg 1999;68:1236-41. [PubMed]
- Hueb WA, Ramires JAF, Bellotti G, et al. Mixomas ventriculares e arritmias cardíacas: relato de 2 casos. Arq Bras Cardiol 1986;46:259-62. [PubMed]
- Zhang J, Chong E, Chai P, et al. Contrasting fatty involvement of the right ventricle: lipoma versus lipomatous hypertrophy. Singapore Med J 2009;50:e342-5. [PubMed]
- Araji OA, Gutierrez-Martin MA, Miranda N, et al. Video-assisted cardioscopy for removal of primary left ventricular fibroma. Interact Cardiovasc Thorac Surg 2010;10:344-5. [PubMed]




