Factors affecting satisfaction with education program for chronic airway disease in primary care settings
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are both chronic airway diseases. Treatment with inhalers is the central component to managing these diseases (1,2), therefore, adherence to prescribed inhaler therapy is the key to self-control of chronic airway diseases. Adherence to inhaled medication is significantly associated with a reduced risk of death and hospital admission due to exacerbation of COPD (3) Poor adherence to inhaled corticosteroids (ICS) is correlated with poor asthma-related outcomes. Less than perfect adherence to ICS appears to account for the majority of asthma-related hospitalizations (4,5). The reported adherence rate of COPD and asthma patients is about 50% and 30–70%, respectively (6-11).
In addition to the issue of adherence, the improper use of inhalers may decrease the effectiveness of the medication and, therefore, decrease the compliance. Inhaler mishandling is common in patients with chronic airflow obstruction and is linked to increased unscheduled health-care resource use and decreased disease control (12). The reported prevalence of incorrect inhalation technique varies from 4–94% (13-16).
The lack of adherence to the inhalers in COPD and asthma patients can be divided into two categories, namely unintentional non-adherence and intentional non-adherence (17). Patients showing unintentional non-adherence have a lack of information or a misunderstanding about the prescribed therapy, the correct technique for their prescribed aerosol device, and have language barriers or a combination of these aspects. Therefore, they are unaware that they do not adhere to the aerosol therapy and fail to understand the correct use of aerosol devices essential for the treatment of pulmonary diseases. In contrast, patients showing intentional non-adherence understand the importance of the prescribed therapy but reject the diagnosis, treatment, or both (18). Therefore, patient education programs should cover the knowledge about the disease in addition to proper inhaler technique to enhance the adherence to therapy in chronic airway disease patients. Patient education is one of the self-management intervention components emphasized by both the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) (1,2).
We previously reported that a well-organized education program improved patients’ knowledge about their disease, accurate inhaler technique and quality of life in both asthma and COPD patients in primary care clinics (19). In this study, we compared the outcomes of the education program in terms of its satisfaction between COPD and asthma patients. We also explored the differences in the extent of improvement of disease knowledge and inhaler technique between the two diseases.
Methods
Study design
The details of this study design have previously reported (19). Briefly, we enrolled 285 patients with physician-diagnosed asthma and COPD from 43 primary care clinics. Three educational visits were conducted at 2-week intervals. On the first visit, we conducted a patient knowledge assessment about their chronic airway disease and tested their inhaler use technique before the patients received the educational program. Thereafter, we conducted education about their disease and appropriate inhaler use and showed educational videos on these topics. On the second visit, the patients were taught an action plan for acute exacerbation and proper inhaler technique and received associated video education. On the final appointment, we summarized the educational elements covered in the first two visits.
Procedure
After three educational visits, we compared the quality of life, patient self-knowledge of the disease, change in inhaler technique and satisfaction with the education program, using a structured questionnaire before and after the education program. We asked three questions about disease knowledge and three questions about the importance of inhaler treatment. We also evaluated the satisfaction with the education program with three questions (Table S1). In this study, we categorized the patients into three groups according to the change in the three topics covered in the questionnaire. When the patients answered “somewhat or strongly agree” to all of the disease knowledge questions, we considered the subjects’ disease knowledge had improved. For the questions about inhaler knowledge, the same definition was applied. Similarly, when the subjects agreed somewhat or strongly to all the questions about the education program, they were considered as satisfied with the course (Table S1). Therefore, we could classify the subjects into four groups according to their improvement in disease knowledge and inhaler technique; improvement/non-improvement in disease knowledge with/without an improvement in inhaler knowledge. We compared the proportion of patients from each group regarding the questions about satisfaction with the education program between the COPD and asthma patients. We performed regression analysis to evaluate the association between their improvement in disease/inhaler knowledge and satisfaction with the education program and quality of life, as assessed by an asthma control test (ACT) or COPD assessment test (CAT). We also investigated the distribution of the change in knowledge and inhaler technique according to the disease.

Full table
Statistical methods
The results for each variable were shown as the mean with standard deviation, for the continuous variables; and the number of cases per category and frequency of responses, for the categorical variables. For the before and after education comparison concerning the quality of life, we used a paired t-test with the significance level set at 0.05. For the before and after education comparison regarding the degree of knowledge and inhaler usage, as assessed by a physician, the chi-square test was used. We also performed regression analysis to evaluate the association between the patient understanding of their disease and their satisfaction with the education program and their quality of life. We used SPSS 21.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis.
Ethics statement
The study protocol was reviewed and approved by the Inje University Institutional Review Board (# IIT-2014-283). A written informed consent, describing the purpose of the study was signed by all of the participants.
Results
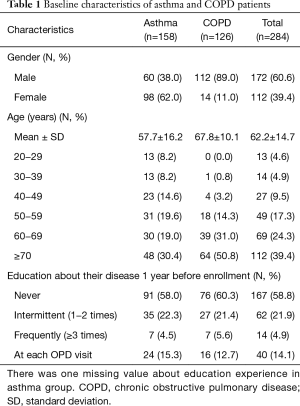
A total of 285 patients were enrolled in this study. There were 158 asthma patients and 127 COPD patients. One COPD patient did not answer the questions about satisfaction, and consequently, 284 patients were included in this study. The mean age was 62.2±14.7 years. A total of 58.5% patients had not taken an education program in the year before enrollment (19) (Table 1).
Full table
Satisfaction with education program
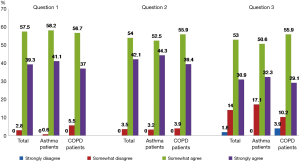
When we asked the patients whether they were satisfied with the education program, they answered differently to each question. For question 1 & 2 (Table S1), only 2.8 and 3.5% of the patients provided a negative answer, respectively. However, for question 3, which asked the willingness to pay an additional cost for the education program, 15.8%responded with a negative answer. Figure 1 shows the proportion of the COPD and asthma patients, respectively, for each response to the three questions regarding their satisfaction with the education program.
Distribution of patients according to their change in knowledge after the education program
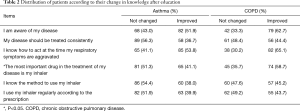
A knowledge improvement was observed after three education sessions (19). Hence, we compared the change in patient knowledge about their disease and their inhaler technique after education between the COPD and asthma subjects. The distribution of the patients who showed an improvement in their knowledge was similar between asthma and COPD subjects. More COPD patients showed an improvement for “the most important drug in the treatment of my disease is my inhaler” than asthma patients (Table 2).
Full table
Improvement of inhaler technique
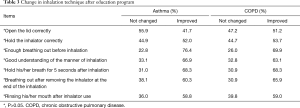
After the education program, the proportion of patients with good inhalation technique increased significantly in both asthma and COPD subjects at all stages of inhaler use. However, there was no statistical significance regarding the number of COPD or asthma patients who showed an improved inhalation technique after education (Table 3).
Full table
Satisfaction with education program according to the change in disease knowledge and inhaler technique
We compared the change in disease and inhaler knowledge, according to satisfaction with the education program. There was no statistical significance found for questions 1 and 2 about satisfaction with the education program. For question 3, 45 patients showed a negative answer. Among these patients, 42 (93.3%) did not improve their inhaler knowledge after the education program. This figure was higher than that obtained for the patients who were satisfied with the education program (P<0.001).
We further compared the proportion of the patients for the questions about satisfaction with the education program according to the status of knowledge concerning their disease. The patients with improved knowledge about both their disease and inhaler use were satisfied with the education program. About 60% of the patients whose knowledge did not improve, were also satisfied with the program. However, more patients, particularly those with asthma, disagreed with question 3, which asked about the willingness to pay an additional cost for the education program (Table 4).
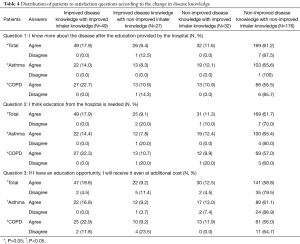
Full table
We performed regression analysis to evaluate the association between patient knowledge improvement and satisfaction with the education program. Overall, we found that knowledge improvement was associated with satisfaction with the education program in both asthma and COPD patients. However, we did not find any significant relation between knowledge improvement and quality of life (Table 5).

Full table
Discussion
In this study, we found that both asthma and COPD patients were satisfied with the education program. For asthma patients, 99.3% of the test subjects somewhat or strongly thought that they knew more about the disease after education and 96.8% somewhat or strongly agreed that education from the hospital is needed. For COPD patients, 94.8% of the test subjects somewhat or strongly thought that they knew more about the disease after education and 95.7% somewhat or strongly agreed that education from the hospital is needed. Interestingly, the proportion of the patients who answered negatively to the question about willingness to pay an additional cost for the education program was higher compared to the other questions. Thus, personal finance is the barrier to enhancing therapy adherence in patients with chronic airway disease. A policy to reduce the economic burden of the patients should be considered.
Our education program improved both disease and inhaler knowledge in the patients (19). We did not find any significant difference between asthma and COPD patients, except one question about the importance of inhaler use for treatment of chronic airway disease. The COPD patients became more aware of this question after receiving the education program (Table 2). Although the proportion of patients showing the correct inhaler use at each step were improved after the education program (19), there was no significant difference observed between asthma and COPD patients (Table 3). Considering that about 60% of the patients had not previously received any education program and had poor awareness of COPD (20-22), this finding suggests increased awareness of COPD in conjunction with the education program is needed.
We investigated patient satisfaction with the education program according to the improvement in disease and inhaler knowledge. Most patients agreed with the satisfaction questions 1 and 2, even though their knowledge did not improve. This finding was consistent when we analyzed asthma and COPD patients separately. However, for question 3, which dealt with cost, significantly more patients answered negatively. Among the asthma patients with neither an improvement in disease nor inhaler knowledge, 23.1% did not agree with the idea of paying an additional cost. This finding reinforced the necessity of a policy to reduce the economic burden of the patients. In comparison, for COPD patients, the proportions were not significantly different according to the change in knowledge (Table 3). We thought that the poor awareness of COPD in the general population was one possible explanation for this finding (20,21,22). A strategy to increase awareness of COPD is recommended. Collaboration with patient organization to give an education about COPD can be a mean to increase awareness, for example. Since patient organization have many activities in patient education, training, information and awareness (23).
Table 5 shows a weak but positive association between knowledge improvement and patient satisfaction with the education program. As our study duration was relatively short, we thought that this correlation could be evident if the study duration had been extended. Our education program significantly improved the quality of life for asthma and COPD patients (19). However, this improvement was not associated with the improvement in disease and inhaler knowledge. About half of the patients met the minimum clinical important difference (MCID) for both the ACT and CAT, indicating that the short duration of our study might be one possible explanation for this finding.
The strength of this study was addressed previously (19). We included both asthma and COPD patients, which made it possible to perform post hoc analysis. All the patients were recruited from primary care clinics and received the education program at the same location. This reflected the real life situation that could generalize the results.
This study had some limitations. First, as we used physician-diagnosed definitions for enrollment, it is possible that strict separation into the COPD and asthma patients has not been achieved. Hence, the comparisons made between both diseases might be reduced. However, we think that the results reflect the real life situation in Korea and did not reduce the necessity or importance of the education program. An additional limitation of our experiment was its short duration as mentioned above. We were unable to perform a follow-up study to evaluate the long-term effects of patient education on quality of life. However, we are planning a prospective study using medical insurance claim data to explore the effect of the education program regarding health care utilization as we did for early COPD patients (24).
Conclusions
After a 1-month education program with three visits in a primary care setting, most asthma and COPD patients were satisfied with the program, even though their knowledge about the disease and inhaler did not improve. The patients knew a lot about their disease after the education and agreed that education from the hospital is needed. The knowledge improvement was associated with satisfaction with the education program in both asthma and COPD patients. However, more patients, particularly those with asthma, disagreed to paying an additional fee to receive the education program. As patient education is one of the self-management intervention components in asthma and COPD patients (1,2), a policy to reduce the economic burden on the patients should be considered to disseminate an education program in primary care clinics.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was reviewed and approved by the Inje University Institutional Review Board (# IIT-2014-283). A written informed consent, describing the purpose of the study was signed by all of the participants.
References
- The Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet]. Available online: (Accessed 19 August 2016).http://www.ginasthma.com
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [Internet]. Available online: (Accessed 21 August 2016).http://www.goldcopd.org
- Vestbo J, Anderson JA, Calverley PM, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax 2009;64:939-43. [PubMed]
- Williams LK, Pladevall M, Xi H, et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol 2004;114:1288-93. [PubMed]
- Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105:930-8. [PubMed]
- Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol 2006;118:899-904. [PubMed]
- Haupt D, Krigsman K, Nilsson JL. Medication persistence among patients with asthma/COPD drugs. Pharm World Sci 2008;30:509-14. [PubMed]
- Krigsman K, Moen J, Nilsson JL, et al. Refill adherence by the elderly for asthma/chronic obstructive pulmonary disease drugs dispensed over a 10-year period. J Clin Pharm Ther 2007;32:603-11. [PubMed]
- Krigsman K, Nilsson JL, Ring L. Adherence to multiple drug therapies: refill adherence to concomitant use of diabetes and asthma/COPD medication. Pharmacoepidemiol Drug Saf 2007;16:1120-8. [PubMed]
- Krigsman K, Nilsson JL, Ring L. Refill adherence for patients with asthma and COPD: comparison of a pharmacy record database with manually collected repeat prescriptions. Pharmacoepidemiol Drug Saf 2007;16:441-8. [PubMed]
- World Health Organization. Adherence to long-term therapies: evidence for action 2003 [Internet]. Available online: (Accessed 23 August 2016).http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf
- Milgrom H, Wamboldt F, Bender B. Monitoring adherence to the therapy of asthma. Curr Opin Allergy Clin Immunol 2002;2:201-5. [PubMed]
- Hardwell A, Barber V, Hargadon T, et al. Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J 2011;20:92-6. [PubMed]
- Lavorini F, Magnan A, Dubus JC, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008;102:593-604. [PubMed]
- Brocklebank D, Ram F., Wright J, et al. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature. Health Technol Assess 2001;5:1-149. [PubMed]
- Lenney J, Innes JA, Crompton GK. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. Respir Med 2000;94:496-500. [PubMed]
- Ari A. Patient education and adherence to aerosol therapy. Respir Care 2015;60:941-55; discussion 955-7. [PubMed]
- Rubin BK. What does it mean when a patient says, “my asthma medication is not working? Chest 2004;126:972-81. [PubMed]
- Lee JY, Yoo KH, Kim DG, et al. Effects of educational interventions for chronic airway disease on primary care. J Korean Med Sci 2016;31:1069-74. [PubMed]
- Seo JY, Hwang YI, Mun SY, et al. Awareness of COPD in a high risk Korean population. Yonsei Med J 2015;56:362-7. [PubMed]
- Mun SY, Hwang YI, Kim JH, et al. Awareness of chronic obstructive pulmonary disease in current smokers: a nationwide survey. Korean J Intern Med 2015;30:191-7. [PubMed]
- Hwang YI, Kwon OJ, Kim YW, et al. Awareness and impact of COPD in Korea: an epidemiologic insight survey. Tuberc Respir Dis 2011;71:400-7.
- Mohammad Y, Fink-Wagner A, Nonikov D. Assets and needs of respiratory patient organizatioins: differences between developed and developing countries. J Thorac Dis 2013;5:914-8. [PubMed]
- Rhee CK, Kim J, Yoon HK, et al. National course of early COPD. Int J Chron Obstruct Pulmon Dis 2017;12:663-8. [PubMed]


