Risk markers for excess mortality in adults with congenital heart disease: does one size fit all?
Over the past few decades, improved survival in patients with congenital heart disease (CHD), particularly those with severe defects, has given rise to a rapidly growing and aging population of adult survivors with increasingly complex disease (1,2). Nevertheless, mortality rates remain higher than the general population, with patients most commonly succumbing to heart failure and to sudden death of presumed arrhythmic etiology. In a recent issue of the European Heart Journal, Oliver et al. explored factors associated with excess mortality in a cohort of 3,311 adults with CHD followed for a median of 10.5 years in a dedicated referral center (3). They confirmed the observation that overall survival of adults with heterogeneous forms of CHD of varied complexity is lower than the general population. An analysis of clinic registry data allowed for detailed phenotyping, whereas vital status was confirmed by means of a national database. Overall, the cohort appeared generally representative of patients followed by adult CHD referral centers, with 51% of patients having moderate or complex lesions, and 49% simple defects. As expected, the mortality rate was highest in patients with complex CHD, although rates were not significantly different among those with moderate versus simple defects.
Oliver et al. provided helpful insights into higher risk subsets (3). For example, patients with non-reparable lesions died at a younger age than surgically palliated adults with CHD. Reinterventions during adulthood were not associated with reduced survival, implying that candidates for transcatheter or surgical interventions were carefully selected. In a multivariable Cox regression model, the following variables were associated with decreased survival: single ventricle physiology, clinical cyanosis, severe pulmonary outflow tract obstruction, infective endocarditis, severe pulmonary hypertension, more than moderate subaortic atrioventricular valve regurgitation, moderate or severe systemic ventricular dysfunction, moderate or severe subpulmonary ventricular dysfunction, ischemic heart disease, aortic aneurysm (including aortic dissection or rupture) and genetic syndromes. The multivariable model was not over fitted (22 variables for 336 events). Naturally, elements that emerge as independent predictors of mortality are highly dependent on variables considered in the model in the first place. In that regard, factors such as electrocardiographic metrics, Holter data, clinical or inducible ventricular arrhythmias, cardiovascular implantable electronic devices, New York Heart Association functional class, and exercise capacity were not assessed.
From the perspective of a cardiologist caring for adults with CHD, the study provides reassuring data for patients with none of the factors associated with higher risk, since survival of this subgroup was comparable to a reference population (3). The authors noted that late referral to an adult CHD specialist did not compromise survival. This observation, together with a Canadian study that reported superior outcomes in patients cared for by specialized adult CHD centers (4), lends credence to the notion that it is better for general practitioners to refer patients late than never. Early referral should, however, remain the objective. As but one example, in patients with congenitally corrected transposition of the great arteries, delaying referral until systemic ventricular dysfunction is established has been shown to adversely impact survival (5). The proportion of patients in Oliver et al.’s study (3) referred late with such time-sensitive critical issues is difficult to estimate but is likely too small to have had a measurable influence on outcomes.
Although the authors consider factors associated with increased mortality to be synonymous with “risk factors”, the semantics of what constitutes a risk factor remains debated. Beyond the undeniable generality that a risk factor implies that an exposure is statistically associated with an outcome, purists will argue that the term “risk factor” should be reserved for variables that are causally linked to the outcome, exhibit a strong and reproducible association, and are modifiable. Most factors identified by Oliver et al. do meet criteria for this more stringent definition of risk factor. Instead, they qualify as “factors associated with”, “determinants of” or “risk markers”, which generally refer to attributes that are related to an increased probability of disease without implications as to causality, strength of associations, or modifiability.
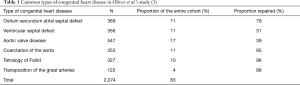
The question inevitably arises as to how results from Oliver et al.’s study could be translated clinically, at a practical level, to individual patients. Careful examination of the study population reveals that 6 underlying lesions constitute 63% of enrolled patients (3). These diagnoses are listed in Table 1 and include tetralogy of Fallot (10%) and transposition of the great arteries (4%), with the latter being the most frequent complex lesion in the cohort and the one associated with the highest risk for sudden cardiac death (6). A concern that is not specific to Oliver et al.’s analysis but plagues studies of heterogeneous populations is the applicability of results generated from a conglomeration of diverse subgroups to risk stratification in individual patients. In the case of CHD, the underlying defect may modify the impact (i.e., so called “effect modifier”) of the association between the purported risk marker and survival. Regression models that lump all forms of CHD together assume that associations between risk markers and outcomes are constant across all subtypes of CHD. There are numerous examples in the literature, some of which are listed in Table 2, which challenge this assumption.

Full table
When effect modification is present, computing an overall estimate of association can be misleading. For example, in patients with aortic valve disease, which constitute 17% of Oliver et al.’s cohort (3), risk markers for those with bicuspid aortic valves generally reflect valve function whereas factors associated with mortality in young adults with mechanical aortic valves relate to their global health (Table 2) (10-12). Age at repair can be a risk marker in patients with surgically corrected CHD, such as aortic coarctation (13), but is not applicable to those with unrepaired CHD. Inducible ventricular tachycardia is an important risk marker in tetralogy of Fallot but not in transposition of the great arteries (15,17). Prognostic determinants in patients with Mustard or Senning baffles (16) may not be transposable to patients with an arterial switch operation (3). Genetic syndromes are themselves highly diverse and subject to effect modification. For example, among genetic syndromes associated with aortopathies, Marfan syndrome (about 170 per 100,000 patient-years) and Turner syndrome (about 36 per 100,000 patients-years) do not carry the same risk for aortic dissection (18,19).
For more accurate identification of risk markers, one solution to dealing with effect modification is to perform lesion-specific analyses (20). This was addressed in part by Oliver et al.’s online supplement, which presents survival curves separately for individual types of CHD (3). Median age at death was >75 years for simple lesions and uncomplicated left-to-right shunts, 60 to 75 years for subvalvular aortic stenosis, Ebstein anomaly, aortic coarctation, tetralogy of Fallot, and complete transposition of the great arteries, and <60 years for Eisenmenger syndrome, atrioventricular discordance, pulmonary atresia, and single ventricle physiology (3). Standardized mortality ratios (i.e., the ratio of observed deaths in the study group to expected deaths in the general population) were computed for individual lesions. Just as survival is clearly impacted by type of CHD, so too are associated risk markers.
Another important issue in assessing survival in adults with CHD is so-called immortal-time bias. “Immortal-time” refers to a span of time during which it is impossible for the outcome under study to have occurred. In the case of adults with CHD, had death transpired during childhood, patients would not have qualified for entry into the study cohort. It is, therefore, impossible for patients to have died at any time between birth and study enrollment, which occurred at a median age of 22.5 years. Bias can be introduced by assessing survival from the moment of birth [i.e., survival curves begin at age 0 in Oliver et al.’s study (3)] when it is statistically impossible for death to have occurred prior to adulthood. One method to overcome immortal-time bias is to begin time-to-event analyses at study entry as opposed to birth. Cognizant of this potential bias, the authors used right-censored Kaplan-Meier curves with age as the time scale accounting for left truncation (3). It is unclear whether such a strategy is as effective in minimizing immortal-time bias as validated techniques such as the Manel-Byar and landmark methods.
In conclusion, Oliver et al. are to be commended for their important study on factors associated with mortality in adults with heterogeneous forms of CHD (3). The study provides valuable insights into population trends and identifies lower and higher risk subgroups of adults with CHD. General risk markers are proposed that require validation in a lesion-specific fashion, considering that the impact of exposures on mortality is substantially modified by type of CHD. Large disease-specific cohort studies that ideally begin at birth and follow patients throughout their childhood and adult lives would shed further light on determinants of risk and inform risk stratification strategies.
Acknowledgements
Dr. P Khairy is supported by a research chair in electrophysiology and congenital heart disease.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Khairy P, Ionescu-Ittu R, Mackie AS, et al. Changing mortality in congenital heart disease. J Am Coll Cardiol 2010;56:1149-57. [Crossref] [PubMed]
- Ávila P, Mercier LA, Dore A, et al. Adult congenital heart disease: a growing epidemic. Can J Cardiol 2014;30:S410-9. [Crossref] [PubMed]
- Oliver JM, Gallego P, Gonzalez AE, et al. Risk factors for excess mortality in adults with congenital heart diseases. Eur Heart J 2017;38:1233-41. [PubMed]
- Mylotte D, Pilote L, Ionescu-Ittu R, et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation 2014;129:1804-12. [Crossref] [PubMed]
- Beauchesne LM, Warnes CA, Connolly HM, et al. Outcome of the unoperated adult who presents with congenitally corrected transposition of the great arteries. J Am Coll Cardiol 2002;40:285-90. [Crossref] [PubMed]
- Gallego P, Gonzalez AE, Sanchez-Recalde A, et al. Incidence and predictors of sudden cardiac arrest in adults with congenital heart defects repaired before adult life. Am J Cardiol 2012;110:109-17. [Crossref] [PubMed]
- Murphy JG, Gersh BJ, McGoon MD, et al. Long-term outcome after surgical repair of isolated atrial septal defect. Follow-up at 27 to 32 years. N Engl J Med 1990;323:1645-50. [Crossref] [PubMed]
- Kim HR, Jung SH, Park JJ, et al. Risk Analysis of the Long-Term Outcomes of the Surgical Closure of Secundum Atrial Septal Defects. Korean J Thorac Cardiovasc Surg 2017;50:78-85. [Crossref] [PubMed]
- Kidd L, Driscoll DJ, Gersony WM, et al. Second natural history study of congenital heart defects. Results of treatment of patients with ventricular septal defects. Circulation 1993;87:I38-51. [PubMed]
- Michelena HI, Desjardins VA, Avierinos JF, et al. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Circulation 2008;117:2776-84. [Crossref] [PubMed]
- Tzemos N, Therrien J, Yip J, et al. Outcomes in adults with bicuspid aortic valves. JAMA 2008;300:1317-25. [Crossref] [PubMed]
- Bouhout I, Stevens LM, Mazine A, et al. Long-term outcomes after elective isolated mechanical aortic valve replacement in young adults. J Thorac Cardiovasc Surg 2014;148:1341-6.e1. [Crossref] [PubMed]
- Brown ML, Burkhart HM, Connolly HM, et al. Coarctation of the aorta: lifelong surveillance is mandatory following surgical repair. J Am Coll Cardiol 2013;62:1020-5. [Crossref] [PubMed]
- Valente AM, Gauvreau K, Assenza GE, et al. Contemporary predictors of death and sustained ventricular tachycardia in patients with repaired tetralogy of Fallot enrolled in the INDICATOR cohort. Heart 2014;100:247-53. [Crossref] [PubMed]
- Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation 2008;117:363-70. [Crossref] [PubMed]
- Vejlstrup N, Sorensen K, Mattsson E, et al. Long-Term Outcome of Mustard/Senning Correction for Transposition of the Great Arteries in Sweden and Denmark. Circulation 2015;132:633-8. [Crossref] [PubMed]
- Khairy P, Van Hare GF, Balaji S, et al. PACES/HRS Expert consensus statement on the recognition and management of arrhythmias in adult congenital heart disease: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology (ACC), the American Heart Association (AHA), the European Heart Rhythm Association (EHRA), the Canadian Heart Rhythm Society (CHRS), and the International Society for Adult Congenital Heart Disease (ISACHD). Heart Rhythm 2014;11:e102-65. [Crossref] [PubMed]
- Gravholt CH, Landin-Wilhelmsen K, Stochholm K, et al. Clinical and epidemiological description of aortic dissection in Turner's syndrome. Cardiol Young 2006;16:430-6. [Crossref] [PubMed]
- Jondeau G, Detaint D, Tubach F, et al. Aortic event rate in the Marfan population: a cohort study. Circulation 2012;125:226-32. [Crossref] [PubMed]
- Khairy P. Ventricular arrhythmias and sudden cardiac death in adults with congenital heart disease. Heart 2016;102:1703-9. [Crossref] [PubMed]